Oropharynx lesion biopsy
Throat lesion biopsy; Biopsy - mouth or throat; Mouth lesion biopsy; Oral cancer - biopsyAn oropharynx lesion biopsy is surgery in which tissue from an abnormal growth or mouth sore is removed and checked for disease.
How the Test is Performed
Painkilling or numbing medicine is first applied to the area. For large sores or sores of the throat, general anesthesia may be needed. This means you will be asleep during the procedure.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
Read Article Now Book Mark ArticleAll or part of the problem area (lesion) is removed. It is sent to the laboratory to check for diseases. If a growth in the mouth or throat needs to be removed, the biopsy will be done first. This is followed by the actual removal of the growth.
How to Prepare for the Test
If a simple painkilling or local numbing medicine is to be used, there is no special preparation. If the test is part of a growth removal or if general anesthesia is used, you will likely be asked not to eat for 6 to 8 hours before the test.
How the Test will Feel
You may feel pressure or tugging while the tissue is being removed. After the numbness wears off, the area may be sore for a few days.
Why the Test is Performed
This test is done to determine the cause of a sore (lesion) in the throat.
Normal Results
This test is only done when there is an abnormal tissue area.
What Abnormal Results Mean
Abnormal results may mean:
- Cancer (such as squamous cell carcinoma)
Cancer
Cancer is the uncontrolled growth of abnormal cells in the body. Cancerous cells are also called malignant cells.
Read Article Now Book Mark ArticleSquamous cell carcinoma
Squamous cell skin cancer is the second most common type of cancer in the United States. Other common types of skin cancer are:Basal cell cancerMelan...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Benign lesions (such as papilloma)
- Fungal infections (such as candida)
- Histoplasmosis
Histoplasmosis
Histoplasmosis is an infection that occurs from breathing in the spores of the fungus Histoplasma capsulatum.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Oral lichen planus
Oral lichen planus
Lichen planus is a condition that forms a very itchy rash on the skin or in the mouth.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Precancerous sore (leukoplakia)
- Viral infections (such as Herpes simplex)
Risks
Risks of the procedure may include:
- Infection of the site
- Bleeding at the site
If there is bleeding, the blood vessels may be sealed (cauterized) with an electric current or laser.
Considerations
Avoid hot or spicy food after the biopsy.
References
Sciubba JJ. Oral mucosal lesions. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 87.
Sinha P, Harréus U. Malignant neoplasms of the oropharynx. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 96.
Throat anatomy - illustration
Structures of the throat include the esophagus, trachea, epiglottis and tonsils.
Throat anatomy
illustration
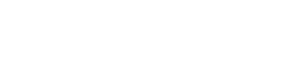
Oropharyngeal biopsy - illustration
Oropharyngeal biopsy is a procedure in which tissue from an abnormal growth or lesion is removed and sent to the lab for testing. Depending upon the size, a small portion or the entire lesion is removed.
Oropharyngeal biopsy
illustration
Throat anatomy - illustration
Structures of the throat include the esophagus, trachea, epiglottis and tonsils.
Throat anatomy
illustration
Oropharyngeal biopsy - illustration
Oropharyngeal biopsy is a procedure in which tissue from an abnormal growth or lesion is removed and sent to the lab for testing. Depending upon the size, a small portion or the entire lesion is removed.
Oropharyngeal biopsy
illustration
Review Date: 10/28/2024
Reviewed By: Ashutosh Kacker, MD, FACS, Professor of Clinical Otolaryngology, Weill Cornell Medical College, and Attending Otolaryngologist, New York-Presbyterian Hospital, New York, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.