Muscular dystrophy
Inherited myopathy; MDMuscular dystrophy (MD) is a group of inherited disorders that cause muscle weakness and loss of muscle tissue, which get worse over time.
Muscle weakness
Weakness is reduced strength in one or more muscles.

Causes
Inherited conditions are passed down through families. They may become manifest in childhood or adulthood. There are many different types of MD. They include:
- Becker muscular dystrophy
Becker muscular dystrophy
Becker muscular dystrophy is an inherited disorder that involves slowly worsening muscle weakness of the legs and pelvis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Duchenne muscular dystrophy
Duchenne muscular dystrophy
Duchenne muscular dystrophy is an inherited disorder. It involves muscle weakness, which quickly gets worse.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Emery-Dreifuss muscular dystrophy
- Facioscapulohumeral muscular dystrophy
Facioscapulohumeral muscular dystrophy
Facioscapulohumeral muscular dystrophy is a condition that causes muscle weakness and loss of muscle tissue that gets worse over time.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Limb-girdle muscular dystrophy
Limb-girdle muscular dystrophy
Limb-girdle muscular dystrophies include at least 33 different inherited diseases. These disorders first affect the muscles around the shoulder gird...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Oculopharyngeal muscular dystrophy
- Myotonic muscular dystrophy
Symptoms
MD can affect adults, but the more severe forms tend to occur in early childhood.
Symptoms vary among the different types of MD. All of the muscles may be affected. Or, only specific groups of muscles may be affected, such as those around the pelvis, shoulder, or face. The muscle weakness slowly gets worse and symptoms may include:
- Delayed development of muscle motor skills
- Difficulty using one or more muscle groups
- Drooling
- Eyelid drooping (ptosis)
Eyelid drooping
Eyelid drooping is excess sagging of the upper eyelid. The edge of the upper eyelid may be lower than it should be (ptosis) or there may be excess b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Frequent falls
- Loss of strength in a muscle or group of muscles as an adult
- Loss in muscle size
- Problems walking (delayed walking)
Problems walking
Walking abnormalities can be caused by many different types of problems. Problems with the joints, (such as arthritis), bones (such as deformities),...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Muscle contractures
Intellectual disability is present in some types of MD.
Several types of MD affect only males.
Exams and Tests
A physical examination and your medical history will help your health care provider determine the type of MD. Specific muscle groups are affected by different types of MD.
The exam may show:
- Weakness of certain muscles
- Abnormally curved spine (scoliosis)
Scoliosis
Scoliosis is an abnormal curving of the spine. Your spine is your backbone. It runs straight down your back. Everyone's spine naturally curves a b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Joint contractures (clubfoot, claw-hand, or others)
Clubfoot
Clubfoot is a condition that involves both the foot and lower leg in which the foot turns inward and downward. It is a congenital condition, which m...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Low muscle tone (hypotonia)
Some types of MD involve the heart muscle, causing cardiomyopathy or abnormal heart rhythm (arrhythmia).
Cardiomyopathy
Cardiomyopathy is disease in which the heart muscle becomes weakened, stretched, or has another structural problem. It often contributes to the hear...

Arrhythmia
An arrhythmia is a disorder of the heart rate (pulse) or heart rhythm. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregul...

Often, there is a loss of muscle mass (wasting). This may be hard to see because some types of MD cause a buildup of fat and connective tissue that makes the muscle appear larger. This is called pseudohypertrophy.
Wasting
Muscle atrophy is the wasting (thinning) or loss of muscle tissue.

A muscle biopsy may be used to confirm the diagnosis. In some cases, a DNA blood test may be all that is needed.
Muscle biopsy
A muscle biopsy is the removal of a small piece of muscle tissue for examination.

Other tests may include:
- Heart testing -- electrocardiography (ECG)
Electrocardiography
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Nerve testing -- nerve conduction and electromyography (EMG)
Nerve conduction
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve. This test is done along with electromyography (EM...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleElectromyography
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urine and blood testing, including creatine phosphokinase (CPK) level
Creatine phosphokinase
Creatine phosphokinase (CPK) is an enzyme in the body. It is found mainly in the heart, brain, and skeletal muscle. This article discusses the test...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genetic testing for some forms of MD
- Muscle biopsy
Treatment
There are no known cures for the various MDs. Recent advances have led to some gene therapies that are promising for the future. The goal of treatment is to control symptoms.
Physical therapy may help maintain muscle strength and function. Leg braces and a wheelchair can improve mobility and self-care. In some cases, surgery on the spine or legs may help improve function.
Corticosteroids taken by mouth are sometimes prescribed to children with certain MDs to keep them walking for as long as possible.
The person should be as active as possible. No activity at all (such as bedrest) can make the disease worse.
Some people with breathing weakness may benefit from devices to assist breathing.
Support Groups
You can ease the stress of illness by joining a support group where members share common experiences and problems.
Support group
The following organizations are good resources for information on muscular dystrophy:Centers for Disease Control and Prevention -- www. cdc. gov/musc...

Outlook (Prognosis)
The severity of disability depends on the type of MD. All types of MD slowly get worse, but how fast this happens varies widely.
Some types of MD, such as Duchenne muscular dystrophy in boys, are associated with a shortened lifespan. Other types cause little disability and people have a normal lifespan.
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of MD.
- You have a personal or family history of MD and you are planning to have children.
Prevention
Genetic counseling is advised when there is a personal or family history of MD. Women may have no symptoms, but still carry the gene for the disorder. Duchenne muscular dystrophy can be detected with about 95% accuracy by genetic studies done during pregnancy.
Genetic counseling
Shiga-like toxin producing E coli hemolytic-uremic syndrome (STEC-HUS) is a disorder that most often occurs when an infection in the digestive system...

References
Manzur AY. Muscular dystrophies. In: Kliegman RM, St. Geme JW, Blum NJ, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 649.
Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389.
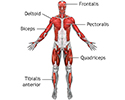
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
Deep anterior muscles - illustration
Muscle tissue is composed primarily of contractile cells. Contractile cells have the ability to produce movement.
Deep anterior muscles
illustration
Tendons and muscles - illustration
Tendons connect muscles to their bony origins and insertions.
Tendons and muscles
illustration
Lower leg muscles - illustration
The muscular components of the lower leg include the gastrocnemius, soleus, peroneus longus, tibialis anterior, extensor digitorum longus, and the Achilles tendon.
Lower leg muscles
illustration
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
Deep anterior muscles - illustration
Muscle tissue is composed primarily of contractile cells. Contractile cells have the ability to produce movement.
Deep anterior muscles
illustration
Tendons and muscles - illustration
Tendons connect muscles to their bony origins and insertions.
Tendons and muscles
illustration
Lower leg muscles - illustration
The muscular components of the lower leg include the gastrocnemius, soleus, peroneus longus, tibialis anterior, extensor digitorum longus, and the Achilles tendon.
Lower leg muscles
illustration
Review Date: 3/31/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.