Liver transplant
Hepatic transplant; Transplant - liver; Orthotopic liver transplant; Liver failure - liver transplant; Cirrhosis - liver transplantLiver transplant is surgery to replace a diseased liver with a healthy liver.
Description
The donated liver may be from:
- A donor who has recently died and has not had liver injury. This type of donor is called a cadaver donor.
- Sometimes, a healthy person will donate part of their liver to a person with a diseased liver. For example, a parent may donate to a child. This kind of donor is called a living donor. The liver can regrow itself in a living donor. Both people most often end up with fully working livers after a successful transplant.
The donor liver is transported in a cooled salt-water (saline) solution that preserves the organ for up to 8 hours. The necessary tests can then be done to match the donor with the recipient.
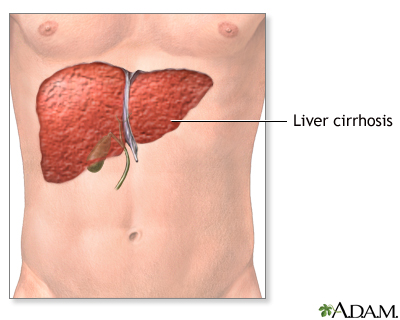
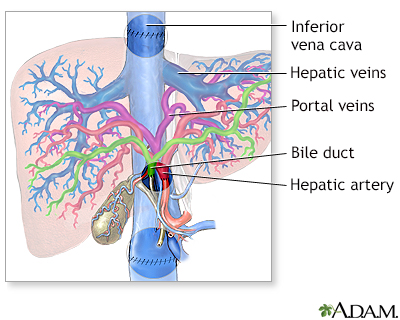
The new liver is removed from the donor through a surgical cut in the upper abdomen. It is placed into the person who needs the liver (called the recipient) and attached to the blood vessels and bile ducts. The operation may take up to 12 hours. The recipient will often need a large amount of blood through a transfusion.
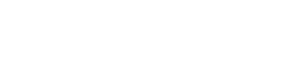
Bile
Bile is a fluid that is made and released by the liver and stored in the gallbladder. Bile helps with digestion. It breaks down fats into fatty acid...

Why the Procedure Is Performed
A healthy liver performs more than 400 jobs each day, including:
- Making bile, which is important in digestion
- Making proteins that help with blood clotting
- Removing or changing bacteria, medicines, and toxins in the blood
- Storing sugars, fats, iron, copper, and vitamins
The most common reason for a liver transplant in children is biliary atresia. In most of these cases, the transplant is from a living donor.
Biliary atresia
Biliary atresia is a blockage in the tubes (ducts) that carry a liquid called bile from the liver to the gallbladder.

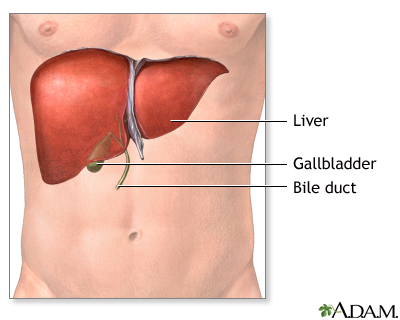
The most common reason for a liver transplant in adults is cirrhosis. Cirrhosis is scarring of the liver that prevents the liver from working well. It can worsen to liver failure. The most common causes of cirrhosis are:
Cirrhosis
Cirrhosis is scarring of the liver and poor liver function. It is the last stage of chronic liver disease.

