Birth control - slow release methods
Contraception - slow-release hormonal methods; Progestin implants; Progestin injections; Skin patch; Vaginal ringCertain birth control methods contain man-made forms of hormones. The natural forms of these hormones are normally made in a woman's ovaries. These hormones are called estrogen and progestin.
Both of these hormones prevent a woman's ovaries from releasing an egg. The release of an egg during menstrual cycle is called ovulation. They do this by changing the levels of the natural hormones the body makes.
Progestin also helps prevent sperm from entering the uterus by making the mucous around a woman's cervix thick and sticky.
Birth control pills are one way of receiving these hormones. They are only effective if taken daily, preferably at about the same time.
Birth control pills
Birth control pills (BCPs) contain man-made forms of 2 hormones called estrogen and progestin. These hormones are made naturally in a woman's ovarie...

There are other methods to prevent pregnancy. The same hormones may be used but they are released slowly over time.
Information
PROGESTIN IMPLANTS
A progestin implant is a small rod that is implanted under the skin, most often on the inside of the arm. The rod releases a small amount of the progestin daily into the bloodstream.
It takes about a minute to insert the rod. The procedure is done using a local anesthetic in a doctor's office. The rod can stay in place for 3 years. However, it can be removed at any time. Removal usually takes only a few minutes.
After the implant has been inserted:
- You may have some bruising around the site for a week or more.
- You should be protected from getting pregnant within 1 week.
- You can use these implants while breastfeeding.
Progestin implants work better than birth control pills to prevent pregnancy. Very few women who use these implants are likely to get pregnant.
Your regular menstrual cycles should return within 3 to 4 weeks after these implants are removed.
PROGESTIN INJECTIONS
Injections or shots that contain the hormone progestin also work to prevent pregnancy. A single shot works for up to 90 days. These injections are given into the muscles of the upper arm or buttocks.
Side effects that may occur include:
- Changes in menstrual cycles or extra bleeding or spotting. Around one half of women who use these injections have no menstrual cycles.
- Breast tenderness, weight gain, headaches, or depression.
Depression
Depression may be described as feeling sad, blue, unhappy, miserable, or down in the dumps. Most of us feel this way at one time or another for shor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Progestin injections work better than birth control pills to prevent pregnancy. Very few women who use progestin injections are likely to get pregnant.
Sometimes the effects of these hormone shots last longer than 90 days. If you are planning to become pregnant in the near future, you might want to consider a different birth control method.
SKIN PATCH
The skin patch is placed on your shoulder, buttocks, or another area of your body. A new patch is applied once a week for 3 weeks. Then you go 1 week without a patch.
Estrogen levels are higher with the patch than with birth control pills or the vaginal ring. Because of this, there may be an increased risk for blood clots in the legs or lungs with this method. The FDA has issued a warning about the patch and the higher risk for a blood clot traveling to a lung.
Blood clots in the legs
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. DVT mainly affects the large...

Lungs
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.

The patch slowly releases both estrogen and progestin into your blood. Your health care provider will prescribe this method for you.
The patch works better than birth control pills to prevent pregnancy. Very few women who use the patch are likely to get pregnant.
The skin patch contains estrogen. Along with the higher risk for blood clots, there is a rare risk for high blood pressure, heart attack, and stroke. Smoking increases these risks even more.
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...

VAGINAL RING
The vaginal ring is a flexible device. This ring is about 2 inches (5 cm) wide and is placed into the vagina. It releases the hormones progestin and estrogen.
- Your provider will prescribe this method, but you will insert the ring yourself.
- It will stay in the vagina for 3 weeks. At the end of the third week, you will take the ring out for 1 week. DO NOT remove the ring until the end of the 3 weeks.
Side effects with the ring may include:
- Nausea and breast tenderness, which are less severe than with birth control pills or patches.
- Vaginal discharge or vaginitis.
Vaginal discharge
Vaginal discharge refers to secretions from the vagina. The discharge may be:Thick, pasty, or thinClear, cloudy, bloody, white, yellow, or greenOdor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Breakthrough bleeding and spotting (may occur more often than with birth control pills).
The vaginal ring contains estrogen. As a result, there is a rare risk for high blood pressure, blood clots, heart attack, and stroke. Smoking increases these risks even more.
The vaginal ring slowly releases both estrogen and progestin into your blood.
The vaginal ring works better than birth control pills to prevent pregnancy. Very few women who use the vaginal ring is likely to get pregnant.
HORMONE-RELEASING IUDS
An intrauterine device (IUD) is a small plastic T-shaped device used for birth control. It is inserted into the uterus. IUDs prevent sperm from fertilizing an egg.
IUD
An intrauterine device (IUD) is a small plastic T-shaped device used for birth control. It is inserted into the uterus where it stays to prevent pre...
Read Article Now Book Mark ArticleA newer type of IUD releases a low dose of a hormone into the uterus each day for a period of 3 to 5 years. This increases the effectiveness of the device as a birth control method. It also has the added benefits of reducing or stopping menstrual flow. It may help protect against cancer (endometrial cancer) in women who are at risk of developing the disease. There are several different IUDs of this type. Some are specially shaped for women who have never been pregnant.
You have choices for what type of IUD to have. Talk with your provider about which type may be best for you.
Type may be best for you
An intrauterine device (IUD) is a small, plastic, T-shaped device used for birth control. It is inserted into the uterus where it stays to prevent p...

