Testicle pain
Pain - testicle; Orchalgia; Epididymitis; OrchitisTesticle pain is discomfort in one or both testicles. The pain can spread into the lower abdomen.
Testicles
The testes are 2 egg-shaped male reproductive organs located in the scrotum. They produce sperm and the male hormone, testosterone.

Causes
The testicles are very sensitive. Even a minor injury can cause pain. In some conditions, abdominal pain may occur before testicle pain.
Common causes of testicle pain include:
- Injury.
- Infection or swelling of the sperm ducts (epididymitis) or testicles (orchitis).
Epididymitis
Epididymitis is swelling (inflammation) of the tube that connects the testicle with the vas deferens. The tube is called the epididymis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleOrchitis
Orchitis is swelling (inflammation) of one or both of the testicles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Twisting of the testicles that can cut off the blood supply (testicular torsion). It is most common in young men between 10 and 20 years old. It is a medical emergency that needs to be treated as soon as possible. If surgery is performed within 4 hours, most testicles can be saved.
Testicular torsion
Testicular torsion is twisting of the spermatic cord, which supports the testes in the scrotum. When this occurs, blood supply is cut off to the tes...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Mild pain may be caused by fluid collection in the scrotum, such as:
- Enlarged veins in the scrotum (varicocele).
Varicocele
A varicocele is the swelling of the veins inside the scrotum. These veins are found along the cord that holds up a man's testicles (spermatic cord)....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cyst in the epididymis that often contains dead sperm cells (spermatocele).
Spermatocele
Testicle pain is discomfort in one or both testicles. The pain can spread into the lower abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fluid surrounding the testicle (hydrocele).
- Pain in the testicles may also be caused by a hernia or kidney stone.
-
Testicular cancer is almost always painless. But any testicle lump should be checked out by your health care provider, whether or not there is pain.
Testicular cancer
Testicular cancer is cancer that starts in the testicles. The testicles are the male reproductive glands located in the scrotum.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Home Care
Non-urgent causes of testicle pain, such as minor injuries and fluid collection, can often be treated with home care. The following steps may reduce discomfort and swelling:
- Provide support to the scrotum by wearing an athletic supporter.
- Apply ice (wrapped in a cloth) to the scrotum.
- Take warm baths if there are signs of swelling.
- While lying down, place a rolled towel under your scrotum.
- Try over-the-counter pain relievers, such as acetaminophen or ibuprofen. Do NOT give aspirin to children.
Take the antibiotics your provider gives you if the pain is caused by infection. Preventive measures to take:
- Prevent injury by wearing an athletic supporter during contact sports.
- Follow safer sex practices. If you are diagnosed with chlamydia or another STD, all of your sexual partners need to be checked to see if they are infected or should take treatment.
- Make sure that children have received the MMR (mumps, measles, and rubella) vaccine.
When to Contact a Medical Professional
Sudden, severe testicle pain needs immediate medical care.
Contact your provider right away or go to an emergency room if:
- Your pain is severe or sudden.
- You have had an injury or trauma to the scrotum, and you still have pain or swelling after 1 hour.
- Your pain is accompanied by nausea or vomiting.
Also call your provider right away if:
- You feel a lump in the scrotum.
- You have a fever.
- Your scrotum is warm, tender to the touch, or red.
- You have been in contact with someone who has the mumps.
What to Expect at Your Office Visit
Your provider will do an exam of your groin, testicles, and abdomen. Your provider will ask you questions about the pain such as:
- How long have you had testicular pain? Did it start suddenly or slowly?
- Is the testicle on one side higher than usual?
- Where do you feel the pain? Is it on one or both sides?
- How bad is the pain? Is it constant or does it come and go?
- Does the pain reach into your abdomen or back?
- Have you had any injuries?
- Have you ever had an infection spread by sexual contact?
- Do you have a urethral discharge?
- Do you have any other symptoms like swelling, redness, change in the color of your urine, fever, or unexpected weight loss?
The following tests may be performed:
-
Ultrasound of the testicles
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urinalysis and urine cultures
Urinalysis
Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Testing of prostate secretions
- CT scan or other imaging tests
- Urine test for sexually transmitted infections
References
Matsumoto AM, Anawalt BD. Testicular disorders. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 19.
McGowan CC. Prostatitis, epididymitis, and orchitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 110.
Pontari M. Inflammatory and pain conditions of the male genitourinary tract: prostatitis and related pain conditions, orchitis, and epididymitis. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 56.
-
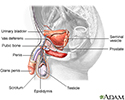
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
Review Date: 7/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.