Cardiac ablation procedures
Catheter ablation; Radiofrequency catheter ablation; Cryoablation - cardiac ablation; AV nodal reentrant tachycardia - cardiac ablation; AVNRT - cardiac ablation; Wolff-Parkinson-White Syndrome - cardiac ablation; Atrial fibrillation - cardiac ablation; Atrial flutter - cardiac ablation; Ventricular tachycardia - cardiac ablation; VT - cardiac ablation; Arrhythmia - cardiac ablation; Abnormal heart rhythm - cardiac ablationCardiac ablation is a procedure that is used to scar small areas in your heart that may be involved in your heart rhythm problems. This can prevent the abnormal electrical signals or rhythms from moving through your heart.
Heart rhythm problems
An arrhythmia is a disorder of the heart rate (pulse) or heart rhythm. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregul...

During the procedure, small wires called electrodes are placed inside your heart to measure your heart's electrical activity. When the source of the problem is found, the tissue causing the problem is destroyed.
Description
There are two methods for performing cardiac ablation:
- Radiofrequency ablation uses heat energy to eliminate the problem area.
- Cryoablation uses very cold temperatures.
The type of procedure you have will depend on what kind of abnormal heart rhythm you have.
Cardiac ablation procedures are done in a hospital laboratory by a team of trained staff. This includes cardiologists (heart doctors), technicians, and nurses. The setting is safe and controlled so your risk is as low as possible.
You will be given medicine (a sedative) before the procedure to help you relax.
- The skin on your neck, arm, or groin will be cleaned well and made numb with an anesthetic.
- Next, the cardiologist will make a small cut in the skin.
- A small, flexible tube (catheter) will be inserted through this cut into one of the blood vessels in the area. The cardiologist will use live x-ray images to carefully guide the catheter up into your heart.
- Sometimes more than one catheter is needed.
Once the catheter is in place, your cardiologist will place small electrodes in different areas of your heart.
- These electrodes are connected to monitors that allow the cardiologist to tell what area in your heart is causing problems with your heart rhythm. In most cases, there are one or more specific areas.
- Once the source of the problem has been found, one of the catheter lines is used to send electrical (or sometimes cold) energy to the problem area.
- This creates a small scar that causes the heart rhythm problem to stop.
Catheter ablation is a long procedure. It can last 4 or more hours. During the procedure your heart will be monitored closely. A health care team member may ask you if you are having symptoms at different times during the procedure. Symptoms you may feel are:
- A brief burning when medicines are injected
- A faster or stronger heartbeat
Faster or stronger heartbeat
Palpitations are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may:Have an unpl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lightheadedness
- Burning when the electrical energy is used
Why the Procedure is Performed
Cardiac ablation is used to treat certain heart rhythm problems that medicines are not controlling. These problems may be dangerous if they are not treated.
Common symptoms of heart rhythm problems may include:
- Chest pain
- Fainting
- Slow or fast heartbeat (palpitations)
- Lightheadedness, dizziness
- Paleness
- Shortness of breath
- Skipping beats -- changes in the pattern of the pulse
- Sweating
Some heart rhythm problems are:
- AV nodal reentrant tachycardia (AVNRT)
- Associated with an accessory pathway, such as Wolff-Parkinson-White syndrome
Wolff-Parkinson-White syndrome
Wolff-Parkinson-White (WPW) syndrome is a condition in which there is an extra electrical pathway in the heart that leads to periods of rapid heart r...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Atrial fibrillation
Atrial fibrillation
Atrial fibrillation (AFib) and atrial flutter are common types of abnormal heart rhythms (arrhythmias) which affect the upper chambers (atria) of the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Atrial flutter
Atrial flutter
Atrial fibrillation (AFib) and atrial flutter are common types of abnormal heart rhythms (arrhythmias) which affect the upper chambers (atria) of the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ventricular tachycardia
Ventricular tachycardia
Ventricular tachycardia (VT) is a rapid heartbeat that starts in the lower chambers of the heart (ventricles).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks
Catheter ablation is generally safe. Talk with your cardiologist about these rare complications:
- Bleeding or blood pooling where the catheter is inserted
-
Blood clot that goes to arteries in your leg, heart, or brain
Blood clot
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Damage to the artery where the catheter is inserted
- Damage to heart valves
- Damage to the coronary arteries (blood vessels that carry blood to your heart)
- Esophageal atrial fistula (a connection that forms between your esophagus and part of your heart)
Fistula
A fistula is an abnormal connection between two body parts, such as an organ or blood vessel and another structure. Fistulas are usually the result ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fluid around the heart (cardiac tamponade)
Cardiac tamponade
Cardiac tamponade is pressure on the heart that occurs when blood or fluid builds up in the space between the heart muscle and the outer covering sac...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart attack
Heart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Vagal or phrenic nerve damage
Before the Procedure
Always tell your health care providers what medicines you are taking, even medicines or herbs you bought without a prescription.
