Spinal fusion
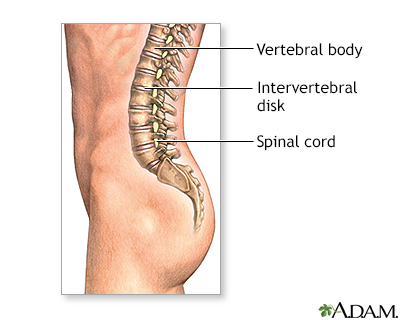
Vertebral interbody fusion; Posterior spinal fusion; Arthrodesis; Anterior spinal fusion; Spine surgery - spinal fusion; Low back pain - fusion; Herniated disk - fusion; Spinal stenosis - fusion; Laminectomy - fusion; Cervical spinal fusion; Lumbar spinal fusionSpinal fusion is surgery to permanently join together two or more bones in the spine so there is no movement between them. These bones are called vertebrae.
Description
You'll be given general anesthesia, which puts you into a deep sleep so you do not feel pain during surgery.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
Read Article Now Book Mark ArticleThe surgeon will make a surgical cut (incision) to view the spine. Other surgery, such as a diskectomy, laminectomy, or a foraminotomy, is almost always done first. Spinal fusion may be done:
Diskectomy
Diskectomy is surgery to remove all or part of the cushion that helps support part of your spinal column. These cushions are called disks, and they ...

Laminectomy
Laminectomy is surgery to remove the lamina. This is part of the bone that makes up a vertebra in the spine. Laminectomy may also be done to remove...
Read Article Now Book Mark ArticleForaminotomy
Foraminotomy is surgery that widens the opening (the foramen) in your spine where nerve roots leave your spinal canal. You may have a narrowing of t...
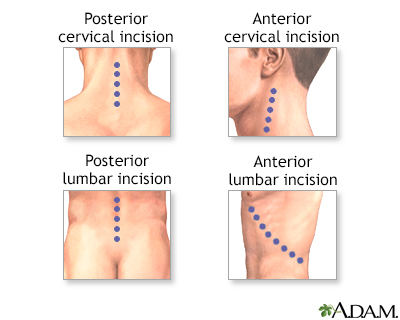
Read Article Now Book Mark Article- On the part of your back or neck over the spine. You may be lying face down. Muscles and tissue will be separated to expose the spine.
- On your side, if you are having surgery on your lower back. The surgeon will use tools called retractors to gently separate, hold the soft tissues such as your bowels and blood vessels apart, and have room to work.
- With a cut on the front of the neck, toward the side.
The surgeon will use a graft (such as bone) to hold (or fuse) the bones together permanently. There are several ways of fusing vertebrae together:
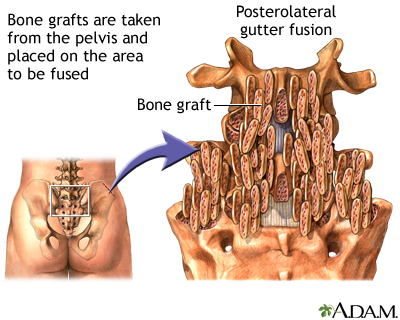
- Strips of bone graft material may be placed over the back part of the spine.
Bone graft material
A bone graft is surgery to place new bone or bone substitutes into spaces around a broken bone or bone defects to stimulate healing.
 ImageRead Article Now Book Mark Article
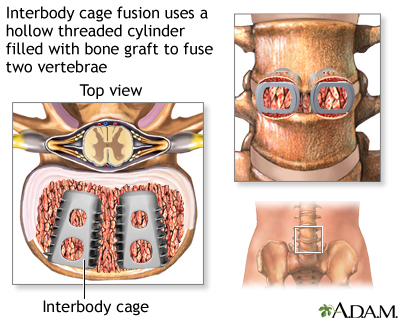
ImageRead Article Now Book Mark Article - Bone graft material may be placed between the vertebrae.
- Special cages may be placed between the vertebrae. These implantable cages are packed with bone graft material.
The surgeon may get the bone graft from:
- Another part of your body (usually around your pelvic bone). This is called an autograft. Your surgeon will make a small cut over your pelvic bone and remove some bone from the back of the rim of the pelvis.
- A bone bank. This is called an allograft which is bone taken from other people that has been cleaned and preserved.
- An artificial bone substitute and growth factors.
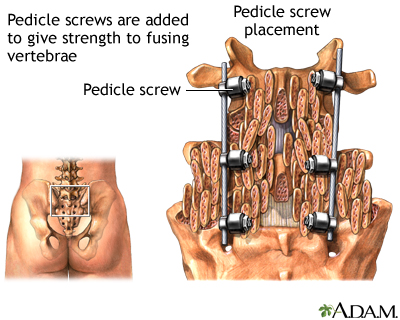
The vertebrae may also be fixed together with rods, screws, plates, or cages. They are used to keep the vertebrae from moving until the bone grafts are fully healed.
Surgery can take 3 to 4 hours.
Why the Procedure Is Performed
Spinal fusion is most often done along with other surgical procedures of the spine. It may be done:
- With other surgical procedures for spinal stenosis, such as foraminotomy or laminectomy
Spinal stenosis
Spinal stenosis is narrowing of the spinal column that causes pressure on the spinal cord, or narrowing of the openings (called neural foramina) wher...
 ImageRead Article Now Book Mark Article
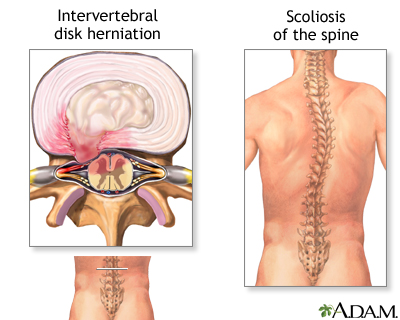
ImageRead Article Now Book Mark Article - After diskectomy in the neck
Spinal fusion may be done if you have:
- Injury or fractures to the bones in the spine
- Weak or unstable spine caused by infections or tumors
- Spondylolisthesis, a condition in which one vertebrae slips forward on top of another
Spondylolisthesis
Spondylolisthesis is a condition in which a bone (vertebra) in the spine moves forward, out of its proper position, in relation to the bone below it....
Read Article Now Book Mark Article - Abnormal curvatures, such as those from scoliosis or kyphosis
Scoliosis
Scoliosis is an abnormal curving of the spine. Your spine is your backbone. It runs straight down your back. Everyone's spine naturally curves a b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleKyphosis
Kyphosis is a curving of the spine that causes a bowing or rounding of the back. This leads to a hunchback or slouching posture.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Arthritis in the spine, such as spinal stenosis
You and your surgeon can decide when you need to have surgery.
Risks
Risks for anesthesia and surgery in general include:
- Reactions to medicines, breathing problems
Breathing problems
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bleeding, blood clots, infection
Blood clots
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks for this surgery include:
- Infection in the wound or vertebral bones
- Damage to a spinal nerve, causing weakness, pain, loss of sensation, problems with your bowels or bladder
- The vertebrae above and below the fusion are more likely to wear away, leading to more problems later
- Leakage of spinal fluid that may require more surgery
- Headaches
Before the Procedure
Tell your surgeon what medicines you are taking. These include medicines, herbs, and supplements you bought without a prescription.
During the days before the surgery:
- Prepare your home for when you leave the hospital.
- If you are a smoker, you need to stop. People who have spinal fusion and continue to smoke may not heal as well. Ask your surgeon or health care provider for help.
You need to stop
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleNot heal
Quitting smoking and other nicotine products, including e-cigarettes, before surgery can improve your recovery and outcome after surgery. Most people...
Read Article Now Book Mark Article - Two weeks before surgery, your surgeon may ask you to stop taking medicines that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and other medicines like these.
- If you have diabetes, heart disease, or other medical problems, your surgeon will ask you to see your regular provider.
Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Talk with your surgeon or provider if you have been drinking a lot of alcohol.
- Ask your surgeon which medicines you should still take on the day of the surgery.
- Let your surgeon know about any cold, flu, fever, herpes breakout, or other illnesses you may have.
On the day of the surgery:
- Follow instructions about not drinking or eating anything before the procedure.
- Take the medicines you were told to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
You may stay in the hospital for up to 3 to 4 days after surgery.
You will receive pain medicines in the hospital. You may take pain medicine by mouth or have a shot or an intravenous line (IV). You may have a pump that allows you to control how much pain medicine you get.
You will be taught how to move properly and how to sit, stand, and walk. You will be told to use a "log-rolling" technique when getting out of bed. This means that you move your entire body at once, without twisting your spine.
You may not be able to eat regular food for 2 to 3 days. You will be given nutrients through an IV and will also eat softer food. When you leave the hospital, you may need to wear a back brace or cast.
Your surgeon will tell you how to take care of yourself at home after spine surgery. Follow instructions on how to take care of your back at home.
Take care of yourself at home after spi...
You were in the hospital for spine surgery. You probably had a problem with one or more disks or spine bones. A disk is a cushion that separates th...

