Ear infection - acute
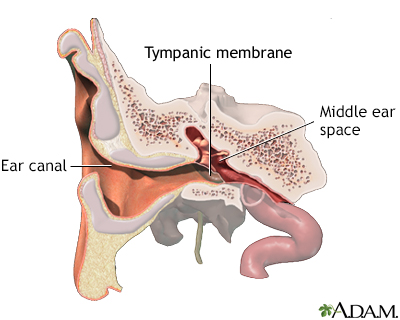
Suspected ear infections are one of the most common reasons parents take their children to their health care provider. The most common type of ear infection is called otitis media. It is caused by swelling and infection of the middle ear. The middle ear is located just behind the eardrum.
An acute ear infection starts over a short period and is painful. Ear infections that last a long time or come and go are called chronic ear infections.
Chronic ear infections
Chronic ear infection is fluid, swelling, or an infection behind the eardrum that does not go away or keeps coming back. It may cause long-term or p...

Ear infection - acute - Animation
Is your child irritable, inconsolably crying, feverish, and having trouble sleeping? If so, your child may have an ear infection. Ear infections are one of the most common reasons parents take their children to the doctor. The most common type is called otitis media, which means an inflammation and infection of the middle ear. The middle ear is located just behind the eardrum. The Eustachian tube runs from the middle of each ear to the back of the throat. This tube drains fluid normally made in the middle ear. If the tube gets blocked, fluid can build up, leading to infection. Ear infections are common in infants and children because their tiny. Eustachian tubes become easily clogged. They're often caused by allergies, colds, and excess mucus and saliva produced during teething. Infants with an ear infection will often be irritable. You may have a hard time consoling their crying, and your child may have a fever and not sleep very well. Older children may have an ear ache and tell you their ear feels full. Because ear infections have fluid behind the ear drum, you can use an electronic ear monitor to detect this fluid at home. Children under 6 months old who might have an ear infection need to see a doctor. Your child's doctor will look inside the child's ear using an instrument called an otoscope. The doctor might see areas of redness, air bubbles behind the ear drum, and fluid inside the middle ear. Often, an ear infection will clear up on its own. For older children, you can place a warm cloth or bottle on their ear and give them over-the-counter ear drops to relieve their pain. If bacteria caused the ear infection, your child may need to take antibiotics. In fact, all ear infections in children under 6 months old are treated with antibiotics. If the infection does NOT go away, on its own or with treatment, the doctor may recommend ear tube surgery. In this procedure, a tiny tube is inserted into the eardrum to drain the fluid. The tube will usually fall out on its own. Ear infections are very treatable, but they may come back again. If your child has to take an antibiotic, make sure they take all of the medicine.
Causes
The eustachian tube runs from the middle of each ear to the back of the throat. Normally, this tube drains fluid that is made in the middle ear. If this tube gets blocked, fluid can build up. This can lead to infection.
- Ear infections are common in infants and children because their eustachian tubes are easily clogged.
- Ear infections can also occur in adults, although they are much less common than in children.

Eustachian tube
Ear infections are more common in children because their eustachian tubes are shorter, narrower, and more horizontal than in adults, making the movement of air and fluid difficult. Bacteria can become trapped when the tissue of the eustachian tube becomes swollen from colds or allergies. Bacteria trapped in the eustachian tube may produce an ear infection that pushes on the eardrum causing it to become red, swollen, and sore.
Anything that causes the eustachian tubes to become swollen or blocked may lead to more fluid buildup in the middle ear behind the eardrum. Some causes are:
- Allergies
Allergies
An allergy is an immune response or reaction to substances that are usually not harmful.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Colds and sinus infections
Colds
The common cold most often causes a runny nose, nasal congestion, and sneezing. You may also have a sore throat, cough, headache, or other symptoms....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSinus infections
Sinusitis is present when the tissue lining the sinuses become swollen or inflamed. It occurs as the result of an inflammatory reaction or an infect...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Excess mucus and saliva produced during teething
Teething
Teething is the growth of teeth through the gums in the mouth of infants and young children.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infected or overgrown adenoids (lymph tissue in the upper part of the throat)
Overgrown adenoids
The adenoids are lymph tissues that sit in your upper airway between your nose and the back of your throat. They are similar to the tonsils. Enlarge...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tobacco smoke
Ear infections are also more likely in children who spend a lot of time drinking from a sippy cup or bottle while lying on their back. Milk may enter the eustachian tube, which may increase the risk of an ear infection. Getting water in the ears will not cause an acute ear infection unless the eardrum has a hole in it.
Other risk factors for acute ear infections include:
- Attending day care (especially centers with more than 6 children)
- Changes in altitude or climate
- Cold climate
- Exposure to smoke
- Family history of ear infections
- Not being breastfed
- Pacifier use
- Recent ear infection
- Recent illness of any type (because illness lowers the body's resistance to infection)
- Birth defect, leading to deficiency in eustachian tube function
Symptoms
In infants, often the main sign of an ear infection is acting irritable or crying that cannot be soothed. Many infants and children with an acute ear infection have a fever or trouble sleeping. Tugging on the ear is not always a sign that the child has an ear infection.
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...

