Rh incompatibility
Rh-induced hemolytic disease of the newborn; Erythroblastosis fetalisRh incompatibility is a condition that develops when a pregnant woman has Rh-negative blood and the baby in her womb has Rh-positive blood.
Causes
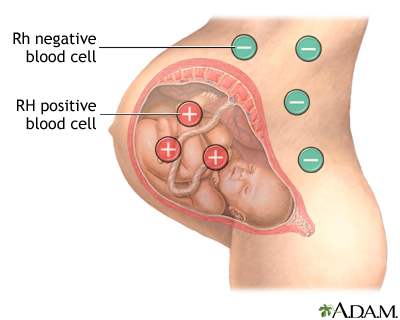
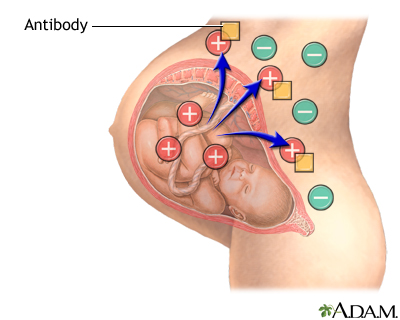
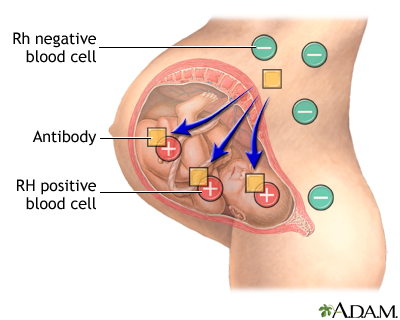
During pregnancy, red blood cells from the unborn baby can cross into the mother's blood through the placenta.
If the mother is Rh-negative, her immune system treats Rh-positive fetal cells as if they were a foreign substance. The mother's body makes antibodies against the fetal blood cells. These antibodies may cross back through the placenta into the developing baby. They destroy the baby's circulating red blood cells.
Antibodies
An antibody is a protein produced by the body's immune system when it detects harmful substances, called antigens. Examples of antigens include micr...

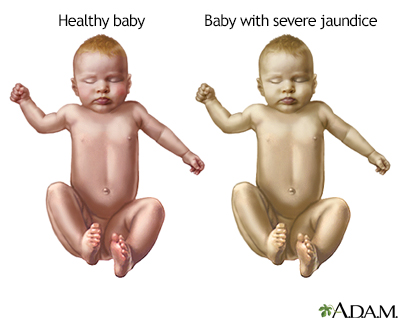
When red blood cells are broken down, they make bilirubin. This causes an infant to become yellow (jaundiced). The level of bilirubin in the infant's blood may range from mild to dangerously high.
Bilirubin
The bilirubin blood test measures the level of bilirubin in the blood. Bilirubin is a yellowish pigment found in bile, a fluid made by the liver. Bi...

Jaundiced
Jaundice is a yellow color of the skin, mucus membranes, or eyes. The yellow coloring comes from bilirubin, a byproduct of old red blood cells. Jau...

Firstborn infants are often not affected unless the mother had past miscarriages or abortions. This would sensitize her immune system. This is because it takes time for the mother to develop antibodies. All children she has later who are also Rh-positive may be affected.
Rh incompatibility develops only when the mother is Rh-negative and the infant is Rh-positive. This problem has become less common in places that provide good prenatal care. This is because special immune globulins called RhoGAM are routinely used.
Symptoms
Rh incompatibility can cause symptoms ranging from very mild to deadly. In its mildest form, Rh incompatibility causes the destruction of red blood cells. There are no other effects.
After birth, the infant may have:
- Yellowing of the skin and whites of the eyes
- Low muscle tone (hypotonia) and lethargy
Exams and Tests
Before delivery, the mother may have more amniotic fluid around her unborn baby (polyhydramnios).
Polyhydramnios
Polyhydramnios occurs when too much amniotic fluid builds up during pregnancy. It is also called amniotic fluid disorder, or hydramnios.

There may be:
-
A positive direct Coombs test result
Coombs test
The Coombs test looks for antibodies that may stick to your red blood cells and cause red blood cells to die too early.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Higher-than-normal levels of bilirubin in the baby's umbilical cord blood
- Signs of red blood cell destruction in the infant's blood
Treatment
Rh incompatibility can be prevented with the use of RhoGAM. Therefore, prevention remains the best treatment. Treatment of an infant who is already affected depends on the severity of the condition.
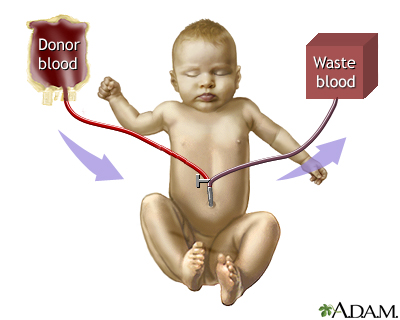
Infants with mild Rh incompatibility may be treated with phototherapy using bilirubin lights. Intravenous (IV) immune globulin may also be used. For infants severely affected, an exchange transfusion of blood may be needed. This is to decrease the levels of bilirubin in the blood.
Bilirubin lights
Bili lights are a type of light therapy (phototherapy) that is used to treat newborn jaundice. Jaundice is a yellow coloring of the skin and eyes. ...

