End-stage kidney disease
End-stage kidney disease (ESKD) is the last stage of long-term (chronic) kidney disease. This is when your kidneys can no longer support your body's needs.
Long-term (chronic) kidney disease
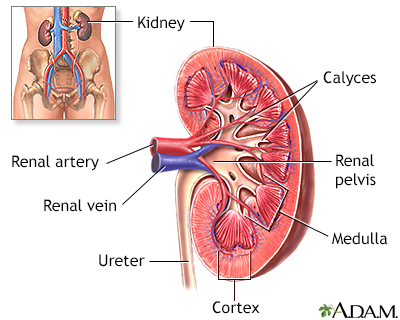
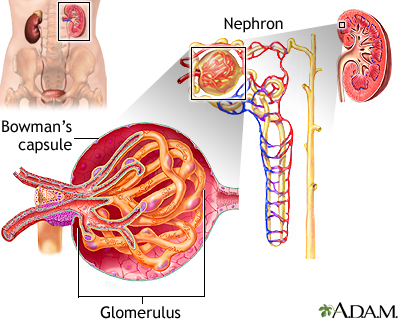
Chronic kidney disease is the slow loss of kidney function over time. The main job of the kidneys is to remove wastes and excess water from the body...

End-stage kidney disease is also called end-stage renal disease (ESRD).
Causes
The kidneys remove waste and excess water from the body. ESRD occurs when the kidneys are no longer able to work at a level needed for day-to-day life.
The most common causes of ESRD in the United States are diabetes and high blood pressure. These conditions can damage your kidneys.
Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
High blood pressure
Blood pressure is a measurement of the force exerted against the walls of your arteries as your heart pumps blood to your body. Hypertension is the ...