Symptoms of an acute ear infection in older children or adults include:
- Ear pain
- Fullness in the ear
- Feeling of general illness
- Nasal congestion
- Cough
Cough
Coughing is an important way to keep your throat and airways clear. But too much coughing may mean you have a disease or disorder. Some coughs are d...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lethargy
- Vomiting
Vomiting
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up forces the contents of the stomach up t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Diarrhea
- Hearing loss in the affected ear
Hearing loss
Hearing loss is being partly or totally unable to hear sound in one or both ears.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Drainage of fluid from the ear
- Loss of appetite
The ear infection may start shortly after a cold. Sudden drainage of yellow or green fluid from the ear may mean the eardrum has ruptured.
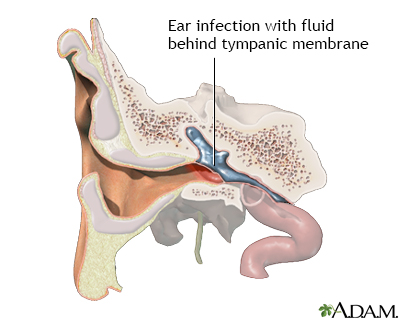
All acute ear infections involve fluid behind the eardrum. At home, you can use an electronic ear monitor to check for this fluid. You can buy this device at a drugstore. You still need to see your child's provider to confirm an ear infection.
Exams and Tests
Your provider will take your medical history and ask about symptoms.
Your provider will look inside the ears using an instrument called an otoscope. This exam may show:
- Areas of marked redness
- Bulging of the tympanic membrane (eardrum)
- Discharge from the ear
- Air bubbles or fluid behind the eardrum
- A hole (perforation) in the eardrum
Your provider might recommend a hearing test if you or your child has a history of ear infections.

Otoscopic exam of the ear
An otoscope is an instrument which is used to look into the ear canal. The ear speculum (a cone-shaped viewing piece of the otoscope) is slowly inserted into the ear canal while looking into the otoscope. The speculum is angled slightly toward the person's nose to follow the canal. A light beam extends beyond the viewing tip of the speculum. The otoscope is gently moved to different angles to view the canal walls and eardrum.
Treatment
Some ear infections clear on their own without antibiotics. Treating the pain and allowing the body time to heal itself is often all that is needed:
- Apply a warm cloth or warm water bottle to the affected ear.
- Use over-the-counter pain relief drops for ears. Or, ask your provider about prescription eardrops to relieve pain.
- Take over-the-counter medicines such as ibuprofen or acetaminophen for pain or fever. Do not give aspirin to children.
All children younger than 6 months with a fever or symptoms of an ear infection should see their provider. Children who are older than 6 months may be watched at home if they do not have:
- A fever higher than 102°F (38.9°C)
- More severe pain or other symptoms
- Other medical problems
If there is no improvement or if symptoms get worse, schedule an appointment with your provider to determine whether antibiotics are needed.
ANTIBIOTICS
A virus or bacteria can cause ear infections. Antibiotics will not help an infection that is caused by a virus. Most providers don't prescribe antibiotics for every ear infection. However, all children younger than 6 months with an ear infection are treated with antibiotics.
Your provider is more likely to prescribe antibiotics if your child:
- Is under age 2 years
- Has a fever
- Appears sick
- Does not improve in 24 to 48 hours
If antibiotics are prescribed, it is important to take them as directed and to take all of the medicines. Do not stop the medicine when symptoms go away. If the antibiotics do not seem to be working within 48 to 72 hours, contact your provider. You may need to switch to a different antibiotic.
Side effects of antibiotics may include nausea, vomiting, and diarrhea. Serious allergic reactions are rare, but may also occur.
Some children have repeat ear infections that seem to go away between episodes. They may receive a smaller, daily dose of antibiotics to prevent new infections.
SURGERY
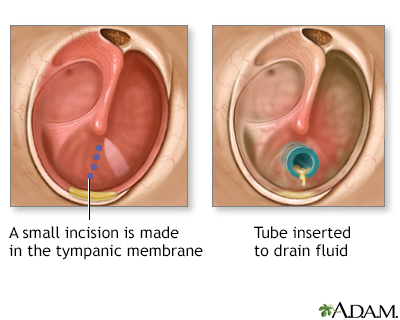
If an infection does not go away with the usual medical treatment, or if a child has many ear infections over a short period of time, their provider may recommend ear tubes:
Ear tubes
Ear tube insertion involves placing tubes through the eardrums. The eardrum is the thin layer of tissue that separates the outer and middle ear. No...

