Heart failure - home monitoring
HF - home monitoring; CHF - home monitoring; Cardiomyopathy - home monitoringHeart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptoms to occur throughout the body. Watching out for the warning signs that your heart failure is getting worse may help you catch problems before they become too serious.
What to Expect at Home
Knowing your body and the symptoms that tell you your heart failure is getting worse will help you stay healthier and out of the hospital. At home, you should watch for changes in your:
- Blood pressure
- Heart rate
- Pulse
- Weight
By watching out for warning signs, you can catch problems before they get too serious. Sometimes these simple checks will remind you that you forgot to take a pill, or that you have been drinking too much fluid or eating too much salt.
Be sure to write down the results of your home self-checks so that you can share them with your health care provider. Your provider's office may have a "telemonitor," a device you can use to send your information automatically. A nurse will go over your self-check results with you in a regular (sometimes weekly) phone call.
Throughout the day, ask yourself:
- Is my energy level normal?
- Am I getting more short of breath when I am doing my everyday activities?
- Are my clothes or shoes feeling tight?
- Are my ankles or legs swelling?
- Am I coughing more often? Does my cough sound wet?
- Do I get short of breath at night?
These are signs that there is too much fluid building up in your body. You will need to learn how to limit your fluids and salt intake to prevent these things from happening.
Your fluids
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes fluid t...
Salt intake
Too much sodium in your diet can be bad for you. If you have high blood pressure or heart failure, you may be asked to limit the amount of salt (whi...

Checking Your Weight
You will get to know what weight is right for you. Weighing yourself will help you know if there is too much fluid in your body. You might also find that your clothes and shoes are feeling tighter than normal when there is too much fluid in your body.
Weigh yourself every morning on the same scale when you get up -- before you eat and after you use the bathroom. Make sure you are wearing similar clothing each time you weigh yourself. Write down your weight every day on a chart so that you can keep track of it.
Contact your provider if your weight goes up by more than 2 to 3 pounds (1 to 1.5 kilograms, kg) in a day or 5 pounds (2 kilograms) in a week. Also contact your provider if you lose a lot of weight.
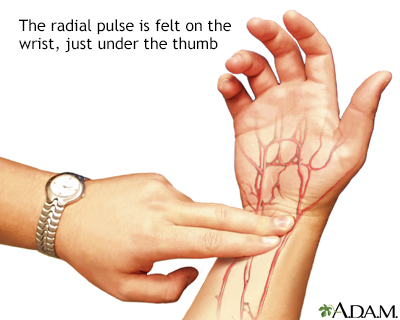
Checking Your Heart Rate and Pulse
Know what your normal pulse rate is. Your provider will tell you what yours should be.
You can take your pulse in the wrist area below the base of your thumb. Use your index and third fingers of your other hand to find your pulse. Use a second hand and count the number of beats for 30 seconds. Then double that number. That is your pulse.
Your provider may give you special equipment to check your heart rate.
Checking Your Blood Pressure
Your provider may ask you to keep track of your blood pressure at home. Make sure you get a good quality, well-fitting home device. Show it to your provider or nurse. It will probably have a cuff with a stethoscope or a digital readout.
Practice with your provider to make sure you are taking your blood pressure correctly.
When to Call the Doctor
Contact your provider if:
- You are tired or weak.
- You feel short of breath when you are active or when you are at rest.
- You have shortness of breath when you lie down, or an hour or two after falling asleep.
- You are wheezing and having trouble breathing.
- You have a cough that does not go away. It may be dry and hacking, or it may sound wet and bring up pink, foamy spit.
- You have swelling in your feet, ankles, or legs.
- You have to urinate a lot, particularly at night.
- You have gained or lost weight.
- You have pain or tenderness in your belly.
- You have symptoms you think might be from your medicines.
- Your pulse or heartbeat gets very slow or very fast, or it is not regular.
- Your blood pressure is lower or higher than is normal for you.
References
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
Heidenreich PA, Bozkurt B, Aguilar D, 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;146(13):e185. PMID: 35363499 pubmed.ncbi.nlm.nih.gov/35363499/.
Lam CSP, Shah SJ, Solomon SD. Heart failure with preserved and mildly reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 51.
Mann DL. Management of heart failure patients with reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 50.
-
Radial pulse - illustration
Arteries carry oxygenated blood away from the heart to the tissues of the body. Veins carry blood depleted of oxygen from the same tissues back to the heart. The arteries are the vessels with the pulse, a rhythmic pushing of the blood in the heart followed by a refilling of the heart chamber. To determine heart rate, one counts the beats at a pulse point like the inside of the wrist for 10 seconds, and multiplies this number by 6. This is the per-minute total.
Radial pulse
illustration
-
Radial pulse - illustration
Arteries carry oxygenated blood away from the heart to the tissues of the body. Veins carry blood depleted of oxygen from the same tissues back to the heart. The arteries are the vessels with the pulse, a rhythmic pushing of the blood in the heart followed by a refilling of the heart chamber. To determine heart rate, one counts the beats at a pulse point like the inside of the wrist for 10 seconds, and multiplies this number by 6. This is the per-minute total.
Radial pulse
illustration
Review Date: 7/14/2024
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.