Myasthenia gravis
Neuromuscular disorder - myasthenia gravisMyasthenia gravis is a neuromuscular disorder. Neuromuscular disorders involve the muscles and the nerves that control them.
Causes
Myasthenia gravis is an autoimmune disorder. An autoimmune disorder occurs when the immune system mistakenly attacks healthy tissue. Antibodies are proteins made by the body's immune system when it detects harmful substances. Antibodies may be produced when the immune system mistakenly considers healthy tissue to be a harmful substance, such as in the case of myasthenia gravis. In people with myasthenia gravis, the body produces antibodies that block the muscle cells from receiving messages (conveyed by neurotransmitters) from the nerve cells.
Autoimmune disorder
An autoimmune disorder occurs when the body's immune system attacks and destroys healthy body tissue by mistake. There are more than 80 autoimmune d...

Antibodies
An antibody is a protein produced by the body's immune system when it detects harmful substances, called antigens. Examples of antigens include micr...

In some cases, myasthenia gravis is linked to tumors of the thymus (an organ of the immune system).
Myasthenia gravis can affect people at any age. It is most common in young women and older men.
Symptoms
Myasthenia gravis causes weakness of the voluntary muscles. These are muscles that you can control. Autonomic muscles of the heart and digestive tract are usually not affected. The muscle weakness of myasthenia gravis worsens with activity and improves with rest.
This muscle weakness can lead to a variety of symptoms, including:
-
Double vision and drooping eyelids (ptosis) are the most common first symptoms
Double vision
There are many types of eye problems and vision disturbances, such as: Halos Blurred vision (the loss of sharpness of vision and the inability to see...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleDrooping eyelids
Eyelid drooping is excess sagging of the upper eyelid. The edge of the upper eyelid may be lower than it should be (ptosis) or there may be excess b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Breathing difficulty because of weakness of the chest wall muscles
Breathing difficulty
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chewing or swallowing difficulty, causing frequent gagging, choking, or drooling
- Difficulty climbing stairs, lifting objects, or rising from a seated position
- Difficulty talking
- Drooping head
-
Facial paralysis or weakness of the facial muscles
Facial paralysis
Facial paralysis means that a person is no longer able to move some or all of the muscles on one or both sides of the face.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fatigue
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Hoarseness or changing voice
Hoarseness or changing voice
Hoarseness refers to difficulty making sounds when trying to speak. Vocal sounds may be weak, breathy, scratchy, or husky, and the pitch or quality ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Difficulty maintaining steady gaze
Exams and Tests
Your health care provider will perform a physical exam. This includes a detailed nervous system (neurological) examination. This may show:
- Muscle weakness, with eye muscles usually affected first
- Weakness usually fluctuates and gets worse with exercise
- Normal reflexes and feeling (sensation)
Tests that may be done include:
-
Blood test to check for acetylcholine receptor antibodies, and others, associated with this disease
Acetylcholine receptor antibodies
Acetylcholine receptor antibody is a protein found in the blood of many people with myasthenia gravis. The antibody affects the part of nerve cells ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
CT or MRI scan of the chest to look for a tumor
CT
A computed tomography (CT) scan is an imaging method that uses x-rays to create pictures of cross-sections of the body. Related tests include:Abdomin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMRI
A magnetic resonance imaging (MRI) scan is an imaging test that uses powerful magnets and radio waves to create pictures of the body. It does not us...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nerve conduction studies to test how fast electrical signals move through a nerve
Nerve conduction studies
Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve. This test is done along with electromyography (EM...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Electromyography (EMG) to test the health of the muscles and the nerves that control the muscles
Electromyography (EMG)
Electromyography (EMG) is a test that checks the health of the muscles and the nerves that control the muscles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pulmonary function tests to measure breathing and how well the lungs are functioning
Pulmonary function tests
Pulmonary function tests are a group of tests that measure breathing and how well the lungs are functioning.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Edrophonium test to see if this medicine reverses the symptoms for a short time
Treatment
There is no known cure for myasthenia gravis. Treatment may allow you to have periods without any symptoms (remission).
Lifestyle changes can often help you continue your daily activities. The following may be recommended:
- Resting throughout the day
- Using an eye patch if double vision is bothersome
- Avoiding stress and heat exposure, which can make symptoms worse
Medicines that may be prescribed include:
- Neostigmine or pyridostigmine to improve communication between the nerves and muscles
- Prednisone and other medicines (such as azathioprine, cyclosporine, or mycophenolate mofetil) to suppress the immune system response if you have severe symptoms and other medicines have not worked well
- Other immunological therapies target specific immune cells or inflammatory response
Crisis situations (myasthenic crisis) are attacks of weakness of the breathing muscles. These attacks can occur without warning when either too much or too little medicine is taken. These attacks usually last no longer than a few weeks. You may need to be admitted to the hospital, where you may need breathing assistance with a ventilator.
Ventilator
A ventilator is a machine that breathes for you or helps you breathe. It is also called a breathing machine or respirator. The ventilator: Is attac...
Read Article Now Book Mark ArticleA procedure called plasmapheresis may also be used to help end the crisis. This procedure involves removing the clear part of the blood (plasma), which contains the antibodies. This may be replaced with donated plasma that is free of antibodies, or with other fluids. Plasmapheresis may also help reduce symptoms for 4 to 6 weeks and is often used before surgery.
A medicine called intravenous immunoglobulin (IVIg) may also be used
Surgery to remove the thymus (thymectomy) may result in permanent remission or less need for medicines, especially when there is a tumor present.
If you have eye problems, your provider may suggest lens prisms to improve vision. Surgery may also be recommended to treat your eye muscles.
Physical therapy can help maintain your muscle strength. This is especially important for the muscles that support breathing.
Some medicines can worsen symptoms and should be avoided. Before taking any medicine, ask your provider whether it is OK for you to take it.
Support Groups
You can ease the stress of illness by joining a myasthenia gravis support group. Sharing with others who have common experiences and problems can help you not feel alone.
Myasthenia gravis support group
The following organizations provide information on myasthenia gravis:Genetic and Rare Diseases Information Center -- rarediseases. info. nih. gov/dis...

