Hysterectomy - vaginal - discharge
Vaginal hysterectomy - discharge; Laparoscopically assisted vaginal hysterectomy - discharge; LAVH - dischargeYou were in the hospital to have a vaginal hysterectomy. This article tells you what to expect and how to care for yourself when you return home after the procedure.
When You're in the Hospital
While you were in the hospital, you had a vaginal hysterectomy. Your surgeon made a cut in your vagina. Your uterus was removed through this cut.
Hysterectomy
Hysterectomy is surgery to remove a woman's womb (uterus). The uterus is a hollow muscular organ that nourishes the developing baby during pregnancy...

Your surgeon may have also used a laparoscope (a thin tube with a small camera on it) and other instruments that were inserted into your belly through several small incisions.
Part or all of your uterus was removed. Your fallopian tubes or ovaries may have also been removed. You may go home on the same day as surgery, or you may spend 1 to 2 nights in the hospital.
What to Expect at Home
It will take at least 3 to 6 weeks to feel better. You will have the most discomfort during the first 2 weeks. Most women will need to use pain medicine regularly and limit their activities during the first 2 weeks. After this period, you may feel tired but will not have much pain. You may not feel like eating much.
You will not have any scars on your skin unless your doctor used a laparoscope and other instruments that were inserted through your belly. In that case, you will have 2 to 4 scars less than 1-inch (3 cm) long.
You will likely have light spotting for 2 to 4 weeks. It may be pink, red, or brownish. It should not have a bad odor.
If you had good sexual function before the surgery, you should continue to have good sexual function afterward. If you had severe bleeding before your hysterectomy that also negatively affected sexual function, your sexual function will often improve after surgery. If you have a decrease in your sexual function after your hysterectomy, talk with your health care provider about possible causes and treatments.
Self-care
Slowly increase how much activity you do every day. Take short walks and increase how far you go gradually. Do not jog, do sit-ups, or other sports until you have checked with your provider.
Do not lift anything heavier than a gallon (3.8 L) jug of milk for a few weeks after surgery. Do not drive for the first 2 weeks.
Do not put anything into your vagina for the first 8 to 12 weeks. This includes douching or using tampons.
Do not start having sexual intercourse for at least 8 weeks, and only after your provider says it is OK. If you had vaginal repairs along with your hysterectomy, you may need to wait 12 weeks for intercourse. Check with your provider.
If your surgeon also used a laparoscope:
- You may remove the wound dressings and take a shower the day after surgery if sutures (stitches), staples, or glue were used to close your skin.
- Cover your wounds with plastic wrap before showering for the first week if tape strips (Steri-Strips) were used to close your skin. Do not try to wash the Steri-Strips off. They should fall off in about a week. If they are still in place after 10 days, remove them unless your doctor tells you not to.
- Do not soak in a bathtub or hot tub, or go swimming, until your doctor tells you it is OK.
Try eating smaller meals than normal and have healthy snacks in between. Eat plenty of fruits and vegetables and drink 8 cups (2 L) of water a day to keep from getting constipated.
To manage your pain:
- Your provider will prescribe pain medicines to use at home.
- If you are taking pain pills 3 or 4 times a day, try taking them at the same times each day for 3 to 4 days. They may work better to relieve the pain this way.
- Try getting up and moving around if you are having some pain in your belly. This may ease your pain.
When to Call the Doctor
Call your provider if:
- You have a fever above 100.5°F (38°C).
- Your surgical wound is bleeding, is red and warm to touch, or has thick, yellow, or green drainage.
- Your pain medicine is not helping your pain.
- It is hard to breathe.
- You have a cough that does not go away.
- You cannot drink or eat.
- You have nausea or vomiting.
- You are unable to pass gas or have a bowel movement.
- You have pain or burning when you urinate, or you are unable to urinate.
- You have a discharge from your vagina that has a bad odor.
- You have bleeding from the vagina that is heavier than light spotting.
- You have swelling or redness in one of your legs.
References
Gambone JC. Gynecologic procedures: imaging studies and surgery. In: Hacker NF, Gambone JC, Hobel CJ, eds. Hacker & Moore's Essentials of Obstetrics and Gynecology. 6th ed. Philadelphia, PA: Elsevier; 2016:chap 31.
Prescott LS, Yunker AC, Alvarez R, Jones HW. Gynecologic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 71.
Thurston J, Murji A, Scattolon S, et al. No. 377 – Hysterectomy for benign gynaecologic indications. Journal of Obstetrics and Gynaecology Canada (JOCG). 2019;41(4):543-557. PMID: 30879487 pubmed.ncbi.nlm.nih.gov/30879487/.
-
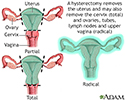
Hysterectomy - illustration
Hysterectomy is surgical removal of the uterus, resulting in inability to become pregnant. This surgery may be done for a variety of reasons including, but not restricted to, chronic pelvic inflammatory disease, uterine fibroids and cancer. A hysterectomy may be done through an abdominal or a vaginal incision.
Hysterectomy
illustration
-
Hysterectomy - illustration
Hysterectomy is surgical removal of the uterus, resulting in inability to become pregnant. This surgery may be done for a variety of reasons including, but not restricted to, chronic pelvic inflammatory disease, uterine fibroids and cancer. A hysterectomy may be done through an abdominal or a vaginal incision.
Hysterectomy
illustration
-
Uterine fibroids and hysterectomy - InDepth
(In-Depth)
-
Cervical cancer - InDepth
(In-Depth)
-
Menopause - InDepth
(In-Depth)
-
Menstrual disorders - InDepth
(In-Depth)
-
Breast cancer - InDepth
(In-Depth)
Review Date: 4/19/2022
Reviewed By: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.