Skin flaps and grafts - self-care
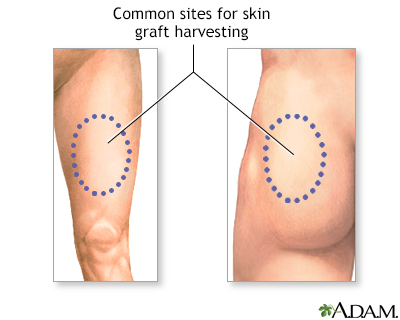
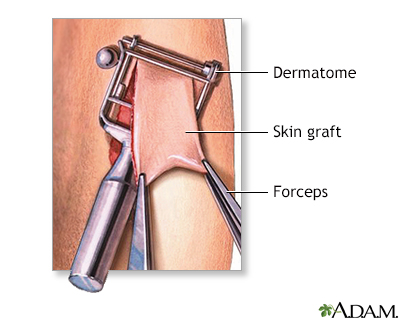
A skin graft is a piece of healthy skin removed from one area of your body to repair damaged or missing skin somewhere else on your body. This skin does not have its own source of blood flow.
Skin graft
A skin graft is a patch of skin that is removed by surgery from one area of the body and transplanted, or attached, to another area.

Learning how to care for skin flaps and grafts can help them heal more quickly and reduce scarring.
Why Skin Flap or Graft Surgery is Performed
A skin flap is healthy skin and tissue that is partly detached and moved to cover a nearby wound.
- A skin flap may contain skin and fat, or skin, fat, and muscle.
- Often, a skin flap is still attached to its original site at one end and remains connected to a blood vessel.
- Sometimes a flap is moved to a new site and the blood vessel is surgically reconnected. This is called a free flap.
Skin grafts are used to help more serious, larger and deeper wounds heal, including:
- Wounds that are too big to heal on their own
- Burns
Burns
Burns commonly occur by direct or indirect contact with heat, electric current, radiation, or chemical agents. Burns can lead to cell death, which c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Skin loss from a serious skin infection
- Surgery for skin cancer
- Venous ulcers, pressure ulcers, or diabetic ulcers that do not heal
Venous ulcers
Venous ulcers (open sores) can occur when the veins in your legs do not push blood back up to your heart as well as they should. Blood backs up in t...
Read Article Now Book Mark ArticlePressure ulcers
A pressure sore is an area of the skin that breaks down when something keeps rubbing or pressing against the skin.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - After mastectomy or amputation
Mastectomy
A mastectomy is surgery to remove the breast tissue. Some of the skin and the nipple may also be removed. The surgery is most often done to treat b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleAmputation
Leg or foot amputation is the removal of a leg, foot or toes from the body. These body parts are called extremities. Amputations are done either by...
Read Article Now Book Mark Article
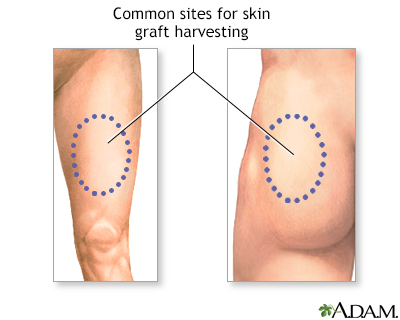
The area from where skin is taken is called the donor site. After surgery, you will have two wounds, the graft or flap itself and the donor site. Donor sites for grafts and flaps are chosen based on:
- How closely the skin matches the area of the wound
- How visible the scar will be from the donor site
- How close the donor site is to the wound
Often the donor site may be more painful after surgery than the wound due to newly exposed nerve endings.
Caring for Skin Flaps and Grafts
You will need to care for the flap or graft site as well as the donor site. When you come home after surgery, you will have a dressing on your wounds. The dressing does several things, including:
- Protect your wound from germs and reduce the risk of infection
- Protect the area as it heals
- Soak up any fluids that leak from your wound
To care for the graft or flap site:
- You may need to rest for several days after surgery as your wound heals.
- The type of dressing you have depends on the type of wound and where it is.
- Keep the dressing and area around it clean and free from dirt or sweat.