- If a child more than 6 months old has had 3 or more ear infections within 6 months or more than 4 ear infections within a 12-month period
- If a child less than 6 months old has had 2 ear infections in a 6- to 12-month period or 3 episodes in 24 months
- If the infection does not go away with medical treatment
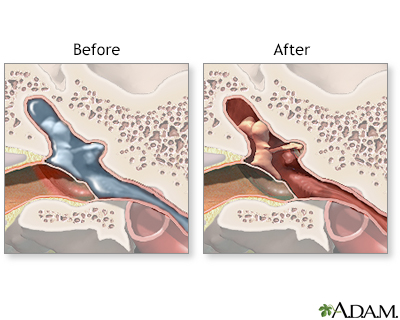
In this procedure, a tiny tube is inserted into the eardrum, keeping open a small hole that allows air to get in so fluids can drain more easily (myringotomy).
The tubes often eventually fall out by themselves. Those that don't fall out may be removed in your provider's office.
If the adenoids are enlarged, removing them with surgery may be considered if ear infections continue to occur. Removing tonsils does not seem to help prevent ear infections.
Ear tube insertion - Animation
If your child gets a lot of ear infections, he may need to have surgery. Let's talk about ear tube insertion. So, why does my child need ear tube surgery? Your child has been having ear infections, probably for a long time, and they either won't go away or they keep coming back. If your child doesn't have ear tube surgery, there's a chance he will lose some hearing or have other long-term ear problems. Once a decision to have surgery has been made, it's good to know what happens during the surgery. Your child will be given general anesthesia. He'll be unconscious and unable to feel pain. The surgeon will make a small cut in your child's eardrum and remove any fluid behind it. Once the fluid is removed, the surgeon will place a small tube through the eardrum. The tube will allow air to flow inward. This keeps the pressure the same on both sides of the eardrum, while letting any fluid still behind the eardrum flow out. Your child will probably go home the same day as surgery. He'll probably be fussy and groggy while the anesthesia wears off. On your way home, you may need to stop at the drug store to pick up antibiotic drops to use in your child's ears for the first few days after surgery. The cut in your child's eardrum will heal on its own, and the tube will eventually fall out. Your child will be able to return to his normal activities shortly. But some doctors may recommend that your child use earplugs when he swims or bathes, to keep water out of his ears. After a child has ear tube surgery, he will usually have fewer ear infections. And if he does have an ear infection, he will usually recover faster than he used to.
Outlook (Prognosis)
Most often, an ear infection is a minor problem that gets better. Ear infections can be treated, but they may occur again in the future.
Most children will have slight short-term hearing loss during and right after an ear infection. This is due to fluid in the ear. Fluid can stay behind the eardrum for weeks or even months after the infection has cleared.
Fluid can stay behind the eardrum
Otitis media with effusion (OME) is thick or sticky fluid behind the eardrum in the middle ear. It occurs without an ear infection. Note: This artic...

Speech or language delay is uncommon. It may occur in a child who has lasting hearing loss from many repeated ear infections.
Possible Complications
In rare cases, a more serious infection may develop, such as:
- Tearing of the eardrum
- Spreading of infection to nearby tissues, such as infection of the bones behind the ear (mastoiditis) or infection of the brain membrane (meningitis)
Mastoiditis
Mastoiditis is an infection of the mastoid bone of the skull. The mastoid bone is located just behind the ear.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chronic otitis media
- Collection of pus in or around the brain (abscess)

Mastoiditis - redness and swelling behind ear
Mastoiditis is an infection of the bony air cells in the mastoid bone, located just behind the ear. It is rarely seen today because of the use of antibiotics to treat ear infections. This child has noticeable swelling and redness behind his right ear because of mastoiditis.
When to Contact a Medical Professional
Contact your provider if:
- You have swelling behind the ear.
- Your symptoms get worse, even with treatment.
- You have a high fever or severe pain.
- Severe pain suddenly stops, which may indicate a ruptured eardrum.
- New symptoms appear, especially severe headache, dizziness, swelling around the ear, or twitching of the face muscles.
Let your provider know right away if a child younger than 6 months has a fever, even if the child doesn't have other symptoms.
Prevention
You can reduce your child's risk of ear infections with the following measures:
- Wash your hands and your child's hands and toys to decrease the chance of getting a cold.
- If possible, choose a day care that has 6 or fewer children. This can reduce your child's chances of getting a cold or other infection.
- Avoid using pacifiers.
- Breastfeed your baby.
- Avoid bottle feeding your child when they are lying down.
- Avoid smoking.
- Make sure your child's immunizations are up to date. The pneumococcal vaccine prevents infections from the bacteria that most commonly cause acute ear infections and many respiratory infections.
Pneumococcal vaccine
Content below is taken in its entirety from the CDC Information Statement (VIS): www. cdc. gov/vaccines/hcp/current-vis/pneumococcal-conjugate. html...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Reviewed By
Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Haddad J. General considerations and evaluation of the ear. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 676.
Pelton SI. Otitis externa, otitis media, and mastoiditis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 61.
Player B. Otitis media. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 680.
Rosenfeld RM, Tunkel DE, Schwartz SR, et al. Clinical Practice Guideline: Tympanostomy tubes in children (update).Otolaryngol Head Neck Surg. 2022;166(1_suppl):S1-S55. PMID: 35138954 pubmed.ncbi.nlm.nih.gov/35138954/.
Schilder AGM, Rosenfeld RM, Venekamp RP. Acute otitis media and otitis media with effusion. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 199.






 All rights reserved.
All rights reserved.