Delivery presentations
Pregnancy - delivery presentation; Labor - delivery presentation; Occiput posterior; Occiput anterior; Brow presentationDelivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
Your baby must pass through your pelvic bones to reach the vaginal opening. The ease at which this passage will take place depends on how your baby is positioned during delivery. The best position for the baby to be in to pass through the pelvis is with the head down and the front of the body facing towards the mother's back. This position is called occiput anterior (OA).
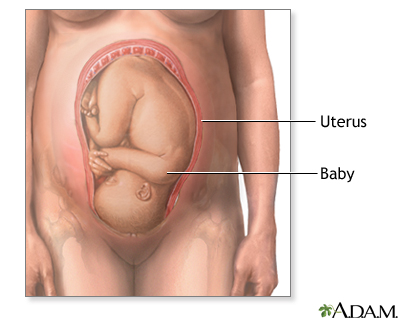
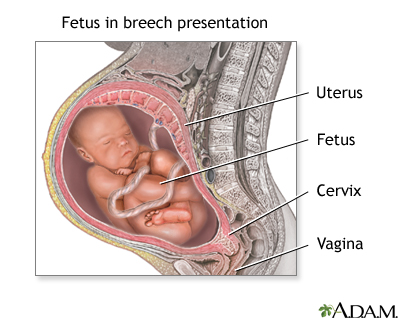
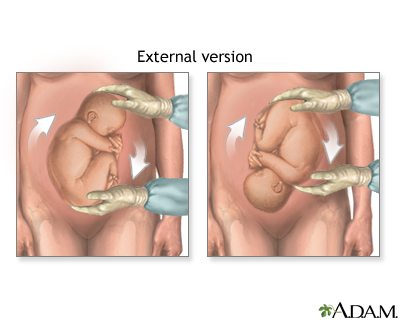
In breech position, the baby's bottom is facing down instead of the head. Your health care provider will most often detect this in an office visit before your labor begins. Most babies will be in the head-down position by about 34 weeks.
Part of your prenatal care after 34 weeks will involve making sure your baby is in the head-down position.
If your baby is breech, it is not safe to deliver vaginally. If your baby is not in a head-down position after your 36th week, your provider can explain your choices and their risks to help you decide what steps to take next.
Your choices and their risks
The best position for your baby inside your uterus at the time of delivery is head down. This position makes it easier and safer for your baby to pa...

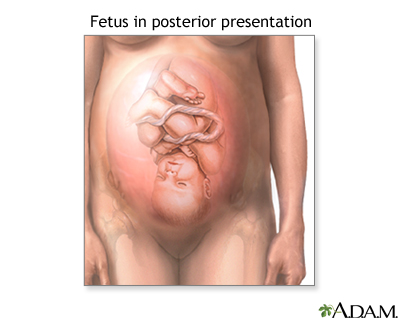
Occiput Posterior (OP)
In occiput posterior position, your baby's head is down, but it is facing the mother's front instead of her back.
It is safe to deliver a baby facing this way. But it is harder for the baby to get through the pelvis. If a baby is in this position, sometimes it will rotate around during labor so that the head stays down and the body faces the mother's back (OA position).
The mother can walk, rock, and try different delivery positions during labor to help encourage the baby to turn. If the baby does not turn, labor can take longer. Sometimes, the provider may use forceps or a vacuum device to help get the baby out. If the baby stays in the OP position during labor, you have a higher risk of needing to deliver your baby by cesarean delivery (C-section).
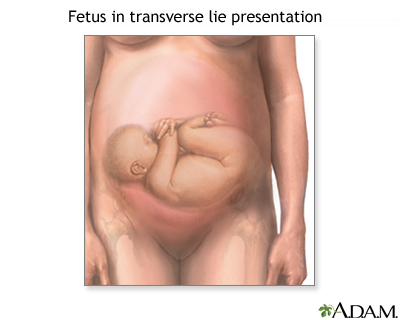
Transverse Position
A baby in the transverse position is sideways. Often, the shoulders or back are over the mother's cervix. This is also called the shoulder, or oblique, position.
The risk for having a baby in the transverse position increases if you:
- Go into labor early
- Have given birth 3 or more times
- Have placenta previa
Placenta previa
Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Unless your baby can be turned into head-down position, a vaginal birth will be too risky for you and your baby. A doctor will deliver your baby by cesarean birth (C-section).
C-section
A C-section is the delivery of a baby by making an opening in the mother's lower belly area. It is also called a cesarean delivery.

Less Common Presentations
With the brow-first position, the baby's head extends backward (like looking up), and the forehead leads the way. This position may be more common if this is not your first pregnancy.
- Your provider rarely detects this position before labor. An ultrasound may be able to confirm a brow presentation.
Ultrasound
A pregnancy ultrasound is an imaging test that uses sound waves to create a picture of how a baby is developing in the womb (uterus). It is also use...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - More likely, your provider will detect this position while you are in labor during an internal exam.
With face-first position, the baby's head is extended backwards even more than with brow first position.
- Most of the time, the force of contractions causes the baby to be in face-first position.
- It is also detected when labor does not progress.
In some of these presentations, a vaginal birth is possible, but labor will generally take longer. After delivery, the baby's face or brow will be swollen and may appear bruised. These changes will go away over the next few days.
References
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Thorp JM, Grantz KL. Clinical aspects of normal and abnormal labor. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 40.
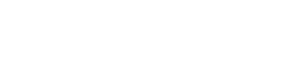
Delivery presentations - illustration
Cephalic (head first) presentation is considered normal, but a breech (feet or buttocks first) delivery can be very difficult, even dangerous for the mother and the baby.
Delivery presentations
illustration
Breech - series
Presentation
Review Date: 11/8/2024
Reviewed By: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.