ESRD almost always comes after chronic kidney disease. The kidneys may slowly stop working during a period of 10 to 20 years before end-stage disease results.
Symptoms
Common symptoms may include:
- General ill feeling and fatigue
General ill feeling
Malaise is a general feeling of discomfort, illness, or lack of well-being.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Itching (pruritus) and dry skin
Pruritus
Itching is a tingling or irritation of the skin that makes you want to scratch the area. Itching may occur all over the body or only in one location...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Headache
Headache
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Weight loss without trying
- Loss of appetite
- Nausea
Other symptoms may include:
- Abnormally dark or light skin
- Nail changes
- Bone pain
- Drowsiness and confusion
Drowsiness
Drowsiness refers to feeling more sleepy than normal during the day. People who are drowsy may fall asleep when they do not want to or at times whic...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleConfusion
Confusion is the inability to think as clearly or quickly as you normally do. You may feel disoriented and have difficulty paying attention, remembe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Problems concentrating or thinking
- Numbness in the hands, feet, or other areas
- Muscle twitching or cramps
Muscle twitching
Muscle twitches are fine movements of a small area of muscle.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Breath odor
- Easy bruising, nosebleeds, or blood in the stool
- Excessive thirst
- Frequent hiccups
- Problems with sexual function
- Menstrual periods stop (amenorrhea)
- Sleep problems
- Swelling of the feet and hands (edema)
Edema
Swelling is the enlargement of organs, skin, or other body parts. It is caused by a buildup of fluid in the tissues. The extra fluid can lead to a ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Vomiting, often in the morning
Exams and Tests
Your health care provider will perform a physical exam and order blood tests. Most people with this condition have high blood pressure.
People with ESRD will make much less urine than normal, or their kidneys may no longer make urine.
ESRD changes the results of many tests. People receiving dialysis will need these and other tests done often:
- Potassium
Potassium
This test measures the amount of potassium in the fluid portion (serum) of the blood. Potassium (K+) helps nerves and muscles communicate. It also ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sodium
Sodium
The sodium blood test measures the concentration of sodium in the blood. Sodium can also be measured using a urine test.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Albumin
Albumin
Albumin is a protein made by the liver. A serum albumin test measures the amount of this protein in the clear liquid portion of the blood. Albumin c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Phosphorous
Phosphorous
The phosphorus blood test measures the amount of phosphate in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Calcium
Calcium
The calcium blood test measures the level of calcium in the blood. This article discusses the test to measure the total amount of calcium in your blo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cholesterol
Cholesterol
Cholesterol is a soft, wax-like substance found in all parts of the body. Your body needs cholesterol to work properly. But too much cholesterol ca...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Magnesium
Magnesium
A serum magnesium test measures the level of magnesium in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Complete blood count (CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Electrolytes
Electrolytes
Electrolytes are minerals in your blood and other body fluids that carry an electric charge. Electrolytes affect how your body functions in many ways...
Read Article Now Book Mark Article
This disease may also change the results of the following tests:
- Vitamin D
- Parathyroid hormone
Parathyroid hormone
The PTH test measures the level of parathyroid hormone in the blood. PTH stands for parathyroid hormone. It is a protein hormone released by the par...
Read Article Now Book Mark Article - Bone density test
Bone density test
A bone mineral density (BMD) test measures how much calcium and other types of minerals are in an area of your bone. This test helps your health care...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Dialysis - Animation
Your kidneys are in charge of filtering wastes out of your blood. But, if your kidneys don't work as well as they should, you may need a procedure called dialysis, a process that removes wastes in place of your kidneys. Let's talk about dialysis. Your kidneys have several important jobs. In addition to filtering your blood, they help maintain just the right balance of water, acids, and minerals in your body. They also function as part of the endocrine system producing hormones. If you've had kidney disease for many years, or your kidneys have suddenly failed because of disease or injury, your doctor may recommend that you have dialysis, a treatment that replaces some of what the kidneys do, removing waste and excess fluid from your blood. It is sometimes used as a holding treatment while awaiting a kidney transplant. Here's how dialysis works. First, your doctor will need to create an access to reach your blood vessels. If you need dialysis only for a short period of time, that access will be made using a hollow tube, called a catheter. Usually the catheter is placed into a large vein in your neck, chest, or leg near your groin. If you're having dialysis for a longer period of time, you'll need a more permanent access. To create this access, your doctor will connect one of your arteries to one of your veins. Then whenever you have dialysis, a needle is simply placed into this access area. During each dialysis session, your blood is removed from your body through the needle. It's sent across a special filter, which removes harmful substances from your blood. Then, your clean blood is sent back into your body. Often, you'll visit a special center for dialysis about three times a week. Each session lasts three to four hours. Or, you may be able to do dialysis right at home three times a week or even daily. Home sessions are shorter, about 2 to 3 hours, and they're easier for your body to tolerate. Before you perform dialysis at home, a nurse will teach you how to place the needle, how to clean the machine, and monitor your blood pressure during treatment. It's important when you're having dialysis that you do all of your scheduled sessions. Also, call your doctor right away if you have any problems, like swelling, redness, fever, a drop in blood pressure, or bleeding. These could be signs that you've developed an infection or other complication from your dialysis, and need medical attention.
ESRD may need to be treated with dialysis or kidney transplant. You may need to stay on a special diet or take medicines to help your body work well.
Dialysis
Dialysis treats end-stage kidney failure. It removes harmful substances from the blood when the kidneys cannot. This article focuses on peritoneal d...
Read Article Now Book Mark ArticleKidney transplant
A kidney transplant is surgery to place a healthy kidney into a person with kidney failure.

DIALYSIS
Dialysis does some of the job of the kidneys when they stop working well.
Dialysis can:
- Remove extra salt, water, and waste products so they do not build up in your body
- Keep safe levels of minerals and vitamins in your body
- Help control blood pressure
- Help the body make red blood cells
Your provider will discuss dialysis with you before you need it. Dialysis removes waste from your blood when your kidneys can no longer do their job.
- Usually, you will go on dialysis when you have only 10% to 15% of your kidney function left.
- Even people who are waiting for a kidney transplant may need dialysis while waiting.
Two different methods are used to perform dialysis:
- During hemodialysis, your blood passes through a tube into an artificial kidney, or filter. This method can be done at home or at a dialysis center.
Hemodialysis
Dialysis treats end-stage kidney disease also called kidney failure. It removes waste from your blood when your kidneys can no longer do their job. ...
Read Article Now Book Mark Article - During peritoneal dialysis, a special solution passes into your belly though a catheter tube. The solution remains in your abdomen for period of time and then is removed. This method can be done at home, at work, or while traveling.
Peritoneal dialysis
Dialysis treats end-stage kidney failure. It removes harmful substances from the blood when the kidneys cannot. This article focuses on peritoneal d...
Read Article Now Book Mark Article
KIDNEY TRANSPLANT
A kidney transplant is surgery to place a healthy kidney into a person with kidney failure. Your provider will refer you to a transplant center. There, you will be seen and evaluated by the transplant team. They will want to make sure that you are a good candidate for kidney transplant.
SPECIAL DIET
You may need to continue following a special diet for chronic kidney disease. The diet may include:
Diet for chronic kidney disease
You may need to make changes to your diet when you have chronic kidney disease (CKD). These changes may include limiting fluids, eating a low-protei...

