Peutz-Jeghers syndrome
Peutz-Jeghers syndrome (PJS) is a rare disorder in which growths called polyps form in the intestines. A person with PJS has a high risk for developing certain cancers.
Causes
It is unknown how many people are affected by PJS. However, the National Institutes of Health estimates that it affects about 1 in 50,000 to 200,000 people.
PJS is caused by a mutation in the gene called STK11 (previously known as LKB1). There are two ways that PJS can occur:
- Familial PJS is inherited in families as an autosomal dominant trait. That means if one of your parents has this type of PJS, you have a 50% chance of inheriting the gene and having the disease.
Autosomal dominant
Autosomal dominant is one of many ways that a genetic trait or disorder can be passed down through families. In an autosomal dominant disease, if you...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Spontaneous PJS is not inherited from a parent. The gene mutation occurs on its own. Once someone carries the genetic change, their children have a 50% chance of inheriting it.
Symptoms
Symptoms of PJS are:
- Brownish or bluish-gray spots on the lips, gums, inner lining of the mouth, and skin
-
Clubbed fingers or toes
Clubbed fingers or toes
Clubbing is changes in the areas under and around the toenails and fingernails that occur with some disorders. The nails may also show changes....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cramping pain in the belly area
- Dark freckles on and around the lips of a child
-
Blood in the stool that can be seen with the naked eye (sometimes)
Blood in the stool
Black or tarry stools with a foul smell are a sign of a problem in the upper digestive tract. It most often indicates that there is bleeding in the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Vomiting
Exams and Tests
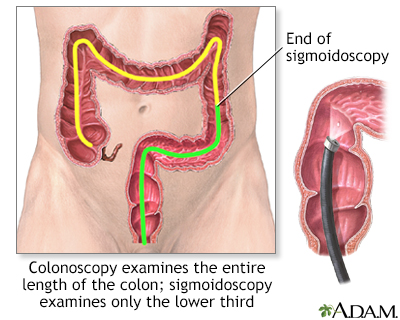
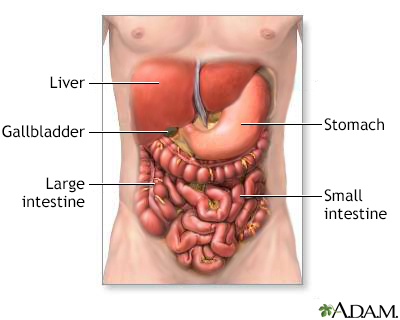
The polyps develop mainly in the small intestine, but also in the large intestine (colon). An exam of the colon called a colonoscopy will show colon polyps. The small intestine is evaluated in two ways. One is a barium x-ray (small bowel series). The other is a capsule endoscopy, in which a small camera is swallowed and then takes many pictures as it travels through the small intestine.
Colonoscopy
A colonoscopy is an exam that views the inside of the colon (large intestine) and rectum, using a tool called a colonoscope. The colonoscope has a sm...

