Acoustic neuroma
Vestibular schwannoma; Tumor - acoustic; Cerebellopontine angle tumor; Angle tumor; Hearing loss - acoustic; Tinnitus - acousticAn acoustic neuroma is a slow-growing tumor of the nerve that connects the ear to the brain. This nerve is called the vestibular cochlear nerve. It is behind the ear, right under the brain.
An acoustic neuroma is a benign tumor. This means that it does not spread to other parts of the body. However, it can damage several important nearby nerves as it grows.
Causes
Acoustic neuromas have been linked with the genetic disorder neurofibromatosis type 2 (NF2).
Neurofibromatosis type 2
Neurofibromatosis 2 (NF2) is a disorder in which tumors form on the nerves of the brain and spine (the central nervous system). It may be passed dow...

Acoustic neuromas are uncommon.
Symptoms
The symptoms vary, based on the size and location of the tumor. Because the tumor grows so slowly, symptoms most often start after age 30.
Common symptoms include:
-
Abnormal feeling of movement (vertigo)
Vertigo
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hearing loss in the affected ear that makes it hard to hear conversations
Hearing loss
Hearing loss is being partly or totally unable to hear sound in one or both ears.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ringing (tinnitus) in the affected ear
Tinnitus
Tinnitus is the medical term for "hearing" noises in your ears. It occurs when there is no outside source of the sounds. Tinnitus is often called "r...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Less common symptoms include:
- Difficulty understanding speech
-
Dizziness
Dizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Headache
-
Loss of balance
Loss of balance
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Numbness in the face or one ear
Numbness
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pain in the face or one ear
Pain in the face
Face pain may be dull and throbbing or an intense, stabbing discomfort in the face or forehead. It can occur in one or both sides.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Weakness of the face or facial asymmetry
Exams and Tests
The health care provider may suspect an acoustic neuroma based on your medical history, an exam of your nervous system, or tests.
Often, the physical exam is normal when the tumor is diagnosed. Sometimes, the following signs may be present:
- Decreased feeling on one side of the face
-
Drooping on one side of the face
Drooping
Facial paralysis means that a person is no longer able to move some or all of the muscles on one or both sides of the face.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Unsteady walk
Unsteady walk
Walking abnormalities can be caused by many different types of problems. Problems with the joints, (such as arthritis), bones (such as deformities),...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
The most useful test to identify an acoustic neuroma is an MRI of the brain. Other tests to diagnose the tumor and tell it apart from other causes of dizziness or vertigo include:
MRI of the brain
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...

- Hearing test
- Test of equilibrium and balance (electronystagmography)
Electronystagmography
Electronystagmography is a test that looks at eye movements to see how well nerves in the brain are working. These nerves are:Vestibular nerve (eigh...
Read Article Now Book Mark Article - Test of hearing and brainstem function (brainstem auditory evoked response)
Treatment
Treatment depends on the size and location of the tumor, your age, and your overall health. You and your provider must decide whether to watch the tumor without treatment, use radiation treatment to stop it from growing, or try to remove it.
Many acoustic neuromas are small and grow very slowly. Small tumors with few or no symptoms may be watched for changes, especially in older people. Regular MRI scans will be done.
If not treated, some acoustic neuromas can:
- Damage the nerves involved in hearing and balance
- Place pressure on nearby brain tissue
- Harm the nerves responsible for movement and feeling in the face
- Lead to a buildup of fluid (hydrocephalus) in the brain (with very large tumors)
Hydrocephalus
Hydrocephalus is a buildup of fluid inside the skull that leads to the brain pushing against the skull. Hydrocephalus means "water on the brain. "...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Removing an acoustic neuroma is more commonly done for:
- Larger tumors
- Tumors that are causing symptoms
- Tumors that are growing quickly
- Tumors that are pressing on the brain
Surgery or a type of radiation treatment is done to remove the tumor and prevent other nerve damage. Depending on the type of surgery performed, hearing can sometimes be preserved.
- The surgical technique to remove an acoustic neuroma is called microsurgery. A special microscope and small, precise instruments are used. This technique offers a higher chance of cure.
-
Stereotactic radiosurgery focuses high-powered x-rays on a small area. It is a form of radiation therapy, not a surgical procedure. It may be used to slow down or stop the growth of tumors that are hard to remove with surgery. It may also be done to treat people who are unable to have surgery, such as older adults or people who are very sick.
Stereotactic radiosurgery
Stereotactic radiosurgery (SRS) is a form of radiation therapy that focuses high-power energy on a small area of the body. Despite its name, radiosu...
Read Article Now Book Mark Article
Removing an acoustic neuroma can damage the acoustic or other nerves. This may cause loss of hearing or weakness in the face muscles. This damage is more likely to occur when the tumor is large.
Outlook (Prognosis)
An acoustic neuroma is not cancer. The tumor does not spread to other parts of the body. However, it may continue to grow and press on structures in the skull.
People with small, slow-growing tumors may not need treatment.
Hearing loss present before treatment is not likely to return after surgery or radiosurgery. In cases of smaller tumors, hearing loss that occurs after surgery may return.
Most people with small tumors will have no permanent weakness of the face after surgery. However, people with large tumors are more likely to have some permanent weakness of the face after surgery.
Signs of nerve damage such as loss of hearing or weakness of the face may be delayed after radiosurgery.
In most cases, brain surgery can completely remove the tumor.
When to Contact a Medical Professional
Contact your provider if you have:
- Hearing loss that is sudden or getting worse
- Ringing in one ear
- Dizziness (vertigo)
References
Arriaga MA, Brackmann DE. Neoplasms of the posterior fossa. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 179.
DeAngelis LM. Tumors of the central nervous system. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 180.
Mellinghoff IK, DeAngelis LM. Tumors of the central nervous system. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 175.
-
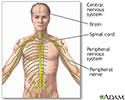
Central nervous system and peripheral nervous system - illustration
The central nervous system comprises the brain and spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
Review Date: 5/2/2024
Reviewed By: Josef Shargorodsky, MD, MPH, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.