- Eating foods low in protein to limit your total daily protein intake
- Getting enough calories if you are losing weight
- Limiting fluids
- Limiting salt, potassium, phosphorous, and other electrolytes
OTHER TREATMENT
Other treatment depends on your symptoms, but may include:
- Extra calcium and vitamin D. (Always talk to your provider before taking supplements.)
- Medicines called phosphate binders, to help prevent blood phosphorous levels from becoming too high.
- Treatment for anemia, such as extra iron in the diet, iron pills or shots, shots of a medicine called erythropoietin, and blood transfusions.
- Medicines to control your blood pressure.
Talk to your provider about vaccinations that you may need, including:
- Hepatitis A vaccine
Hepatitis A vaccine
All content below is taken in its entirety from the CDC Hepatitis A Vaccine Information Statement (VIS): www. cdc. gov/vaccines/hcp/current-vis/hepat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hepatitis B vaccine
Hepatitis B vaccine
All content below is taken in its entirety from the CDC Hepatitis B Vaccine Information Statement (VIS): www. cdc. gov/vaccines/hcp/current-vis/hepat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - COVID-19 vaccine
COVID-19 vaccine
COVID-19 vaccines are used to prepare the body's immune system to protect against COVID-19. Everyone ages 6 months and older should get a 2024-2025 C...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Flu vaccine
Flu vaccine
All content below is taken in its entirety from the CDC Inactivated Influenza Vaccine Information Statement (VIS) www. cdc. gov/vaccines/hcp/current-...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pneumonia vaccine (PPV)
Pneumonia vaccine
All content below is taken in its entirety from the CDC Pneumococcal Polysaccharide Vaccine Information Statement (VIS): CDC review information for P...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Support Groups
Some people may benefit from taking part in a kidney disease support group.
Kidney disease support group
The following organizations are good resources for information on kidney disease:American Geriatrics Society -- www. healthinaging. org/a-z-topic/kid...

Outlook (Prognosis)
End-stage kidney disease leads to death if you do not have dialysis or a kidney transplant. Both of these treatments have risks. The outcome is different for each person.
Possible Complications
Health problems that can result from ESRD include:
- Anemia
Anemia
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. Different type...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bleeding from the stomach or intestines
- Bone, joint, and muscle pain
- Changes in blood sugar (glucose)
- Damage to nerves of the legs and arms
Damage to nerves of the legs and arms
Peripheral nerves carry information to and from the brain. They also carry signals in both directions between the spinal cord and the rest of the bo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fluid buildup around the lungs
Fluid buildup around the lungs
A pleural effusion is a buildup of fluid between the layers of tissue that line the lungs and chest cavity.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High blood pressure, heart attack, and heart failure
High blood pressure
Blood pressure is a measurement of the force exerted against the walls of your arteries as your heart pumps blood to your body. Hypertension is the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHeart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHeart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High potassium level
High potassium level
High potassium level is a problem in which the amount of potassium in the blood is higher than normal. The medical name of this condition is hyperka...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Increased risk of infection
- Liver damage or failure
- Malnutrition
Malnutrition
Malnutrition is the condition that occurs when your body does not get enough nutrients.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Miscarriages or infertility
- Restless legs syndrome
Restless legs syndrome
Restless legs syndrome (RLS) is a nervous system problem that causes you to feel an unstoppable urge to get up and pace or walk. You feel uncomforta...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Stroke, seizures, and dementia
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSeizures
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleDementia
Dementia is a loss of brain function that occurs with certain diseases. It affects one or more brain functions such as memory, thinking, language, j...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Swelling and edema
- Weakening of the bones and fractures related to high phosphorous and low calcium levels
Reviewed By
Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Inker LA, Levey AS. Staging and management of chronic kidney disease. In: Gilbert SJ, Weiner DE, Bomback AS, Perazella MA, Rifkin DE, eds. National Kidney Foundation Primer on Kidney Diseases. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 51.
Taal MW. Classification and management of chronic kidney disease. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 59.
Yeun JY, Young B, Depner TA, Chin AA. Hemodialysis. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 63.

 All rights reserved.
All rights reserved.