Insulinoma
An insulinoma is a tumor in the pancreas that produces too much insulin.
Tumor
A tumor is an abnormal growth of body tissue. Tumors can be cancerous (malignant) or noncancerous (benign).
Read Article Now Book Mark ArticleCauses
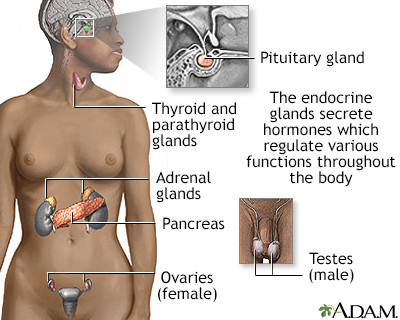
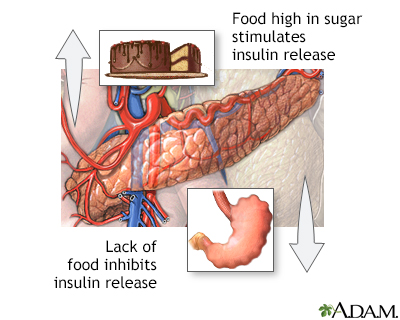
The pancreas is an organ in the abdomen. The pancreas makes several enzymes and hormones, including the hormone insulin. Insulin's job is to reduce the level of sugar (glucose) in the blood by helping sugar move into cells.
Enzymes
Enzymes are complex proteins that cause a specific chemical change. For example, they can help break down the foods we eat so the body can use them....
Read Article Now Book Mark ArticleMost of the time when your blood sugar level decreases, the pancreas stops making insulin to make sure that your blood sugar stays in the normal range. Tumors of the pancreas that produce too much insulin are called insulinomas. Insulinomas keep making insulin, even when it's not needed, and can make your blood sugar level too low (hypoglycemia).
A high blood insulin level causes a low blood sugar level (hypoglycemia). Hypoglycemia may be mild, leading to symptoms such as anxiety and hunger. Or it can be severe, leading to seizures, coma, and even death.
Hypoglycemia
Low blood sugar is a condition that occurs when the body's blood sugar (glucose) decreases and is too low. Blood sugar below 70 mg/dL (3. 9 mmol/L) i...

Insulinomas are very rare tumors. They usually occur as single, small tumors. But there can also be several small tumors.
Most insulinomas are non-cancerous (benign) tumors. People with certain genetic disorders, such as multiple endocrine neoplasia type I, are at higher risk for insulinomas.
Multiple endocrine neoplasia type I
Multiple endocrine neoplasia (MEN) type I is a disease in which one or more of the endocrine glands are overactive or forms a tumor. It is passed do...

Symptoms
Symptoms are most common when you are fasting or skip or delay a meal. Symptoms may include:
- Anxiety, behavior changes, or confusion
Anxiety
Stress is a feeling of emotional or physical tension. It can come from any event or thought that makes you feel frustrated, angry, or nervous. Stres...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleConfusion
Confusion is the inability to think as clearly or quickly as you normally do. You may feel disoriented and have difficulty paying attention, remembe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Clouded vision
- Loss of consciousness or coma
Loss of consciousness
Decreased alertness is a state of reduced awareness and is often a serious condition. A coma is the most severe state of decreased alertness from whi...
Read Article Now Book Mark Article - Convulsions or tremor
Convulsions
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Dizziness or headache
- Hunger between meals; weight gain is common
- Fast heart rate or palpitations
Fast heart rate
A bounding pulse is a strong throbbing felt over one of the arteries in the body. It is due to a forceful heartbeat.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sweating
Exams and Tests
After fasting, your blood may be tested for:
- Blood C-peptide level
C-peptide
C-peptide is a substance that is created when the hormone insulin is produced and released into the body. The insulin C-peptide test measures the am...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood glucose level
- Blood insulin level
- Medicines that cause the pancreas to release insulin
- The response of your body to a shot of glucagon
CT, MRI, or PET scan of the abdomen may be done to look for a tumor in the pancreas. If a tumor is not seen in the scans, one of the following tests may be performed:
CT
An abdominal CT scan is an imaging test that uses x-rays to create cross-sectional pictures of the belly area. CT stands for computed tomography....

MRI
An abdominal magnetic resonance imaging scan is an imaging test that uses powerful magnets and radio waves. The waves create pictures of the inside ...

PET
A positron emission tomography (PET) scan is a type of imaging test. It uses a radioactive substance called a tracer to look for disease in the body...
Read Article Now Book Mark Article- Endoscopic ultrasound (test that uses a flexible scope and sound waves to view digestive system organs)
Endoscopic ultrasound
Endoscopic ultrasound is a type of imaging test. It is used to see organs in and near the digestive tract.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Octreotide scan (special test that checks for specific hormone-producing cells in the body)
- Pancreatic arteriography (test that uses special dye to view the arteries in the pancreas)
Arteriography
An arteriogram is an imaging test that uses x-rays and a special dye to see inside the arteries. It can be used to view arteries in the heart, brain...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pancreatic venous sampling for insulin (test that helps locate the approximate location of the tumor inside the pancreas)
Treatment
Surgery is the usual treatment for insulinoma. If there is a single tumor, it will be removed. If there are many tumors, part of the pancreas will need to be removed. At least 15% of the pancreas must be left to produce normal levels of enzymes for digestion.
In rare cases, the entire pancreas is removed if there are many insulinomas or they come back after surgery. Removing the entire pancreas leads to diabetes because there is no longer any insulin being produced. Insulin shots (injections) are then required.
If no tumor is found during surgery, or if you can't have surgery, you may get the medicine diazoxide to lower insulin production and prevent hypoglycemia. A water pill (diuretic) is given with this medicine to prevent the body from retaining fluid. Octreotide is another medicine that is used to reduce insulin release in some people.
Outlook (Prognosis)
In most cases, the tumor is non-cancerous (benign), and surgery can cure the disease. But a severe hypoglycemic reaction or the spread of a cancerous tumor to other organs can be life threatening.
Possible Complications
Complications may include:
- Severe hypoglycemic reaction
- Spread of a cancerous tumor (metastasis)
Metastasis
Metastasis is the movement or spreading of cancer cells from one organ or tissue to another. Cancer cells usually spread through the blood or the ly...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Diabetes if the entire pancreas is removed (rare), or food not being absorbed if too much of the pancreas is removed
- Inflammation and swelling of the pancreas
When to Contact a Medical Professional
Contact your health care provider if you develop any symptoms of insulinoma. Seizures and losing consciousness are an emergency. Call 911 or the local emergency number right away.
Reviewed By
Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 01/17/2025.
Arbelaez AM, Rickels MR. Hypoglycemia. In: Melmed S, Auchus RJ, Goldfine AB, Rosen CJ, Kopp PA, eds. Williams Textbook of Endocrinology. 15th ed. Philadelphia, PA: Elsevier; 2025:chap 39.
Asban A, Patel AJ, Reddy S, Wang T, Balentine CJ, Chen H. Cancer of the endocrine system. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 68.
National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology (NCCN guidelines): Neuroendocrine and adrenal tumors. Version 4.2024. www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf. Updated January 17, 2025. Accessed January 27, 2025.
Strosberg JR, Al-Toubah T. Neuroendocrine tumors. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 34.
 All rights reserved.
All rights reserved.