Myotonia congenita
Thomsen's disease; Becker's diseaseMyotonia congenita is an inherited condition that affects muscle relaxation. It is congenital, meaning that it is present from birth. It occurs more frequently in northern Scandinavia.
Causes
Myotonia congenita is caused by a genetic change (genetic variant). It is passed down from either one or both parents to their children (inherited).
Myotonia congenita is caused by a problem in the part of the muscle cells that are needed for muscles to relax. Abnormal repeated electrical signals occur in the muscles, causing a type of muscle stiffness called myotonia.
Symptoms
The hallmark of this condition is myotonia. This means the muscles are unable to quickly relax after contracting. For example, after a handshake, the person is only very slowly able to open and pull away their hand.
Early symptoms may include:
- Difficulty swallowing
- Gagging
- Stiff movements that improve when they are repeated
- Shortness of breath or tightening of the chest at the beginning of exercise
- Frequent falls
- Difficulty opening eyes after forcing them closed or crying
Children with myotonia congenita often look muscular and well-developed. They may not have symptoms of myotonia congenita until age 2 or 3.
Exams and Tests
Your health care provider may ask if there is a family history of myotonia congenita.
Tests include:
- Electromyography (EMG) and nerve conduction studies (NCS)
Electromyography
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleNerve conduction studies
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve. This test is done along with electromyography (EM...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genetic testing
- Muscle biopsy
Muscle biopsy
A muscle biopsy is the removal of a small piece of muscle tissue for examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
As cold and stress can worsen symptoms, management is first directed at avoiding these potential triggers. Some forms of exercise may also be beneficial. Mexiletine is a medicine that treats symptoms of myotonia congenita. Other treatments include:
- Phenytoin
- Procainamide
- Quinine (rarely used now, due to side effects)
- Carbamazepine
Support Groups
The following resources can provide more information on myotonia congenita:
- Muscular Dystrophy Association -- www.mda.org/disease/myotonia-congenita
- National Library of Medicine, Medline Plus -- medlineplus.gov/genetics/condition/myotonia-congenita/
Outlook (Prognosis)
People with this condition can do well. Symptoms only occur when a movement is first started. After a few repetitions, the muscle relaxes and the movement becomes normal.
Possible Complications
Complications may include:
- Aspiration pneumonia caused by swallowing difficulties
Aspiration pneumonia
Pneumonia is inflammation (swelling) and infection of the lungs or large airways. Aspiration pneumonia occurs when food or liquid is breathed into th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Frequent choking, gagging, or trouble swallowing in an infant
- Long-term (chronic) joint problems
- Weakness of the abdominal muscles
When to Contact a Medical Professional
Contact your provider if your child has symptoms of myotonia congenita.
Prevention
Couples who want to have children and who have a family history of myotonia congenita should consider genetic counseling.
Genetic counseling
Genetics is the study of heredity, the process of a parent passing certain genes on to their children. A person's appearance, such as height, hair co...

References
Bryan ES, Alsaleem M. Myotonia congenita. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Updated August 28, 2023. PMID: 32966006 www.ncbi.nlm.nih.gov/books/NBK562335/.
Kang MK, Kerchner GA, Ptácek LJ. Channelopathies: episodic and electrical disorders of the nervous system. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 98.
Manzur AY. Muscular dystrophies. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 649.
Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389.
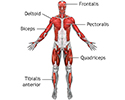
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
Deep anterior muscles - illustration
Muscle tissue is composed primarily of contractile cells. Contractile cells have the ability to produce movement.
Deep anterior muscles
illustration
Tendons and muscles - illustration
Tendons connect muscles to their bony origins and insertions.
Tendons and muscles
illustration
Lower leg muscles - illustration
The muscular components of the lower leg include the gastrocnemius, soleus, peroneus longus, tibialis anterior, extensor digitorum longus, and the Achilles tendon.
Lower leg muscles
illustration
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
Deep anterior muscles - illustration
Muscle tissue is composed primarily of contractile cells. Contractile cells have the ability to produce movement.
Deep anterior muscles
illustration
Tendons and muscles - illustration
Tendons connect muscles to their bony origins and insertions.
Tendons and muscles
illustration
Lower leg muscles - illustration
The muscular components of the lower leg include the gastrocnemius, soleus, peroneus longus, tibialis anterior, extensor digitorum longus, and the Achilles tendon.
Lower leg muscles
illustration
Review Date: 3/31/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.