Undescended testicle repair
Orchidopexy; Inguinal orchidopexy; Orchiopexy; Repair of undescended testicle; Cryptorchidism repairUndescended testicle repair is surgery to correct testicles that have not dropped down into the correct position in the scrotum.
Undescended testicle
Undescended testicle occurs when one or both testicles fail to move into the scrotum before birth.

Description
The testicles develop in the infant's abdomen as the baby grows in the womb. They drop down into the scrotum in the last months before birth.
Scrotum
The scrotum is a part of a male's body that is located below the penis. The scrotum is the sac (pouch) that contains the testes, epididymis, and the...

In some cases, one or both testicles do not drop into the correct position. About one half of these cases will descend within the first year of life without treatment.
Undescended testicle repair surgery is recommended for males whose testicles do not descend on their own.
The surgery is done while the child is asleep (unconscious) and pain-free under general anesthesia. The surgeon makes a cut in the groin. This is where most undescended testes are located.
After finding the cord that holds the testis in the scrotum, the surgeon unties it from the tissue around it. This allows the cord to extend to its full length. A small cut is made in the scrotum, and a pouch is created. The testicle is pulled down into the scrotum and stitched into place. Stitches are used to close the surgical cuts.
In some cases, the procedure can be done laparoscopically. This involves smaller surgical cuts.
When the testicle is located very high, correction may require two stages. The separate surgeries are done several months apart.
Why the Procedure Is Performed
This surgery is recommended for infants older than 1 year whose testicles have not descended into the scrotum (cryptorchidism).
Testicles
The testes are 2 egg-shaped male reproductive organs located in the scrotum. They produce sperm and the male hormone, testosterone.

Cryptorchidism
Undescended testicle occurs when one or both testicles fail to move into the scrotum before birth.

An undescended testicle is different from a "retractile" testicle. In this condition, the testicle drops into the scrotum and then pulls back. Retractile testicles do not need surgery.
Risks
Risks of any anesthesia are:
- Reactions to medicines
- Problems breathing
Problems breathing
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks of any surgery are:
- Bleeding
- Infection
Risks of this surgery include:
- Shrinkage of the testicle or failure of the testicle to grow to normal size.
- Inability to bring the testicle into the scrotum, resulting in the removal of the testicle.
After the Procedure
Undescended testicle repair is successful in most cases. A small percentage of men will have fertility problems.
Men who have had undescended testicles should do monthly self-exams for the rest of their lives to look for possible tumors. Men with undescended testes have higher rates of testicular cancer than those with normal testicle development, even if they have a fully descended testicle on the other side. There is also a higher risk for testicular cancer in the other testicle that descended normally. Bringing the testicles down will make it easier to monitor for tumor growth in the future.
Testicular cancer
Testicular cancer is cancer that starts in the testicles. The testicles are the male reproductive glands located in the scrotum.

Outlook (Prognosis)
The surgery may be done on an outpatient basis. Bed rest is recommended for the first 2 to 3 days. Avoid strenuous activity, including bicycling, for at least 1 month.
References
Barthold JS, Hagerty JA. Etiology, diagnosis, and management of the undescended testis. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 46.
Eftekharzadeh S, Weaver J, Srinivasan AK. Laparoscopic orchiopexy. In: Bishoff JT, Kavoussi LR, Kavoussi N, Bishoff T, eds. Atlas of Laparoscopic and Robotic Urologic Surgery. 4th ed. Philadelphia, PA: Elsevier; 2023:chap 39.
Elder JS. Disorders and anomalies of the scrotal contents. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 560.
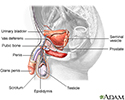
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
Before and after testicular repair - illustration
In normal fetal development, during the last months of birth, the testicles develop in the abdomen and descend into the scrotum in the male fetus. Sometimes at birth, one or both testicles may fail to descend into the scrotum. If the testicle has not descended within the first year of the baby's life, surgery may be recommended to return the testicle to its proper position in the scrotum.
Before and after testicular repair
illustration
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
Before and after testicular repair - illustration
In normal fetal development, during the last months of birth, the testicles develop in the abdomen and descend into the scrotum in the male fetus. Sometimes at birth, one or both testicles may fail to descend into the scrotum. If the testicle has not descended within the first year of the baby's life, surgery may be recommended to return the testicle to its proper position in the scrotum.
Before and after testicular repair
illustration
Review Date: 1/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.