Take care of your back at home
Low back pain refers to pain that you feel in your lower back. You may also have back stiffness, decreased movement of the lower back, and difficult...

Outlook (Prognosis)
Surgery does not always improve pain, and in some cases, can make it worse. However, in some people, surgery can be effective for severe pain that does not get better with other treatments.
If you had chronic back pain before surgery, you will likely still have some pain afterward. Spinal fusion is unlikely to take away all your pain and other symptoms.
Chronic back pain
Low back pain refers to pain that you feel in your lower back. You may also have back stiffness, decreased movement of the lower back, and difficult...

It is hard to predict which people will improve and how much relief surgery will provide, even when using MRI scans or other tests.
Losing weight and getting exercise increase your chances of feeling better.
Future spine problems are possible after spine surgery. After spinal fusion, the area that was fused together can no longer move. Therefore, the spinal column above and below the fusion are more likely to be stressed when the spine moves, and may cause problems later on.
References
Dru AB, Vaziri S, Polifka AJ, Ghogawala Z, Hoh DJ. Indications for spine fusion for axial pain. In: Steinmetz MP, Berven SH, Benzel EC, eds. Benzel's Spine Surgery: Techniques, Complication Avoidance, and Management. 5th ed. Philadelphia, PA: Elsevier; 2022:chap 135.
Gardocki RJ, Park AL. Degenerative disorders of the thoracic and lumbar spine. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 39.
Wang JC, Dailey AT, Mummaneni PV, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2014;21(1):48-53. PMID: 24980585 pubmed.ncbi.nlm.nih.gov/24980585/.
Scoliosis - illustration
Abnormal curvature in the spine is known as scoliosis, and generally begins just at the onset of puberty and progresses during the period of rapid growth. Most junior high schools routinely screen for scoliosis because, if caught early, progressive spine curvature can be prevented. Scoliosis affects girls much more frequently than boys.
Scoliosis
illustration
Spinal fusion - series - Normal anatomy
Presentation
Scoliosis - illustration
Abnormal curvature in the spine is known as scoliosis, and generally begins just at the onset of puberty and progresses during the period of rapid growth. Most junior high schools routinely screen for scoliosis because, if caught early, progressive spine curvature can be prevented. Scoliosis affects girls much more frequently than boys.
Scoliosis
illustration
Spinal fusion - series - Normal anatomy
Presentation
Review Date: 8/12/2023
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.