Outlook (Prognosis)
There is no cure, but long-term remission is possible. You may have to restrict some daily activities. People who have only eye symptoms (ocular myasthenia gravis), may develop generalized myasthenia over time.
A woman with myasthenia gravis can get pregnant, but careful prenatal care is important. The baby may be weak and require medicines for a few weeks after birth, but usually will not develop the disorder.
Possible Complications
The condition may cause life-threatening breathing problems. This is called a myasthenic crisis.
People with myasthenia gravis are at higher risk for other autoimmune disorders, such as thyrotoxicosis, rheumatoid arthritis, and systemic lupus erythematosus (lupus).
Thyrotoxicosis
Hyperthyroidism is a condition in which the thyroid gland makes too much thyroid hormone. The condition is often called overactive thyroid.

Rheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...

Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the immune system of the body mistakenly attacks healthy tissue. It c...

When to Contact a Medical Professional
Call your provider if you develop symptoms of myasthenia gravis.
Go to the emergency room or call 911 or the local emergency number if you have breathing difficulty or swallowing problems.
References
Chang CWJ. Myasthenia gravis and Guillain-Barré syndrome. In: Parrillo JE, Dellinger RP, eds. Critical Care Medicine: Principles of Diagnosis and Management in the Adult. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 61.
Guptill JT, Sanders DB. Disorders of neuromuscular transmission. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley's and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 108.
Narayanaswami P, Sanders DB, Wolfe G, et al. International Consensus Guidance for Management of Myasthenia Gravis: 2020 Update. Neurology. 2021;96(3):114-122. PMID: 33144515 pubmed.ncbi.nlm.nih.gov/33144515/.
-
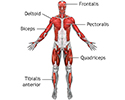
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
-
Ptosis - drooping of the eyelid - illustration
Drooping of the eyelid is called ptosis. Ptosis may result from damage to the nerve that controls the muscles of the eyelid, problems with the muscle strength (as in myasthenia gravis), or from swelling of the lid.
Ptosis - drooping of the eyelid
illustration
-
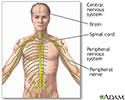
Central nervous system and peripheral nervous system - illustration
The central nervous system comprises the brain and spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
-
Superficial anterior muscles - illustration
Superficial muscles are close to the surface of the skin. Muscles which lie closer to bone or internal organs are called deep muscles.
Superficial anterior muscles
illustration
-
Ptosis - drooping of the eyelid - illustration
Drooping of the eyelid is called ptosis. Ptosis may result from damage to the nerve that controls the muscles of the eyelid, problems with the muscle strength (as in myasthenia gravis), or from swelling of the lid.
Ptosis - drooping of the eyelid
illustration
-
Central nervous system and peripheral nervous system - illustration
The central nervous system comprises the brain and spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
Review Date: 4/29/2023
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School of Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.