Gastroparesis
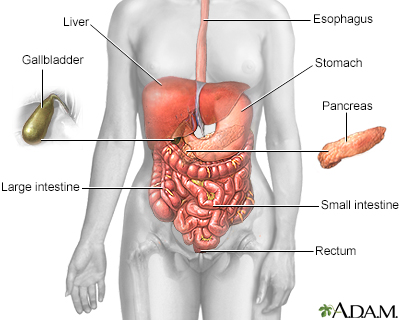
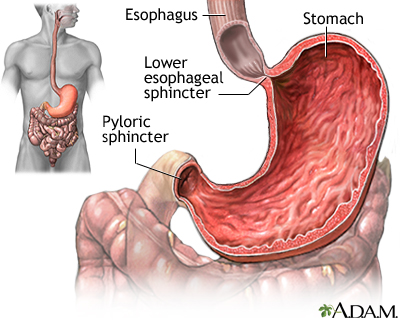
Gastroparesis is a condition that reduces the ability of the stomach to empty its solid contents. It does not involve a blockage (obstruction) of the outlet of the stomach.
Causes
The exact cause of gastroparesis is unknown. It may be caused by a disruption of nerve signals to the stomach. The condition is a common complication of diabetes. It can also follow some surgeries.
Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
Risk factors for gastroparesis include:
- Diabetes, especially long-term diabetes or if the blood sugar is very high
- Gastrectomy (surgery to remove part of the stomach)
Gastrectomy
Gastrectomy is surgery to remove part or all of the stomach. If only part of the stomach is removed, it is called partial gastrectomyIf the whole sto...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Systemic sclerosis and other autoimmune diseases
Systemic sclerosis
Scleroderma is a disease that involves the buildup of fibrous tissue in the skin and elsewhere in the body. It also damages the cells that line the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Post-viral illness
- Parkinson disease
- Use of medicine such as those that block certain nerve signals (anticholinergic medicine) or muscle contraction (narcotic pain relievers)
Symptoms
Symptoms may include:
- Abdominal distention
Abdominal distention
A swollen abdomen is when your belly area is bigger than usual.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Abdominal pain
- Hypoglycemia (in people with diabetes)
Hypoglycemia
Low blood sugar is a condition that occurs when the body's blood sugar (glucose) decreases and is too low. Blood sugar below 70 mg/dL (3. 9 mmol/L) i...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Nausea
Nausea
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up forces the contents of the stomach up t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Premature abdominal fullness after meals or feeling full after eating only a small amount of food
Premature abdominal fullness after meal
Satiety is the satisfied feeling of being full after eating. Early satiety is feeling full sooner than normal or after eating less than usual....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Weight loss without trying
Weight loss
Unexplained weight loss is a decrease in body weight, when you did not try to lose the weight on your own. Many people gain and lose weight. Uninten...
Read Article Now Book Mark Article - Vomiting
Vomiting
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up forces the contents of the stomach up t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Tests you may need include:
- Esophagogastroduodenoscopy (EGD).
Esophagogastroduodenoscopy
Esophagogastroduodenoscopy (EGD) is a test to examine the lining of the esophagus, stomach, and first part of the small intestine (the duodenum)....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Gastric emptying study (usually using isotope-labeled food). Other tests that are used include a wireless motility capsule or a breath test.
- Upper GI series.
Upper GI series
An upper GI and small bowel series is a set of x-rays taken to examine the esophagus, stomach, and small intestine. Barium enema is a different test ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
People with diabetes should always control their blood sugar level. Better control of blood sugar level may improve symptoms of gastroparesis. Eating small and more frequent meals and soft/pureed foods (called a small-particle diet) may also help relieve some symptoms.
Medicines that may help include:
- Erythromycin (short-term only)
- Metoclopramide, a medicine that helps empty the stomach, or domperidone (available with special approval in the US)
- Serotonin (5-HT4) agonist medicines, which act on serotonin receptors
- Anti-nausea treatments to help control nausea and vomiting
Other treatments may include:
- Electrical stimulation of the stomach
- Endoscopic myotomy (cutting muscles at the pylorus, the outlet of the stomach), called G-POEM (gastric per-oral endoscopic myotomy)
- Surgical procedure that creates an opening between the stomach and small intestine to allow food to move through the digestive tract more easily (gastroenterostomy)
If weight loss and malnutrition have occurred, a feeding tube may be inserted into the small intestine to give food until symptoms are better.
Outlook (Prognosis)
Many treatments, especially medicines, seem to provide only temporary benefit or have side effects when used for a long time. Gastroparesis is a chronic condition. Management of flare-ups may be helped by the use of diet and medicines. Endoscopic or surgical myotomy often provides a long-term improvement.
Possible Complications
Ongoing nausea and vomiting may cause:
- Dehydration
Dehydration
Dehydration occurs when your body does not have as much water and fluids as it needs. Dehydration can be mild, moderate, or severe, based on how much...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Electrolyte imbalances
Electrolyte
Electrolytes are minerals in your blood and other body fluids that carry an electric charge. Electrolytes affect how your body functions in many ways...
Read Article Now Book Mark Article - Malnutrition
People with diabetes may have serious complications from poor blood sugar control.
When to Contact a Medical Professional
Changes in your diet may help control symptoms. Contact your health care provider if symptoms continue or if you have new symptoms.
Reviewed By
Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Carmilleri M. Disorders of gastrointestinal motility. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 122.
Camilleri M, Kuo B, Nguyen L. ACG Clinical Guideline: Gastroparesis. Am J Gastroenterol. 2022;117(8):1197-1220. PMID: 35926490 pubmed.ncbi.nlm.nih.gov/35926490/.
Koch KL. Gastric neuromuscular function and neuromuscular disorders. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 50.
 All rights reserved.
All rights reserved.