Epididymitis
Epididymitis is swelling (inflammation) of the tube that connects the testicle with the vas deferens. The tube is called the epididymis.
Causes
Epididymitis is most common in men ages 19 to 35. It is most often caused by a bacterial infection. Infection often begins in the urethra, the prostate, or the bladder. Gonorrhea and chlamydia infections are most often the cause of the problem in young heterosexual men. In children and older men, it is more commonly caused by E coli and similar bacteria. This is also true in men who have sex with men.
Gonorrhea
Gonorrhea is a common sexually transmitted infection (STI).
Read Article Now Book Mark ArticleChlamydia
Chlamydia is an infection caused by the bacteria Chlamydia trachomatis. It is most often spread through sexual contact.

Mycobacterium tuberculosis (TB) can cause epididymitis. Other bacteria (such as Ureaplasma) may also cause the condition.
Amiodarone is a medicine which prevents abnormal heart rhythms. This medicine can also cause epididymitis.
The following increase the risk for epididymitis:
- Recent surgery
- Past structural problems in the urinary tract
- Regular use of a urethral catheter
Catheter
A urinary catheter is a tube placed in the body to drain and collect urine from the bladder.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sexual intercourse with more than one partner and not using condoms
-
Enlarged prostate
Enlarged prostate
The prostate is a gland that produces some of the fluid that carries sperm during ejaculation. The prostate gland surrounds the urethra, the tube th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Epididymitis may begin with:
- Low fever
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chills
- Feeling of heaviness in the testicle area
The testicle area will get more sensitive to pressure. It will become painful as the condition progresses. An infection in the epididymis can easily spread to the testicle.
Other symptoms include:
-
Blood in the semen
Blood in the semen
Blood in the semen is called hematospermia. It may be in amounts too small to be seen except with a microscope, or it may be visible in the ejaculat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Discharge from the urethra (the opening at the end of the penis)
- Discomfort in the lower abdomen or pelvis
- Lump near the testicle
Less common symptoms are:
- Pain during ejaculation
- Pain or burning during urination
- Painful scrotal swelling (epididymis is enlarged)
Scrotal swelling
Scrotal swelling is abnormal enlargement of the scrotum. This is the name for the sac surrounding the testicles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tender, swollen, and painful groin area on affected side
-
Testicle pain that gets worse during a bowel movement
Testicle pain
Testicle pain is discomfort in one or both testicles. The pain can spread into the lower abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms of epididymitis may be similar to those of testicular torsion, which requires emergent treatment.
Testicular torsion
Testicular torsion is twisting of the spermatic cord, which supports the testes in the scrotum. When this occurs, blood supply is cut off to the tes...

Exams and Tests
Physical exam will show a red, tender lump on the affected side of the scrotum. You may have tenderness in a small area of the testicle where the epididymis is attached. A large area of swelling may develop around the lump.
The lymph nodes in the groin area may be enlarged. There may also be discharge from the penis. A rectal exam may show an enlarged or tender prostate.
These tests may be performed:
-
Complete blood count (CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Doppler ultrasound
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Testicular scan (nuclear medicine scan)
-
Urinalysis and culture (you may need to give several specimens, including initial stream, mid-stream, and after a prostate massage)
Urinalysis
Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tests for chlamydia and gonorrhea
Treatment
Your health care provider will prescribe medicine to treat the infection. Sexually transmitted infections need antibiotics. Your sexual partners should also be treated. You may need pain medicines and anti-inflammatory medicines.
If you are taking amiodarone, you may need to lower your dose or change your medicine. Talk with your provider.
To ease discomfort:
- Rest lying down with the scrotum elevated.
Scrotum
The scrotum is a part of a male's body that is located below the penis. The scrotum is the sac (pouch) that contains the testes, epididymis, and the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Apply ice packs to the painful area (but do not apply ice directly to the area).
- Wear underwear with more support or an athletic supporter.
You will need to follow-up with your provider to make sure the infection has cleared completely.
Outlook (Prognosis)
Epididymitis most often gets better with antibiotic treatment. There are no long-term sexual or reproductive problems in most cases. However, the condition may return.
Possible Complications
Complications include:
-
Abscess in the scrotum
Abscess
An abscess is a collection of pus in any part of the body. In most cases, the area around an abscess is swollen and inflamed.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Long-term (chronic) epididymitis
- Opening on the skin of the scrotum
- Death of testicular tissue due to lack of blood (testicular infarction)
-
Infertility
Infertility
Infertility means you cannot get pregnant (conceive). There are 2 types of infertility:Primary infertility refers to couples who have not become preg...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Sudden and severe pain in the scrotum is a medical emergency. You need to be seen by a provider right away.
When to Contact a Medical Professional
Contact your provider if you have symptoms of epididymitis. Go to the emergency room or call 911 or the local emergency number if you have sudden, severe testicle pain or pain after an injury.
Prevention
You can prevent complications if you get diagnosed and treated early.
Your provider may prescribe antibiotics before a surgery. This is because some surgeries could raise the risk for epididymitis. Practice safe sex. Avoid multiple sexual partners and use condoms. This may help prevent epididymitis caused by sexually transmitted diseases.
Safe sex
Safe sex means taking steps before and during sex that can prevent you from getting an infection, or from giving an infection to your partner. These...

References
Pontari M. Inflammatory and pain conditions of the male genitourinary tract: prostatitis and related pain conditions, orchitis, and epididymitis. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 56.
Reno HEL, Geisler WM. Diseases caused by chlamydiae. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 294.
-
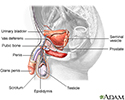
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
Blood in semen - illustration
The presence of blood in semen (the fluid discharged upon ejaculation) may be caused by inflammation, infection, obstruction or trauma.
Blood in semen
illustration
-
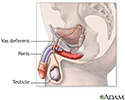
Pathway of sperm - illustration
The testes are where sperm are manufactured in the scrotum. The epididymis is a tortuously coiled structure topping the testis, and it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the deferent duct. Sperm then travels through the deferent duct through up the spermatic cord into the pelvic cavity, over the ureter to the prostate behind the bladder. Here, the vas deferens joins with the seminal vesicle to form the ejaculatory duct, which passes through the prostate and empties into the urethra. When ejaculation occurs, rhythmic muscle movements propel the sperm forward.
Pathway of sperm
illustration
-
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
-
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
Blood in semen - illustration
The presence of blood in semen (the fluid discharged upon ejaculation) may be caused by inflammation, infection, obstruction or trauma.
Blood in semen
illustration
-
Pathway of sperm - illustration
The testes are where sperm are manufactured in the scrotum. The epididymis is a tortuously coiled structure topping the testis, and it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the deferent duct. Sperm then travels through the deferent duct through up the spermatic cord into the pelvic cavity, over the ureter to the prostate behind the bladder. Here, the vas deferens joins with the seminal vesicle to form the ejaculatory duct, which passes through the prostate and empties into the urethra. When ejaculation occurs, rhythmic muscle movements propel the sperm forward.
Pathway of sperm
illustration
-
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
Review Date: 9/2/2024
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.