Colon cancer screening - Animation
Colon cancer is one of the leading causes of cancer-related deaths in the United States. The good news is that earlier diagnosis due to screening tests often leads to a complete cure. Colorectal cancer starts in the large intestine, also known as the colon. Nearly all colon cancers begin as noncancerous, or benign, polyps, some of which may slowly develop into cancer. Screening can detect these polyps and early cancers. Polyps can be removed years before cancer even has a chance to develop. Your doctor can use two types of tools to screen for cancer. The first type is a stool test. Polyps in the colon and small cancers can bleed tiny amounts of blood that you can't see with the naked eye. The most common method to test for the presence of blood is the fecal occult blood test or FOBT. This test checks your stool for small amounts of blood that you may not be able to see. Two other stool tests are the fecal immunochemical test and the stool DNA test. The second type of screening tests involve looking at the lining of the colon. One of these tests is a sigmoidoscopy exam. This test uses a flexible scope to look at the lower portion of your colon. But, because it looks only at the last one-third of the large intestine, it may miss some cancers. So this test is done along with a stool test. A colonoscopy is similar to sigmoidoscopy, but it can see the entire colon. For this test, your doctor will give you instructions for cleansing your bowel. This is called bowel preparation. During the colonoscopy, you’ll receive medicine to make you relaxed and sleepy. Another test your doctor may recommend is a virtual colonoscopy, also called a CT colonography. This test uses a CAT scan and computer software to create a 3-D image of your large intestine. Beginning at age 45, all men and women should have a screening test for colon cancer. Screening options for people with average risk for colon cancer include visual based exams. These could be a colonoscopy every 10 years starting at age 45 or a virtual colonoscopy every 5 years. A Flexible sigmoidoscopy every 5 years or a Flexible sigmoidoscopy every 10 years plus stool testing with FIT done every year. Screening options also include stool based tests. People with average risk should have an FOBT or FIT every year. A colonoscopy is needed if the results are positive, or a Stool DNA test every 1 to 3 years. A colonoscopy is needed if the results are positive. People with certain risk factors for colon cancer may need screening at a younger age, or they may need screening more often. Such people include those with a family history of colon cancer, those with a history of previous colon cancer or polyps, or people with a history of ulcerative colitis or Crohn disease. The death rate for colon cancer has dropped in the past 15 years and this may be due to increased awareness and colon screening. In general, early diagnosis is much more likely to lead to a complete cure.
Additional exams may show:
-
Part of the intestine folded in on itself (intussusception)
Intussusception
Intussusception is the sliding of one part of the intestine into another. This article focuses on intussusception in children.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Benign (noncancerous) tumors in the nose, airways, ureters, or bladder
Laboratory tests may include:
- Complete blood count (CBC) -- may reveal anemia
Anemia
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. Different type...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genetic testing
-
Stool occult blood, to look for blood in stool
Stool occult blood
The stool guaiac test looks for hidden (occult) blood in a stool sample. It can find blood even if you cannot see it yourself. It is a common type ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Total serum iron and iron-binding capacity (TIBC) -- may indicate iron-deficiency anemia
Total serum iron and iron-binding capac...
Total iron binding capacity (TIBC) is a blood test to see if you have too much or too little iron in your blood. Iron moves through the blood attach...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Surgery may be needed to remove polyps that cause long-term problems. Iron supplements help counteract blood loss.
People with this condition should be monitored by a health care provider and checked regularly for cancerous polyp changes.
Support Groups
More information and support for people with PJS and their families can be found at:
- National Organization for Rare Disorders (NORD) -- rarediseases.org/rare-diseases/peutz-jeghers-syndrome
- Genetic and Rare Diseases Information Center (GARD) -- rarediseases.info.nih.gov/diseases/7378/peutz-jeghers-syndrome
Outlook (Prognosis)
There may be a high risk for these polyps becoming cancerous. Some studies link PJS with cancers of the gastrointestinal tract, lung, breast, uterus, and ovaries.
Possible Complications
Complications may include:
- Intussusception
- Polyps that lead to cancer
-
Ovarian cysts
Ovarian cysts
An ovarian cyst is a sac filled with fluid that forms on or inside an ovary. This article is about cysts that form during your monthly menstrual cycl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - A type of ovarian tumors called sex cord tumors
When to Contact a Medical Professional
Contact your provider for an appointment if you or your child has symptoms of this condition. Severe abdominal pain may be a sign of an emergency condition such as intussusception.
Prevention
Genetic counseling is recommended if you are planning to have children and have a family history of this condition.
Reviewed By
Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Garber JJ, Chung DC. Colonic polyps and polyposis syndromes. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 126.
McGarrity TJ, Amos CI, Baker MJ. Peutz-Jeghers syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews. Seattle, WA: University of Washington. www.ncbi.nlm.nih.gov/books/NBK1266/. Updated September 2, 2021. Accessed April 18, 2024.
Zahler SG, Kabbany MN, Murray KF. Tumors of the digestive tract. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 393.
Disclaimer



 All rights reserved.
All rights reserved.