- Do not let the dressing get wet.
- Do not touch the dressing. Leave it in place for as long as your health care provider recommends (about 4 to 7 days).
- Take any medicines or pain relievers as directed.
- If possible, try to elevate the wound so it is above your heart. This helps reduce swelling. You may need to do this while sitting or lying down. You can use pillows to prop up the area.
- If your provider says it is OK, you may use an ice pack on the bandage to help with swelling. Ask how often you should apply the ice pack. Be sure to keep the bandage dry.
- Avoid any movement that might stretch or injure the flap or graft. Avoid hitting or bumping the area.
- You will need to avoid strenuous exercise for several days. Ask your provider for how long.
- If you have a vacuum dressing, you may have a tube attached to the dressing. If the tube falls off, contact your provider.
- You will probably see your provider to have your dressing changed in 4 to 7 days. You may need to have the dressing to your flap or graft site changed by your provider a couple times over 2 to 3 weeks.
- As the site heals, you may be able to care for it at home. Your provider will show you how to care for your wound and apply dressings.
- The site may become itchy as it heals. Do not scratch the wound or pick at it.
- After the site heals, apply SPF 30 or higher sunscreen to surgical sites if exposed to the sun.
To care for the donor site:
- Leave the dressing in place. Keep it clean and dry.
- Your provider will remove the dressing in about 4 to 7 days, or give you instructions for how to remove it.
- After the dressing is removed, you may be able to leave the wound uncovered. However, if it is in an area that is covered by clothing, you will want to cover the site to protect it. Ask your provider what type of dressing to use.
- Do not apply any lotions or creams to the wound unless your provider tells you to. As the area heals, it may itch and scabs may form. Do not pick scabs or scratch the wound as it heals.
Bathing or Showering
Your provider will let you know when it is OK to bathe after surgery. Keep in mind:
- You may need to take sponge baths for 2 to 3 weeks while your wounds are in the early stages of healing.
- Once you get the OK to bathe, showers are better than baths because the wound does not soak in water. Soaking your wound could cause it to reopen.
- Be sure to protect your dressings while you bathe to keep them dry. Your provider may suggest covering the wound with a plastic bag to keep it dry.
- If your provider gives the OK, gently rinse your wound with water as you bathe. Do not rub or scrub the wound. Your provider may recommend special cleansers to use on your wounds.
- Gently pat dry the area around your wound with a clean towel. Let the wound air dry.
- Do not use soaps, lotions, powders, cosmetics, or other skin care products on your wound unless told to do so by your provider.
At some point during the healing process, you will not need a dressing anymore. Your provider will tell you when you can leave your wound uncovered and how to care for it.
When to Call the Doctor
Contact your provider if:
- Pain gets worse or does not improve after taking pain relievers
- You have bleeding that won't stop after 10 minutes with gentle, direct pressure
- Your dressing becomes loose
- Edges of the graft or flap start to come up
- You feel something bulging out of the graft or flap site
Also contact your provider if you notice signs of an infection, such as:
- Increased drainage from the wound
- Drainage becoming thick, tan, green, or yellow, or smells bad (pus)
- Your temperature is above 100°F (37.8°C) for more than 4 hours
- Red streaks appear that lead away from the wound
Reviewed By
Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Padilla PL, Khoo KH, Ho T, Cole EL, Sirvent RZ, Philips LG. Plastic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 69.
Pettengill KM. Therapy management of complex injuries of the hand. In: Skirven TM, Osterman AL, Fedorczyk JM, Amadio PC, Feldscher SB, Shin EK, eds. Rehabilitation of the Hand and Upper Extremity. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 75.
Woelfel SL, Armstrong DG, Shin L. Wound care. In: Sidawy AN, Perler BA, eds. Rutherford’s Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 118.
Wysong A, Higgins S. Basic principles in flap reconstruction. In: Rohrer TE, Cook JL, Kaufman AJ, eds. Flaps and Grafts in Dermatologic Surgery. 2nd ed. Philadelphia, PA: Elsevier; 2018:chap 2.


 All rights reserved.
All rights reserved.