References
Allen RH, Kaunitz AM, Hickey M, Brennan A. Hormonal contraception. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 18.
American College of Obstetricians and Gynecologists website. Combined hormonal birth control: pill, patch, and ring, FAQ 185. www.acog.org/womens-health/faqs/combined-hormonal-birth-control-pill-patch-ring. Updated March 2018. Accessed August 16, 2022.
American College of Obstetricians and Gynecologists website. Long-acting reversible contraception (LARC): Intrauterine device (IUD) and implant, FAQ184. www.acog.org/womens-health/faqs/long-acting-reversible-contraception-iud-and-implant. Updated November 2021. Accessed August 16, 2022.
Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(4):1-66. PMID: 27467319 pubmed.ncbi.nlm.nih.gov/27467319/.
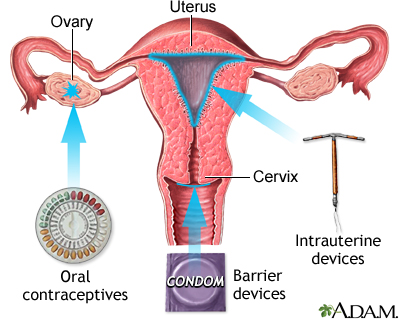
Birth control methods - illustration
Artificial contraception methods work in different ways to decrease the likelihood that sexual intercourse will result in pregnancy. Barrier methods such as condoms (male or female), diaphragms (with or without spermicide) and sponges (with spermicide) have as their first line of defense the physical blocking of the sperm's entry into the uterus. If sperm cannot get into the uterus it cannot fertilize an egg, and pregnancy cannot occur. IUDs disrupt the normal uterine environment. The hormones in oral contraceptives and hormone implants fool the ovaries into refraining from ovulation, and without a fertile egg, pregnancy will not occur. IUDs and oral contraceptives and hormones may be used as emergency contraception in the case of unprotected sex, but neither one will protect against sexually-transmitted disease.
Birth control methods
illustration
Birth control methods - illustration
Artificial contraception methods work in different ways to decrease the likelihood that sexual intercourse will result in pregnancy. Barrier methods such as condoms (male or female), diaphragms (with or without spermicide) and sponges (with spermicide) have as their first line of defense the physical blocking of the sperm's entry into the uterus. If sperm cannot get into the uterus it cannot fertilize an egg, and pregnancy cannot occur. IUDs disrupt the normal uterine environment. The hormones in oral contraceptives and hormone implants fool the ovaries into refraining from ovulation, and without a fertile egg, pregnancy will not occur. IUDs and oral contraceptives and hormones may be used as emergency contraception in the case of unprotected sex, but neither one will protect against sexually-transmitted disease.
Birth control methods
illustration
- Diabetes - type 1 - InDepth(In-Depth)
- Diabetes - type 2 - InDepth(In-Depth)
- Carpal tunnel syndrome - InDepth(In-Depth)
- Infertility in women - InDepth(In-Depth)
- Stress - InDepth(In-Depth)
- Scleroderma - InDepth(In-Depth)
- Uterine fibroids and hysterectomy - InDepth(In-Depth)
- Insomnia - InDepth(In-Depth)
- Heart failure - InDepth(In-Depth)
- Narcolepsy - InDepth(In-Depth)
Review Date: 4/19/2022
Reviewed By: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.