Pneumomediastinum
Mediastinal emphysemaPneumomediastinum is air in the mediastinum. The mediastinum is the space in the middle of the chest, between the lungs and around the heart.
Causes
Pneumomediastinum is uncommon. The condition can be caused by injury or disease. Most often, it occurs when air leaks from any part of the lung or airways into the mediastinum.
Increased pressure in the lungs or airways may be caused by:
- Too much coughing
- Repeated bearing down to increase abdominal pressure (such as pushing during childbirth or a bowel movement)
- Sneezing
- Vomiting
It may also happen after:
- An infection in the neck or center of the chest
- Rapid rises in altitude, or scuba diving
- Tearing of the esophagus (the tube that connects the mouth and stomach)
- Tearing of the trachea (windpipe)
- Use of a breathing machine (ventilator)
Ventilator
A ventilator is a machine that breathes for you or helps you breathe. It is also called a breathing machine or respirator. The ventilator: Is attac...
Read Article Now Book Mark Article - Use of inhaled recreational drugs, such as marijuana or crack cocaine
- Surgery
- Trauma to the chest
Pneumomediastinum also can occur with collapsed lung (pneumothorax) or other diseases.
Pneumothorax
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung between the lung and chest wall. This buil...

Symptoms
There may be no symptoms. The condition usually causes chest pain behind the breastbone, which may spread to the neck or arms. The pain may be worse when you take a breath or swallow.
Exams and Tests
During a physical exam, your health care provider may feel small bubbles of air under the skin of the chest, arms, or neck (called subcutaneous emphysema).
A chest x-ray or CT scan of the chest may be done. This is to confirm that air is in the mediastinum, and to help diagnose a hole in the trachea or esophagus.
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.

CT scan of the chest
A chest CT (computed tomography) scan is an imaging method that uses x-rays to create cross-sectional pictures of the chest and upper abdomen....

When examined, sometimes the person can look very puffy (swollen) in the face and eyes. This can look worse than it actually is.
Treatment
Often, no treatment is needed because the body will gradually absorb the air. Breathing high concentrations of oxygen may speed this process.
The provider may put in a chest tube if you also have a collapsed lung. You may also need treatment for the cause of the problem. A hole in the trachea or esophagus needs to be repaired with surgery.
Chest tube
A chest tube is a hollow, flexible tube placed into the chest. It acts as a drain. Chest tubes drain blood, fluid, or air from around your lungs, he...

Outlook (Prognosis)
The outlook depends on the disease or events that caused the pneumomediastinum.
Possible Complications
Air may build up and enter the space around the lungs (pleural space), causing the lung to collapse.
In rare cases, air may enter the area between the heart and the thin sac that surrounds the heart. This condition is called a pneumopericardium.
In other rare cases, so much air builds up in the middle of the chest that it pushes on the heart and the great blood vessels, so they cannot work properly.
All of these complications require urgent attention because they can be life threatening.
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number if you have severe chest pain or difficulty breathing.
References
McCool FD. Diseases of the diaphragm, chest wall, pleura, and mediastinum. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 86.
Vemana AP, Haider SK. Pneumomediastinum. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 462.
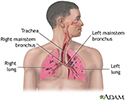
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Review Date: 8/19/2024
Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.