Pulmonary hypertension - at home
Pulmonary hypertension - self-care; Activity - pulmonary hypertension; Preventing infections - pulmonary hypertension; Oxygen - pulmonary hypertensionPulmonary hypertension (PAH) is abnormally high blood pressure in the arteries of the lungs. With PAH, the right side of the heart has to work harder than normal.
Pulmonary hypertension
Pulmonary hypertension is high blood pressure in the arteries of the lungs. It makes the right side of the heart work harder than normal.

As the illness gets worse, you will need to do more to take care of yourself. You will also need to make changes in your home and get more help around the house.
Keep Active
Try walking to build up strength:
- Ask your health care provider or respiratory therapist how far to walk.
- Slowly increase how far you walk.
- Try not to talk when you walk so you do not get out of breath.
- Stop if you have chest pain or feel dizzy.
Ride a stationary bike. Ask your provider or respiratory therapist how long and how hard to ride.
Get stronger even when you are sitting:
- Use small weights or rubber tubing to make your arms and shoulders stronger.
- Stand up and sit down several times.
- Raise your legs straight out in front of you. Hold for a few seconds, then lower them back down.
- Stop if you have chest pain or feel dizzy.
Self-care
Other tips for self-care include:
- Try to eat 5 to 6 small meals a day. It might be easier to breathe when your stomach is not full.
- Do not drink a lot of liquid before or while eating your meals.
- Ask your provider what foods to eat to get more energy.
Foods to eat to get more energy
If you are sick or undergoing cancer treatment, you may not feel like eating. But it is important to get enough protein and calories so you do not l...
Read Article Now Book Mark Article - If you smoke, now is the time to quit. Stay away from smokers when you are out. Do not allow smoking in your home.
Now is the time to quit
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Stay away from strong odors and fumes.
- Ask your provider or respiratory therapist which breathing exercises are good for you.
- Take all the medicines that your provider prescribed for you.
- Talk to your provider if you feel depressed or anxious.
- Tell your provider if you are becoming dizzy or have a lot more swelling in your legs.
Stay Away From Infections
You should:
- Get a flu shot every year and other recommended vaccines (like the COVID-19 vaccine). Ask your provider if you should get a pneumonia (pneumococcal) vaccine.
Flu shot
All content below is taken in its entirety from the CDC Inactivated Influenza Vaccine Information Statement (VIS) www. cdc. gov/vaccines/hcp/vis/vis-...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCOVID-19 vaccine
COVID-19 vaccines are used to prepare the body's immune system to protect against COVID-19. Everyone ages 6 months and older should get a 2023-2024 u...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticlePneumonia (pneumococcal) vaccine
All content below is taken in its entirety from the CDC Information Statement (VIS): www. cdc. gov/vaccines/hcp/vis/vis-statements/pcv. html
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Wash your hands often. Always wash them after you go to the bathroom and when you are around people who are sick.
Wash your hands often
Washing your hands often during the day is an important way to help reduce the spread of germs and prevent illness. Learn when you should wash your ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Stay away from crowds.
- Ask visitors with colds to wear masks, or to visit you after their colds are gone.
Around the Home
Make it easier for yourself at home.
- Put items you use often in spots where you do not have to reach or bend over to get them.
- Use a cart with wheels to move things around the house.
- Use an electric can opener, dishwasher, and other things that will make your chores easier to do.
- Use cooking tools (knives, peelers, and pans) that are not heavy.
To save your energy:
- Use slow, steady motions when you are doing things.
- Sit down if you can when you are cooking, eating, dressing, and bathing.
- Get help for harder tasks.
- Do not try to do too much in one day.
- Keep the phone with you or near you.
- Wrap yourself in a towel rather than drying off.
- Try to reduce stress in your life.
Going Home with Oxygen
In the hospital, you received oxygen treatment. You may need to use oxygen at home. Do not change how much oxygen is flowing without asking your provider.
Use oxygen at home
Because of your medical problem, you may need to use oxygen to help you breathe. You will need to know how to use and store your oxygen.
Have a backup supply of oxygen at home or with you when you go out. Keep the phone number of your oxygen supplier with you at all times. Learn how to use oxygen safely at home.
How to use oxygen safely
Oxygen makes things burn much faster. Think of what happens when you blow into a fire; it makes the flame bigger. If you are using oxygen in your h...
If you check your oxygen with an oximeter at home and your number often drops below 90%, call your provider. If you check your oxygen during activity, it should be above or at 90% almost all the time. If not, call your provider.
Make sure you have enough supply of your medicines. Abruptly stopping them can lead to serious illness.
Follow-up
Your hospital provider may ask you to make a follow-up visit with:
- Your primary care provider
- Your lung doctor (pulmonologist) or your heart doctor (cardiologist)
- Someone who can help you stop smoking, if you smoke
When to Call the Doctor
Call your provider if your breathing is:
- Getting harder
- Faster than before
- Shallow, or you cannot get a deep breath
Also call your provider if:
- You need to lean forward when sitting, to breathe more easily
- You feel sleepy or confused
- You have a fever
- Your fingertips, or the skin around your fingernails, are blue
- You feel dizzy, pass out (syncope), or have chest pain
- You have increased leg swelling
References
Lammi MR, Mathai SC. Pulmonary hypertension: general approach. In: Broaddus VC, King TE, Ernst JD, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 83.
Maron BA. Pulmonary hypertension. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 88.
-
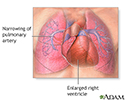
Primary pulmonary hypertension - illustration
Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance. Some symptoms include chest pain, weakness, shortness of breath, and fatigue. The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
Primary pulmonary hypertension
illustration
-
Primary pulmonary hypertension - illustration
Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance. Some symptoms include chest pain, weakness, shortness of breath, and fatigue. The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
Primary pulmonary hypertension
illustration
Review Date: 5/3/2023
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.