Nephrogenic diabetes insipidus
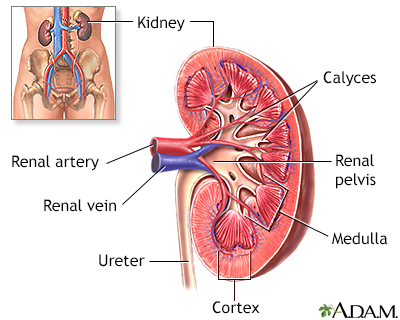
Nephrogenic diabetes insipidus (NDI) is a disorder in which a defect in the small tubes (tubules) in the kidneys causes a person to pass a large amount of urine and lose too much water.
Causes
Normally, the kidney tubules allow most water in the blood to be filtered and returned to the blood.
NDI occurs when the kidney tubules do not respond to a hormone in the body called antidiuretic hormone (ADH), also called vasopressin. ADH normally causes the kidneys to make the urine more concentrated.
Antidiuretic hormone
Antidiuretic blood test measures the level of antidiuretic hormone (ADH) in blood.
Read Article Now Book Mark ArticleAs a result of not responding to the ADH signal, the kidneys release too much water into the urine. This causes the body to produce a large quantity of very dilute urine.
NDI is very rare. Congenital nephrogenic diabetes insipidus means it is present at birth. It is a result of a genetic variant passed down through families. Men are usually affected, though women can pass this gene on to their children.
Most commonly, NDI develops because of other reasons. This is called an acquired disorder. Factors that can trigger the acquired form of this condition include:
- Blockage in the urinary tract
- High blood calcium levels
- Low blood potassium levels
- Use of certain medicines (lithium, demeclocycline, amphotericin B)
Symptoms
You may have intense or uncontrollable thirst, and crave ice water.
You will produce large amounts of urine, usually more than 3 liters, and up to 15 liters per day. The urine is very dilute and looks almost like water. You may need to urinate every hour or even more, even during the night when you are not eating or drinking as much.
If you do not drink enough fluids, dehydration can result. Symptoms may include:
- Dry mucous membranes
- Dry skin
- Sunken appearance to eyes
- Sunken fontanelles (soft spot) in infants
- Changes in memory or balance
Other symptoms that can occur due to lack of fluids, causing dehydration, include:
- Fatigue, feeling weak
- Headache
Headache
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Irritability
- Low body temperature
- Muscle pain
- Rapid heart rate
- Weight loss
- A change in alertness, and even coma
Coma
Decreased alertness is a state of reduced awareness and is often a serious condition. A coma is the most severe state of decreased alertness from whi...
Read Article Now Book Mark Article
Exams and Tests
Your health care provider will examine you and ask about your or your child's symptoms.
A physical exam may reveal:
- Low blood pressure
- Rapid pulse
- Shock
Shock
Shock is a life-threatening condition that occurs when the body is not getting enough blood flow. Lack of blood flow means the cells and organs do n...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Signs of dehydration
Tests may reveal:
- High serum osmolality
High serum osmolality
Osmolality blood test is a test that measures the concentration of all chemical particles found in the fluid part of blood. Osmolality in the urine c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High urine output, regardless of how much fluid you drink
- Kidneys do not concentrate urine when you are given ADH (usually a medicine called desmopressin)
- Low urine osmolality
Urine osmolality
The osmolality urine test measures the concentration of chemicals in urine. Osmolality in the blood can be measured using a blood test.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Normal or high blood ADH levels
Other tests that may be done include:
- Blood electrolyte test
Blood electrolyte test
The sodium blood test measures the concentration of sodium in the blood. Sodium can also be measured using a urine test.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urine 24-hour volume
Urine 24-hour volume
The urine 24-hour volume test measures the amount of urine produced in a day. The amounts of creatinine, protein, and other chemicals released into ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urine concentration test
Urine concentration test
A urine concentration test measures the ability of the kidneys to conserve or excrete water.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urine specific gravity
Urine specific gravity
Urine specific gravity is a laboratory test that shows the total concentration of all chemical particles in the urine.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Supervised water deprivation test
Water deprivation test
A urine concentration test measures the ability of the kidneys to conserve or excrete water.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
The goal of treatment is to control the body's fluid levels. A large amount of fluids will be given. The amount should be about equal to the amount of water being lost in the urine.
If the condition is due to a certain medicine, stopping the medicine may improve symptoms. But, do not stop taking any medicine without first talking to your provider.
Medicines may be given to improve symptoms by reducing urine output.
Outlook (Prognosis)
If a person drinks enough water, this condition will not have much effect on the fluid or electrolyte balance of the body. Sometimes, passing a lot of urine for a long time can cause other electrolyte problems.
Electrolyte
Electrolytes are minerals in your blood and other body fluids that carry an electric charge. Electrolytes affect how your body functions in many ways...
Read Article Now Book Mark ArticleIf the person does not drink enough fluids, high urine output may cause dehydration and high levels of sodium in the blood.
NDI that is present at birth is a long-term condition requiring lifelong treatment.
Possible Complications
Untreated, NDI may cause any of the following:
- Dilation of the ureters and bladder
- High blood sodium (hypernatremia)
Hypernatremia
The sodium blood test measures the concentration of sodium in the blood. Sodium can also be measured using a urine test.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Severe dehydration
- Shock
- Coma
When to Contact a Medical Professional
Contact your provider if you or your child has symptoms of this disorder.
Prevention
Congenital NDI cannot be prevented.
Treating the disorders that can lead to the acquired form of the condition may prevent it from developing in some cases.
Reviewed By
Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Al-Awqati Q, Radhakrishnan J. Disorders of sodium and water. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 102.
Bock ME, Dixon BP. Diabetes insipidus. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 570.
Bockenhauer D. Fluid, electrolyte, and acid-base disorders in children. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 73.
Scheinman SJ. Genetically based kidney transport disorders. In: Gilbert SJ, Weiner DE, eds. National Kidney Foundation Primer on Kidney Diseases. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 37.
Thompson CJ, Garrah A, Disorders of sodium, diabetes insipidus and hyponatremia. In: Robertson RP, eds. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 12.
 All rights reserved.
All rights reserved.