Uveitis
Iritis; Pars planitis; Choroiditis; Chorioretinitis; Anterior uveitis; Posterior uveitis; IridocyclitisUveitis is swelling and inflammation of the uvea. The uvea is the middle layer of the wall of the eye. The uvea supplies blood for the iris at the front of the eye and the retina in the back of the eye.
Uvea
The uvea is the middle layer of the eye. It lies beneath the white part of the eye (the sclera). It is made of the iris, ciliary body, and choroid....

Retina
The retina is the light-sensitive layer of tissue at the back of the eyeball. Images that come through the eye's lens are focused on the retina. Th...

Causes
Uveitis can be caused by autoimmune disorders. These diseases occur when the body's immune system attacks and destroys healthy body tissue by mistake. Examples are:
Autoimmune disorders
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 autoimmune d...

- Ankylosing spondylitis
Ankylosing spondylitis
Ankylosing spondylitis (AS) is a chronic form of arthritis. It mostly affects the bones and joints at the base of the spine where it connects with t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Behcet disease
- Psoriasis
Psoriasis
Psoriasis is a skin condition that causes skin redness, silvery scales, and irritation. Most people with psoriasis have thick, red, well-defined pat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Reactive arthritis
- Rheumatoid arthritis
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sarcoidosis
Sarcoidosis
Sarcoidosis is a disease in which inflammation occurs in the lymph nodes, lungs, liver, eyes, skin, and/or other tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Ulcerative colitis
Ulcerative colitis
Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Uveitis can also be caused by infections such as:
- AIDS
AIDS
Human immunodeficiency virus (HIV) is the virus that causes acquired immunodeficiency syndrome (AIDS). When a person becomes infected with HIV, the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cytomegalovirus (CMV) retinitis
CMV) retinitis
Cytomegalovirus (CMV) retinitis is a viral infection of the retina of the eye resulting in inflammation.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Herpes zoster infection
Herpes zoster infection
Shingles is a painful, blistering skin rash. It is caused by the varicella-zoster virus, a member of the herpes family of viruses. This is the viru...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Histoplasmosis
Histoplasmosis
Histoplasmosis is an infection that occurs from breathing in the spores of the fungus Histoplasma capsulatum.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Kawasaki disease
Kawasaki disease
Kawasaki disease is a rare condition that involves inflammation of the blood vessels. It occurs in children.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Syphilis
Syphilis
Syphilis is a bacterial infection that is most often spread through sexual contact.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Toxoplasmosis
Toxoplasmosis
Toxoplasmosis is an infection due to the parasite Toxoplasma gondii.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exposure to toxins or injury can also cause uveitis. In many cases, the cause is unknown.
Often the inflammation is limited to only part of the uvea. The most common form of uveitis involves inflammation of the iris, in the front part of the eye. In this case, the condition is called iritis. In most cases, it occurs in healthy people. The disorder may affect only one eye. It is most common in young and middle-aged people.
Posterior uveitis affects the back part of the eye. It involves primarily the choroid. This is the layer of blood vessels and connective tissue in the middle layer of the eye. This type of uveitis is called choroiditis. If the retina is also involved, it is called chorioretinitis.
Another form of uveitis is pars planitis. Inflammation occurs in the area called the pars plana, which is located between the iris and the choroid. Pars planitis most often occurs in young men. It is generally not associated with any other disease. However, it may be linked to Crohn disease and possibly multiple sclerosis.
Symptoms
Uveitis can affect one or both eyes. Symptoms depend on which part of the uvea is inflamed. Symptoms may develop rapidly and can include:
- Blurred vision
Blurred vision
There are many types of eye problems and vision disturbances, such as: Halos Blurred vision (the loss of sharpness of vision and the inability to see...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Dark, floating spots in the vision
- Eye pain
Eye pain
Pain in the eye may be described as a burning, throbbing, aching, or stabbing sensation in or around the eye. It may also feel like you have a forei...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Redness of the eye
Redness of the eye
Eye redness is most often due to swollen or dilated blood vessels. This makes the surface of the eye look red or bloodshot.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sensitivity to light