Intravenous
Intravenous means "within a vein. " Most often it refers to giving medicines or fluids through a needle or tube inserted into a vein. This allows th...
Read Article Now Book Mark ArticleOutlook (Prognosis)
Full recovery is expected for mild Rh incompatibility.
Possible Complications
Complications may include:
- Brain damage due to high levels of bilirubin (kernicterus)
Kernicterus
Bilirubin encephalopathy is a rare neurological condition that occurs in some newborns with severe jaundice.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fluid buildup and swelling in the baby (hydrops fetalis)
Hydrops fetalis
Hydrops fetalis is a serious condition. It occurs when abnormal amounts of fluid build up in two or more body areas of a fetus or newborn. It is a ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Problems with mental function, movement, hearing, speech, and seizures
Seizures
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Contact your health care provider if you think or know you are pregnant and have not yet seen a provider.
Prevention
Rh incompatibility is almost completely preventable. Rh-negative mothers should be followed closely by their providers during pregnancy.
Special immune globulins, called RhoGAM, are now used to prevent RH incompatibility in mothers who are Rh-negative.
If the father of the infant is Rh-positive or if his blood type is not known, the mother is given an injection of RhoGAM during the second trimester. If the baby is Rh-positive, the mother will get a second injection within a few days after delivery.
These injections prevent the development of antibodies against Rh-positive blood. However, women with Rh-negative blood type must get injections:
- During every pregnancy
- After a miscarriage or abortion
- After prenatal tests such as amniocentesis and chorionic villus biopsy
Amniocentesis
Amniocentesis is a test that can be done during pregnancy to look for certain problems in the developing baby. These problems include:Birth defectsG...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleChorionic villus biopsy
Chorionic villus sampling (CVS) is a test some pregnant women have to screen their baby for genetic problems.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - After injury to the abdomen during pregnancy
References
Kaplan M, Wong RJ, Bensen R, Sibley E, Stevenson DK. Neonatal jaundice and liver disease. In: Martin RJ, Fanaroff AA, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 95.
Moise KJ. Red cell alloimmunization. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 40.
Thom CS, Lambert MP. Blood disorders. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 138.
-
Erythroblastosis fetalis - photomicrograph - illustration
Antibodies from an Rh negative mother may enter the blood stream of her unborn Rh positive infant, damaging the red blood cells (RBCs). The infant responds by increasing RBC production and sending out immature RBCs that still have nuclei. This photograph shows normal RBCs, damaged RBCs, and immature RBCs that still contain nuclei.
Erythroblastosis fetalis - photomicrograph
illustration
-
Jaundiced infant - illustration
Newborn jaundice (producing yellow skin) can have many causes, but the majority of these infants have a condition called physiological jaundice, a natural occurrence in the newborn due to the immature liver. This type of jaundice is short term, generally lasting only a few days. Jaundice should be evaluated by a physician until decreasing or normal levels of bilirubin are measured in the blood.
Jaundiced infant
illustration
-
Antibodies - illustration
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Antibodies
illustration
-
Exchange transfusion - series
Presentation
-
Rh incompatibility - series
Presentation
-
Erythroblastosis fetalis - photomicrograph - illustration
Antibodies from an Rh negative mother may enter the blood stream of her unborn Rh positive infant, damaging the red blood cells (RBCs). The infant responds by increasing RBC production and sending out immature RBCs that still have nuclei. This photograph shows normal RBCs, damaged RBCs, and immature RBCs that still contain nuclei.
Erythroblastosis fetalis - photomicrograph
illustration
-
Jaundiced infant - illustration
Newborn jaundice (producing yellow skin) can have many causes, but the majority of these infants have a condition called physiological jaundice, a natural occurrence in the newborn due to the immature liver. This type of jaundice is short term, generally lasting only a few days. Jaundice should be evaluated by a physician until decreasing or normal levels of bilirubin are measured in the blood.
Jaundiced infant
illustration
-
Antibodies - illustration
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Antibodies
illustration
-
Exchange transfusion - series
Presentation
-
Rh incompatibility - series
Presentation
Review Date: 1/1/2025
Reviewed By: Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.