During the days before the procedure:
- Ask your cardiologist which medicines you should still take on the day of the surgery.
- Tell your cardiologist if you are taking aspirin, clopidogrel (Plavix), prasugrel (Effient), ticagrelor (Brilinta), warfarin (Coumadin), or another blood thinner such as apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa) and edoxaban (Savaysa).
- If you smoke, stop before the procedure. Ask your provider for help if you need it.
- Tell your cardiologist if you have a cold, flu, fever, herpes breakout, or other illness.
Cold
The common cold most often causes a runny nose, nasal congestion, and sneezing. You may also have a sore throat, cough, headache, or other symptoms....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFlu
The flu (influenza) is a viral respiratory illness that causes fever, chills, runny nose, body aches, and cough. It spreads easily from person to pe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHerpes
Genital herpes is a sexually transmitted infection. It is caused by the herpes simplex virus (HSV). This article focuses on HSV type 2 infection....
Read Article Now Book Mark Article
On the day of the procedure:
- You will most often be asked not to drink or eat anything after midnight the night before your procedure.
- Take the medicines your cardiologist has told you to take with a small sip of water.
- You will be told when to arrive at the hospital.
After the Procedure
Pressure to reduce bleeding is put on the area where the catheters were inserted into your body. You will be kept in bed for at least 1 hour. You may need to stay in bed for up to 5 or 6 hours. Your heart rhythm will be checked during this time.
Your cardiologist will decide whether you can go home on the same day, or if you will need to stay in the hospital overnight for continued heart monitoring. You will need someone to drive you home after your procedure.
For 2 or 3 days after your procedure, you may have these symptoms:
- Fatigue
- Achy feeling in your chest
- Skipped heartbeats or times when your heartbeat is very fast or irregular
Your cardiologist may keep you on your medicines, or give you new ones that help control your heart rhythm.
Outlook (Prognosis)
Success rates are different depending on what type of heart rhythm problem is being treated.
References
Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275-e444. PMID: 28506916 pubmed.ncbi.nlm.nih.gov/28506916/.
Mehta NK, Haines DE. Cryoablation and other radiofrequency alternatives. In Jalife J, Stevenson WG, eds. Zipes and Jalife’s Cardiac Electrophysiology: From Cell to Bedside. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 131.
Miller JM, Ellenbogen KA. Therapy for cardiac arrhythmias. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 64.
Qian PC, Sauer WH. Radiofrequency ablation. In: Jalife J, Stevenson WG, eds. Zipes and Jalife’s Cardiac Electrophysiology: From Cell to Bedside. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 130.
-
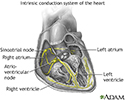
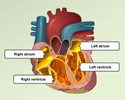
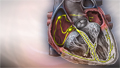
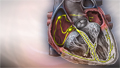
Conduction system of the heart - illustration
The intrinsic conduction system sets the basic rhythm of the beating heart by generating impulses which stimulate the heart to contract.
Conduction system of the heart
illustration
Review Date: 7/14/2024
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.