Sensitivity to light
Photophobia is eye discomfort in bright light.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
The health care provider will take a complete medical history and do an eye exam. Lab tests may be done to rule out infection or a weak immune system.
If you are over age 25 and have pars planitis, your provider will suggest a brain and spine MRI. This will check for multiple sclerosis.
Treatment
Iritis and irido-cyclitis (anterior uveitis) are most often mild. Treatment may involve:
- Dark glasses
- Eye drops that dilate the pupil to relieve pain
- Steroid eye drops
Pars planitis is often treated with steroid eye drops. Other medicines, including steroids taken by mouth, may be used to help suppress the immune system and reduce inflammation.
Posterior uveitis treatment depends on the underlying cause. It almost always includes steroids taken by mouth.
If the uveitis is caused by a body-wide (systemic) infection, you may be given antibiotics. You may also be given powerful anti-inflammatory medicines called corticosteroids. Sometimes certain types of immune-suppressant medicines are used to treat severe uveitis.
Outlook (Prognosis)
With proper treatment, most attacks of anterior uveitis go away in a few days to weeks. However, the problem often returns.
Posterior uveitis may last from months to years. It may cause permanent vision damage, even with treatment.
Possible Complications
Complications may include:
- Cataracts
- Fluid within the retina
- Glaucoma
Glaucoma
Glaucoma is a group of eye conditions that can damage the optic nerve. This nerve sends the images you see to your brain. Most often, optic nerve da...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Irregular pupil
- Retinal detachment
Retinal detachment
Retinal detachment is a separation of the light-sensitive membrane (retina) in the back of the eye from its supporting layers.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Vision loss
Vision loss
There are many types of eye problems and vision disturbances, such as: Halos Blurred vision (the loss of sharpness of vision and the inability to see...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Symptoms that need urgent medical care are:
- Eye pain
- Reduced vision
Prevention
If you have a body-wide (systemic) infection or disease, treating the condition may prevent uveitis.
References
American Academy of Ophthalmology Eye Wiki website. Treatment of uveitis. eyewiki.org/Treatment_of_Uveitis. Updated January 16, 2024. Accessed August 14, 2024.
Cioffi GA, Liebmann JM. Diseases of the visual system. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 391.
Durand ML. Infectious causes of uveitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 115.
Read RW. General approach to the uveitis patient and treatment strategies. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 7.2.
Testi I, Pavesio CE. Uveitis related to HLA-B27 and juvenile idiopathic arthritis-associated uveitis. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 7.13.
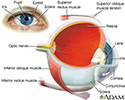
Eye - illustration
The eye is the organ of sight, a nearly spherical hollow globe filled with fluids (humors). The outer layer (sclera, or white of the eye, and cornea) is fibrous and protective. The middle layer (choroid, ciliary body and the iris) is vascular. The innermost layer (retina) is sensory nerve tissue that is light sensitive. The fluids in the eye are divided by the lens into the vitreous humor (behind the lens) and the aqueous humor (in front of the lens). The lens itself is flexible and suspended by ligaments which allow it to change shape to focus light on the retina, which is composed of sensory neurons.
Eye
illustration
Visual field test - illustration
Central and peripheral vision is tested by using visual field tests. Changes may indicate eye diseases, such as glaucoma or retinitis.
Visual field test
illustration
Eye - illustration
The eye is the organ of sight, a nearly spherical hollow globe filled with fluids (humors). The outer layer (sclera, or white of the eye, and cornea) is fibrous and protective. The middle layer (choroid, ciliary body and the iris) is vascular. The innermost layer (retina) is sensory nerve tissue that is light sensitive. The fluids in the eye are divided by the lens into the vitreous humor (behind the lens) and the aqueous humor (in front of the lens). The lens itself is flexible and suspended by ligaments which allow it to change shape to focus light on the retina, which is composed of sensory neurons.
Eye
illustration
Visual field test - illustration
Central and peripheral vision is tested by using visual field tests. Changes may indicate eye diseases, such as glaucoma or retinitis.
Visual field test
illustration
Review Date: 7/9/2024
Reviewed By: Audrey Tai, DO, MS, Athena Eye Care, Mission Viejo, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.