- Long-term infection with hepatitis B or hepatitis C
Hepatitis B
Hepatitis B is irritation and swelling (inflammation) of the liver due to infection with the hepatitis B virus (HBV). Other types of viral hepatitis ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHepatitis C
Hepatitis C is a viral disease that leads to swelling (inflammation) of the liver. Other types of viral hepatitis include:Hepatitis AHepatitis BHepat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Long-term alcohol overuse
Alcohol overuse
Alcoholic liver disease is damage to the liver and its function due to alcohol abuse.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Metabolic associated steatotic hepatitis (MASH; previously called non-alcoholic steatohepatitis or NASH)
- Acute toxicity from an overdose of acetaminophen or due to consuming poisonous mushrooms
Other illnesses that may cause cirrhosis and liver failure include:
- Autoimmune hepatitis
Autoimmune hepatitis
Autoimmune hepatitis causes inflammation of the liver. It occurs when immune cells mistake the liver's normal cells for harmful invaders and attack ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hepatic vein blood clot (thrombosis)
Hepatic
The term "hepatic" refers to the liver. For example, the hepatic duct drains bile from the liver.
Read Article Now Book Mark ArticleClot
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Liver damage from poisoning or medicines
- Problems with the drainage system of the liver (the biliary tract), such as primary biliary cholangitis (previously called primary biliary cirrhosis) or primary sclerosing cholangitis
Primary biliary cholangitis
The bile ducts are tubes that move bile from the liver to the small intestine. Bile is a substance that helps with digestion. All of the bile ducts...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticlePrimary sclerosing cholangitis
Sclerosing cholangitis refers to swelling (inflammation), scarring, and destruction of the bile ducts inside and outside of the liver.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Metabolic disorders of copper or iron (Wilson disease and hemochromatosis, respectively)
Wilson disease
Wilson disease is an inherited disorder in which there is too much copper in the body's tissues. The excess copper damages the liver and nervous sys...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHemochromatosis
Hemochromatosis is a condition in which there is too much iron in the body. It is also called iron overload.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Liver transplant surgery is often not recommended for people who have:
- Certain infections, such as tuberculosis or osteomyelitis.
Osteomyelitis
Osteomyelitis is a bone infection. It is caused by bacteria or other germs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Difficulty taking medicines several times each day for the rest of their lives.
- Heart or lung disease (or other life-threatening diseases).
- A history of cancer.
- Infections, such as hepatitis, that are considered to be active. But now Hepatitis C can be cured and medicine for Hepatitis B started before transplant.
- Cigarette use or an alcohol or drug use disorder, or other risky lifestyle habits.
- A lack of a good support system.
Risks
Risks of any anesthesia include:
- Problems breathing or with blood pressure
- Reactions to medicines
Risks of any surgery include:
- Bleeding
- Heart attack or stroke
- Infection
Liver transplant surgery and management after surgery carry major risks. There is an increased risk for infection because you must take medicines that suppress the immune system to prevent transplant rejection. Signs of infection include:
- Diarrhea
- Drainage from your surgical wound
- Fever
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Jaundice
- Redness
- Swelling
- Tenderness
Before the Procedure
Your health care provider will refer you to a transplant center. The transplant team will want to make sure that you are a good candidate for a liver transplant. You will make a few visits over several weeks or months. You will need to have blood drawn and imaging tests done.
If you are the person getting the new liver, the following tests will be done before the procedure:
- Tissue and blood typing to make sure your body will not reject the donated liver
Tissue
A histocompatibility antigen blood test looks at proteins called human leukocyte antigens (HLAs). These are found on the surface of almost all cells...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood tests or skin tests to check for infection
- Heart tests such as an electrocardiogram (ECG), echocardiogram, or cardiac catheterization
Electrocardiogram
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEchocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCardiac catheterization
Cardiac catheterization involves passing a thin flexible tube (catheter) into the right or left side of the heart. The catheter is most often insert...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tests to look for early cancer
- Tests to look at your liver, gallbladder, pancreas, small intestine, and the blood vessels around the liver
- Colonoscopy, depending on your age
You may choose to look at one or more transplant centers to determine which is best for you.
- Ask the center how many transplants they perform every year, and their survival rates. Compare these numbers to those of other transplant centers.
- Ask what support groups they have available, and what travel and housing arrangements they offer.
- Ask what is the average waiting time for a liver transplant.
If the transplant team thinks you are a good candidate for a liver transplant, you will be put on a national waiting list.
- Your place on the waiting list is based on a number of factors. Key factors include the type of liver problems you have, how severe your disease is, and the likelihood that a transplant will be successful.
- The amount of time you spend on a waiting list is most often not a factor in how soon you get a liver, with the possible exception of children.
While you are waiting for a liver, follow these steps:
- Follow any diet your transplant team recommends.
- Do not drink alcohol or use drugs.
- Do not smoke.
- Keep your weight in the appropriate range. Follow the exercise program your provider recommends.
- Take all medicines prescribed for you. Report changes in your medicines and any new or worsening medical problems to the transplant team.
- Follow-up with your regular provider and transplant team at any appointments that have been made.
- Make sure the transplant team has your correct phone numbers, so they can contact you immediately if a liver becomes available. Make sure that, no matter where you are going, you can be contacted quickly and easily.
- Have everything ready ahead of time to go to the hospital.
After the Procedure
If you received a donated liver, you will likely need to stay in the hospital for a week or longer. After that, you will need to be closely followed up by a doctor for the rest of your life. You will have regular blood tests after the transplant.
The recovery period is about 6 to 12 months. Your transplant team may ask you to stay close to the hospital for the first 3 months. You will need to have regular check-ups, with blood tests and x-rays for many years.
Outlook (Prognosis)
People who receive a liver transplant may reject the new organ. This means that their immune system sees the new liver as a foreign substance and tries to destroy it.
To avoid rejection, almost all transplant recipients must take medicines that suppress their immune response for the rest of their lives. This is called immunosuppressive therapy. Although the treatment helps prevent organ rejection, it also puts people at a higher risk for infection and cancer.
If you take immunosuppressive medicine, you need to be regularly screened for cancer. The medicines may also cause high blood pressure and high cholesterol, and increase the risks for diabetes.
A successful transplant requires close follow-up with your provider and your transplant team. You must always take your medicine as directed.
References
Carrion AF, Martin P. Liver transplantation. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 97.
Fontana RJ. Liver failure and liver transplantation In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 140.
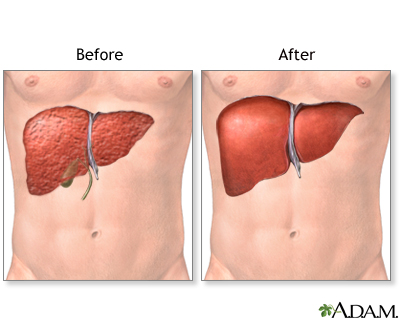
Donor liver attachment - illustration
In liver transplant surgery the diseased liver is removed through an incision made in the upper abdomen. The new liver is put in place and attached to the patient's blood vessels and bile ducts. The healthy liver is obtained from a donor who has recently died but has not suffered liver injury. Liver transplants can save the lives of people who might otherwise die.
Donor liver attachment
illustration
Liver transplant - series
Presentation
Donor liver attachment - illustration
In liver transplant surgery the diseased liver is removed through an incision made in the upper abdomen. The new liver is put in place and attached to the patient's blood vessels and bile ducts. The healthy liver is obtained from a donor who has recently died but has not suffered liver injury. Liver transplants can save the lives of people who might otherwise die.
Donor liver attachment
illustration
Liver transplant - series
Presentation
Review Date: 6/11/2024
Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.