Spasticity
Spasticity is stiff or rigid muscles. It may also be called unusual tightness or increased muscle tone. Reflexes (for example, a knee-jerk reflex) are stronger or exaggerated. The condition can interfere with walking, movement, speech, and many other activities of daily living.
Considerations
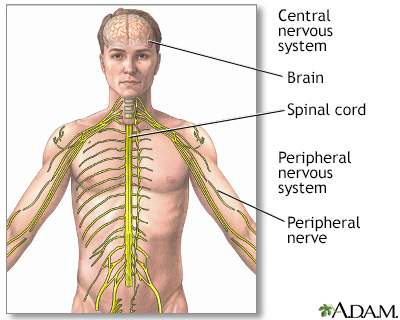
Spasticity is often caused by damage to the part of the brain that is involved in movements under your control. It may also occur from damage to the nerves in the spinal cord.
Symptoms of spasticity include:
- Abnormal posture
- Carrying the shoulder, arm, wrist, and finger at an abnormal angle because of muscle tightness
- Exaggerated deep tendon reflexes (the knee-jerk or other reflexes)
- Repetitive jerky motions (clonus), especially when you are touched or moved
- Scissoring (crossing of the legs as the tips of scissors would close)
- Pain or deformity of the affected area of the body
Spasticity may also affect speech. Severe, long-term spasticity may lead to contracture of muscles. This can reduce range of motion or leave the joints bent.
Contracture
A contracture develops when the normally stretchy (elastic) tissues are replaced by nonstretchy (inelastic) fiber-like tissue. This tissue makes it ...

Causes
Spasticity may be caused by any of the following:
- Brain damage caused by lack of oxygen, as can occur in near drowning or near suffocation
Near drowning
Non-fatal drowning means a person developed trouble breathing from being underwater or having their head underwater, and survived. If a person has be...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cerebral palsy (group of disorders due to brain injury at birth)
Cerebral palsy
Cerebral palsy (CP) is a group of disorders that involve the brain. This affects nervous system functions, such as movement, learning, hearing, seei...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cervical spinal stenosis
- Head injury
- Infections of brain or spinal cord (Lyme disease, syphilis, HIV, tuberculosis)
- Multiple sclerosis
Multiple sclerosis
Multiple sclerosis (MS) is an autoimmune disease that affects the brain and spinal cord (central nervous system).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Neurodegenerative illness (illnesses that damage the brain and nervous system over time)
- Phenylketonuria (disorder in which the body can't break down the amino acid phenylalanine)
Phenylketonuria
Phenylketonuria (PKU) is a rare condition in which a baby is born without the ability to properly break down an amino acid called phenylalanine....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Spinal cord injury
- Stroke
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tumors in brain or spinal cord
- Toxins (nitrous oxide or "laughing gas")
- Vitamin or mineral deficiency (vitamin B12, vitamin E, copper)
This list does not include all conditions that can cause spasticity.
Home Care
Exercise, including muscle stretching, can help make symptoms less severe. Physical therapy is also helpful.
When to Contact a Medical Professional
Contact your health care provider if:
- The spasticity gets worse
- You notice deformity of the affected areas
What to Expect at Your Office Visit
Your doctor will perform a physical exam and ask about your symptoms, including:
- When was it first noticed?
- How long has it lasted?
- Is it always present?
- How severe is it?
- Which muscles are affected?
- What makes it better?
- What makes it worse?
- What other symptoms are present?
After determining the cause of your spasticity, the provider may refer you to a physical therapist. Physical therapy involves different exercises, including muscle stretching and strengthening exercises. Physical therapy exercises can be taught to parents who can then help their child do them at home.
Other treatments may include:
- Medicines to treat spasticity. These need to be taken as instructed.
- Botulinum toxin that can be injected into the spastic muscles.
- In rare cases, a pump used to directly deliver medicine into the spinal fluid and nervous system.
- Sometimes surgery to release the tendon or to cut the nerve-muscle pathway.
Reviewed By
Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School of Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Deluca GC, Griggs RC. Approach to the patient with neurologic disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 368.
McGee S. Examination of the motor system: approach to weakness. In: McGee S, ed. Evidence-Based Physical Diagnosis. 5th ed. Philadelphia, PA: Elsevier; 2022:chap 61.
Oleszek JC, Davidson LT. Spasticity. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 730.
 All rights reserved.
All rights reserved.