Heart failure - surgeries and devices
CHF - surgery; Congestive heart failure - surgery; Cardiomyopathy - surgery; HF - surgery; Intra-aortic balloon pumps - heart failure; IABP - heart failure; Catheter based assist devices - heart failureThe main treatments for heart failure are making lifestyle changes and taking your medicines. However, there are procedures and surgeries that may help.
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...

Pacemakers and Defibrillators
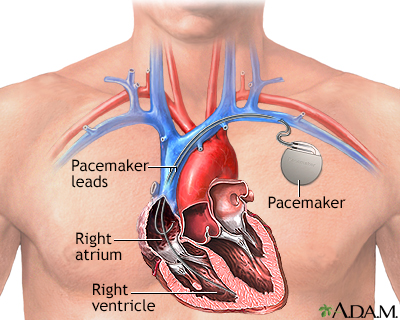
A heart pacemaker is a small, battery-operated device that sends a signal to your heart. The signal makes your heart beat at the correct pace.
Heart pacemaker
A pacemaker is a small, battery-operated device. This device senses when your heart is beating too slowly. It sends a signal to your heart that mak...

Pacemakers may be used:
- To correct abnormal heart rhythms. The heart may beat too slowly, too fast, or in an irregular manner.
- To better coordinate the beating of the heart in people with heart failure. These are called biventricular pacemakers.
When your heart is weakened, gets too large, and does not pump blood very well, you are at high risk for abnormal heartbeats that can lead to sudden cardiac death.
- An implantable cardioverter-defibrillator (ICD) is a device that detects heart rhythms. It quickly sends an electrical shock to the heart to change the rhythm back to normal.
Implantable cardioverter-defibrillator ...
An implantable cardioverter-defibrillator (ICD) is a device that detects a life-threatening, rapid heartbeat. This abnormal heartbeat is called an a...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Most biventricular pacemakers can also work as implantable cardio-defibrillators (ICD).
Procedures and Surgery to Improve Blood Supply to the Heart
The most common cause of heart failure is coronary artery disease (CAD), which is a narrowing of the small blood vessels that supply blood and oxygen to the heart. CAD may become worse and make it harder to manage your symptoms.
After performing certain tests, your health care provider may feel that opening a narrowed or blocked blood vessel will improve your heart failure symptoms. Suggested procedures may include:
Tests
The diagnosis of heart failure is made largely on a person's symptoms and a physical exam. However, there are many tests that can help give more inf...
Read Article Now Book Mark Article-
Angioplasty and stent placement
Angioplasty and stent placement
Angioplasty is a procedure to open narrowed or blocked blood vessels that supply blood to the heart. These blood vessels are called the coronary art...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart bypass surgery
Heart bypass surgery
Heart bypass surgery creates a new route, called a bypass, for blood and oxygen to go around a blockage to reach your heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Heart Valve Surgery
Blood that flows between the chambers of your heart, or out of your heart into the aorta, must pass through a heart valve. These valves open enough to allow blood to flow through. They then close, keeping blood from flowing backward.
When these valves do not work well (become too leaky or too narrow), blood does not flow correctly through the heart to the body. This problem may cause heart failure or make heart failure worse.
Heart valve surgery may be needed to repair or replace one of the valves.
Heart valve surgery
Heart valve surgery is used to repair or replace diseased heart valves. Blood that flows between different chambers of your heart must flow through a...

Surgery for End-stage Heart Failure
Some types of surgery are done for severe heart failure when other treatments no longer work. These procedures are often used when a person is waiting for a heart transplant. They are also sometimes used long term in cases when transplant is not planned or possible.
Heart transplant
A heart transplant is surgery to remove a damaged or diseased heart and replace it with a healthy donor heart.

Examples of some of these devices include left ventricular assist devices (LVAD), right ventricular assist devices (RVAD), or a total artificial hearts. They are considered for use if you have severe heart failure that cannot be controlled with medicine or a special pacemaker.
Left ventricular assist devices (LVAD)
Ventricular assist devices (VADs) help your heart pump blood from one of the main pumping chambers to the rest of your body or to the other side of t...

- Ventricular assist devices (VAD) help your heart pump blood from the pumping chambers of your heart to either the lungs or to the rest of your body These pumps may be implanted in your body or connected to a pump outside your body.
- You may be on a waiting list for a heart transplant. Some people who get a VAD are very ill and may already be on a heart-lung bypass machine.
- Total artificial hearts are being developed, but are not yet in wide use.
Devices inserted through a catheter such as intra-aortic balloon pumps (IABP) are sometimes used.
- An IABP is a thin balloon that is inserted into an artery (most often in the leg) and threaded into the main artery exiting the heart (aorta).
- These devices can help maintain heart function in the short term. Because they can be placed quickly, they are useful for people who have a sudden and severe decline in heart function
- They are used in people who are waiting for recovery or for more advanced assist devices.
References
Aaronson KD, Pagani FD. Mechanical circulatory support. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 59.
Ewald GA, Milano CA, Rogers JG. Circulatory assist devices in heart failure. In: Felker GM, Mann DL, eds. Heart Failure: A Companion to Braunwald's Heart Disease. 4th ed. Philadelphia, PA: Elsevier, 2020:chap 45.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2023;81(15):1551. PMID: 35379503 pubmed.ncbi.nlm.nih.gov/35379503/.
Mann DL. Management of heart failure patients with reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 50.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021;143(10):e784. PMID: 33332149 pubmed.ncbi.nlm.nih.gov/33332149/.
Rihal CS, Naidu SS; Society for Cardiovascular Angiography and Interventions (SCAI), et al. 2015 SCAI/ACC/HFSA/STS clinical expert consensus statement on the use of percutaneous mechanical circulatory support devices in cardiovascular care: Endorsed by the American Heart Association, the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia Intervencion; affirmation of value by the Canadian Association of Interventional Cardiology-Association Canadienne de Cardiologie d'intervention. J Am Coll Cardiol. 2015;65(19):e7-26. PMID: 25861963 pubmed.ncbi.nlm.nih.gov/25861963/.
-
Pacemaker - illustration
A pacemaker is a small, battery-operated electronic device which is inserted under the skin to help the heart beat regularly and at an appropriate rate. The pacemaker has leads that travel through a large vein to the heart, where the wires are anchored. The leads send the electrical impulses to the heart to tell it to beat.
Pacemaker
illustration
-
Pacemaker - illustration
A pacemaker is a small, battery-operated electronic device which is inserted under the skin to help the heart beat regularly and at an appropriate rate. The pacemaker has leads that travel through a large vein to the heart, where the wires are anchored. The leads send the electrical impulses to the heart to tell it to beat.
Pacemaker
illustration
-
Heart attack and acute coronary syndrome - InDepth
(In-Depth)
-
Rheumatoid arthritis
(Alt. Medicine)
-
Weight control and diet - InDepth
(In-Depth)
-
Erectile dysfunction - InDepth
(In-Depth)
-
Gastroesophageal reflux disease and heartburn - InDepth
(In-Depth)
-
Breast cancer - InDepth
(In-Depth)
Review Date: 4/10/2023
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.