Idiopathic pulmonary fibrosis
Idiopathic diffuse interstitial pulmonary fibrosis; IPF; Pulmonary fibrosis; Cryptogenic fibrosing alveolitis; CFA; Fibrosing alveolitis; Usual interstitial pneumonitis; UIPIdiopathic pulmonary fibrosis (IPF) is scarring or thickening of the lungs without a known cause.
Causes
Health care providers do not know what causes IPF or why some people develop it. Idiopathic means the cause is not known. The condition may be due to the lungs responding to an unknown substance or injury. Genes may play a role in developing IPF. The disease occurs most often in people between 60 and 70 years old. IPF is more common in men than women.
Symptoms
When you have IPF, your lungs become scarred and stiffened. This makes it hard for you to breathe. In most people, IPF gets worse quickly over months or a few years. In others, IPF worsens over a much longer time.
Symptoms may include any of the following:
- Chest pain (sometimes)
- Cough (usually dry)
- Not able to be as active as before
-
Shortness of breath during activity (this symptom lasts for months or years, and over time may also occur when at rest)
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Feeling faint
- Gradual weight loss
Exams and Tests
Your provider will do a physical exam and ask about your medical history. You will be asked whether you have been exposed to asbestos or other toxins and if you have been a smoker.
The physical exam may find that you have:
- Abnormal breath sounds called crackles (sounds like Velcro being pulled apart)
-
Bluish skin (cyanosis) around the mouth or fingernails due to low oxygen (with advanced disease)
Bluish skin
A bluish color to the skin or mucous membrane is usually due to a lack of oxygen in the blood. The medical term is cyanosis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Enlargement and curving of the fingernail bases, called clubbing
Tests that help diagnose IPF include the following:
-
Bronchoscopy
Bronchoscopy
Bronchoscopy is a test to view the airways and diagnose lung disease. It may also be used during the treatment of some lung conditions.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
High resolution chest CT scan (HRCT)
Chest CT scan
A chest CT (computed tomography) scan is an imaging method that uses x-rays to create cross-sectional pictures of the chest and upper abdomen....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Echocardiogram
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Measurements of blood oxygen level (arterial blood gases)
Blood oxygen level
Blood gases are a measurement of how much oxygen and carbon dioxide are in your blood. They also determine the acidity (pH) of your blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pulmonary function tests
Pulmonary function tests
Pulmonary function tests are a group of tests that measure breathing and how well the lungs are functioning.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - 6-minute walk test
- Tests for autoimmune diseases such as rheumatoid arthritis, lupus, or scleroderma
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleLupus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the immune system of the body mistakenly attacks healthy tissue. It c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleScleroderma
Scleroderma is a disease that involves the buildup of fibrous tissue in the skin and elsewhere in the body. It also damages the cells that line the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Open lung (surgical) biopsy
Treatment
There is no known cure for IPF.
Treatment is aimed at relieving symptoms and slowing disease progression:
- Pirfenidone (Esbriet) and nintedanib (Ofev) are two medicines that are used to treat people with IPF. They may help slow lung damage.
- People with low blood oxygen levels will need oxygen support at home.
Oxygen support
Because of your medical problem, you may need to use oxygen to help you breathe. You will need to know how to use and store your oxygen.
Read Article Now Book Mark Article - Lung rehabilitation will not cure the disease, but it can help people exercise with less difficulty breathing.
Making home and lifestyle changes can help manage breathing symptoms. If you or any family members smoke, now is the time to stop.
Home and lifestyle changes
You were in the hospital to treat your breathing problems that are caused by interstitial lung disease. This disease scars your lungs, which makes i...
Read Article Now Book Mark ArticleTime to stop
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...

A lung transplant may be considered for some people with advanced IPF.
Lung transplant
Lung transplant is surgery to replace one or both diseased lungs with healthy lungs from a human donor.

Support Groups
You can ease the stress of illness by joining a support group. Sharing with others who have common experiences and problems can help you not feel alone.
More information and support for people with IPF and their families can be found at:
- Pulmonary Fibrosis Foundation -- www.pulmonaryfibrosis.org/patients-caregivers/medical-and-support-resources/find-a-support-group
- American Lung Association -- www.lung.org/better-breathers
Outlook (Prognosis)
IPF may improve or stay stable for a long time with or without treatment. Most people get worse, even with treatment.
When breathing symptoms become more severe, you and your provider should discuss treatments that prolong life, such as lung transplantation. Also discuss advance care planning.
Treatments that prolong life
Sometimes after injury or a long illness, the main organs of the body no longer work properly without support. Your health care provider may tell yo...
Read Article Now Book Mark ArticleAdvance care planning
When you are very ill or injured, you may not be able to make health care choices for yourself. If you are unable to speak for yourself, your health...

Possible Complications
Complications of IPF may include:
- Abnormally high levels of red blood cells due to low blood oxygen levels
-
Collapsed lung
Collapsed lung
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung between the lung and chest wall. This buil...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High blood pressure in the arteries of the lungs
- Respiratory failure
-
Cor pulmonale (right-sided heart failure)
Cor pulmonale
Cor pulmonale is a condition that causes the right side of the heart to fail. Long-term high blood pressure in the pulmonary arteries of the lung an...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Death
When to Contact a Medical Professional
Contact your provider right away if you have any of the following:
- Breathing that is harder, faster, or shallower (you are unable to take a deep breath)
- Need to lean forward when sitting to breathe comfortably
- Frequent headaches
- Sleepiness or confusion
- Fever
- Dark mucus when you cough
- Blue fingertips or skin around your fingernails
References
National Heart, Lung, and Blood Institute website. Idiopathic pulmonary fibrosis. www.nhlbi.nih.gov/health/idiopathic-pulmonary-fibrosis. Updated June 26, 2023. Accessed May 14, 2024.
Raghu G, Martinez FJ. Interstitial lung disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 80.
Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am J Respir Crit Care Med. 2022;205(9):e18-e47. PMID: 35486072 pubmed.ncbi.nlm.nih.gov/35486072/.
Ryu JH, Selman M, Lee JS, Colby TV, King TE. Idiopathic pulmonary fibrosis. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 89.
Silhan LL, Danoff SK. Nonpharmacologic therapy for idiopathic pulmonary fibrosis. In: Collard HR, Richeldi L, eds. Interstitial Lung Disease. Philadelphia, PA: Elsevier; 2018:chap 5.
-
Spirometry - illustration
Spirometry is a painless study of air volume and flow rate within the lungs. Spirometry is frequently used to evaluate lung function in people with obstructive or restrictive lung diseases such as asthma or cystic fibrosis.
Spirometry
illustration
-
Clubbing - illustration
Clubbing may result from chronic low blood-oxygen levels. This can be seen with cystic fibrosis, congenital cyanotic heart disease, and several other diseases. The tips of the fingers enlarge and the nails become extremely curved from front to back.
Clubbing
illustration
-
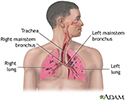
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Spirometry - illustration
Spirometry is a painless study of air volume and flow rate within the lungs. Spirometry is frequently used to evaluate lung function in people with obstructive or restrictive lung diseases such as asthma or cystic fibrosis.
Spirometry
illustration
-
Clubbing - illustration
Clubbing may result from chronic low blood-oxygen levels. This can be seen with cystic fibrosis, congenital cyanotic heart disease, and several other diseases. The tips of the fingers enlarge and the nails become extremely curved from front to back.
Clubbing
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Review Date: 5/3/2024
Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.