Upper airway biopsy
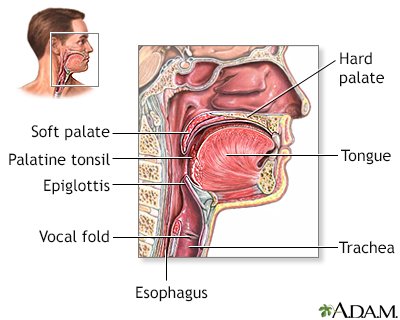
Upper airway biopsy is surgery to remove a small piece of tissue from the nose, mouth, and throat area. The tissue will be examined under the microscope by a pathologist.
How the Test is Performed
The surgeon will spray a numbing medicine in your mouth and throat. A metal tube is inserted to hold your tongue out of the way.
Another numbing medicine flows through the tube down the back of the throat. This may cause you to cough at first. When the area feels thick or swollen, it is numb.
The test may also be performed under general anesthesia, so that you will be asleep and not feel pain.
The surgeon looks at the abnormal area, and removes a small piece of tissue. It is sent to the laboratory for examination.
How to Prepare for the Test
DO NOT eat for 6 to 12 hours before the test.
Tell your surgeon if you take a blood thinner, such as aspirin, clopidogrel, or warfarin, when you schedule the biopsy. You may need to stop taking them for a little while. Never stop taking any medicines without first talking to your surgeon or health care provider.
How the Test will Feel
As the area is being numbed, you may feel like there is fluid running down the back of your throat. You may feel the need to cough or gag. And you may feel pressure or mild tugging.
When the numbness wears off, your throat may feel scratchy for several days. After the test, the cough reflex will return in 1 to 2 hours. Then you may eat and drink normally.
Why the Test is Performed
This test may be done if your provider thinks there is a problem with your upper airway. It may also be done with a bronchoscopy.
Bronchoscopy
Bronchoscopy is a test to view the airways and diagnose lung disease. It may also be used during the treatment of some lung conditions.

Normal Results
The upper airway tissues are normal, with no abnormal growths.
What Abnormal Results Mean
Disorders or conditions that may be discovered include:
- Benign (noncancerous) cysts or masses
- Cancer
Cancer
Cancer is the uncontrolled growth of abnormal cells in the body. Cancerous cells are also called malignant cells.
Read Article Now Book Mark Article - Certain infections
- Granulomas and related inflammation (may be caused by tuberculosis)
Granulomas
Granulomatosis with polyangiitis (GPA) is a rare disorder in which blood vessels become inflamed. This leads to damage in major organs of the body. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleTuberculosis
Pulmonary tuberculosis (TB) is a contagious bacterial infection that involves the lungs. It may spread to other organs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Autoimmune disorders, such as granulomatosis with polyangiitis
Granulomatosis with polyangiitis
Granulomatosis with polyangiitis (GPA) is a rare disorder in which blood vessels become inflamed. This leads to damage in major organs of the body. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Necrotizing vasculitis
Necrotizing vasculitis
Necrotizing vasculitis is a group of disorders that involve inflammation of the blood vessel walls. The size of the affected blood vessels helps to ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks
Risks for this procedure include:
- Bleeding (some bleeding is common, heavy bleeding is not)
- Breathing difficulties
- Sore throat
There is a risk of choking if you swallow water or food before the numbness wears off.
Reviewed By
Ashutosh Kacker, MD, FACS, Professor of Clinical Otolaryngology, Weill Cornell Medical College, and Attending Otolaryngologist, New York-Presbyterian Hospital, New York, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Barbareschi M, Mengoli MC, Cavazza A. Nonneoplastic pathology of the large and small airways. In: Smith ML, Leslie KO, Wick MR, eds. Practical Pulmonary Pathology: a diagnostic approach. 4th ed. Philadelphia, PA: Elsevier; 2024:chap 9.
Kraft M. Approach to the patient with respiratory disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 71.
Küpeli E, Mehta AC. Diagnostic bronchoscopy: Basic techniques. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 26.
Yu DH, Feller-Kopman D. Tracheobronchial endoscopy. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 71.


 All rights reserved.
All rights reserved.