Testicular torsion repair
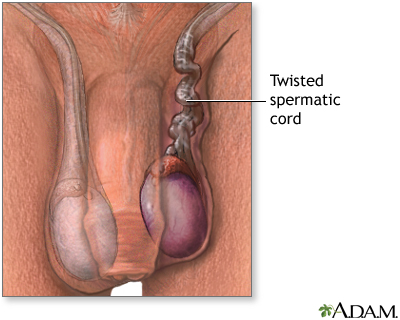
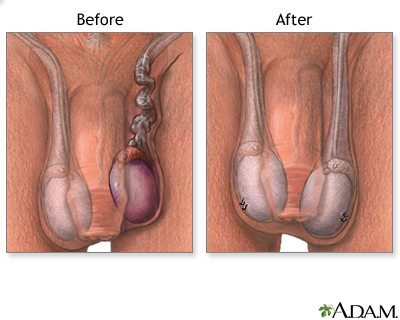
Testicular torsion repair is surgery to untangle or untwist a spermatic cord. The spermatic cord has a collection of blood vessels in the scrotum that lead to the testicles. Testicular torsion develops when the cord twists. This pulling and twisting blocks blood flow to the testicle.
Testicular torsion
Testicular torsion is twisting of the spermatic cord, which supports the testes in the scrotum. When this occurs, blood supply is cut off to the tes...

Description
Most of the time, you will get general anesthesia for testicular torsion repair surgery. You will be asleep and pain-free.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
Read Article Now Book Mark ArticleTo perform the procedure:
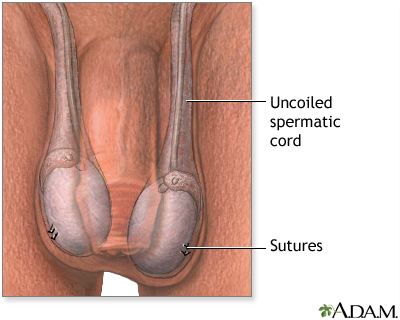
- The surgeon will make a cut in your scrotum to get to the twisted cord.
Scrotum
The scrotum is a part of a male's body that is located below the penis. The scrotum is the sac (pouch) that contains the testes, epididymis, and the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - The cord will be untwisted. The surgeon will then attach the testicle to the inside of your scrotum using stitches.
- The other testicle will be attached in the same way to prevent future problems.
Why the Procedure Is Performed
Testicular torsion is an emergency. In most cases, surgery is needed right away to relieve pain and swelling and to prevent the loss of the testicle. For the best results, surgery should be done within 4 hours after symptoms begin. By 12 hours, a testicle may become damaged so badly that it has to be removed.
Risks
Risks of this surgery are:
- Bleeding
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internal)Outside the body (external)Bleeding may occur:Inside the body when blood le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infection
- Pain
- Wasting away of the testicle despite the return of blood flow
- Infertility
Before the Procedure
Most of the time, this surgery is done as an emergency, so there is often too little time to have medical tests beforehand. You may have an imaging test (most often ultrasound) to check for blood flow and tissue death.
Most of the time, you will be given pain medicine and sent to a urologist for surgery as soon as possible.
After the Procedure
Following your surgery:
- Pain medicine, rest, and ice packs will relieve pain and swelling after surgery.
- Do not put the ice directly on your skin. Wrap it in a towel or cloth.
- Rest at home for several days. You may wear a scrotal support for a week after surgery.
- Avoid strenuous activity for 1 to 2 weeks. Slowly start doing your normal activities.
- You may resume sexual activity after about 4 to 6 weeks.
Outlook (Prognosis)
If surgery is done in time, you should have a complete recovery. When it is done within 4 hours after symptoms begin, the testicle can be saved most of the time.
If one testicle has to be removed, the remaining healthy testicle should provide enough hormones for normal male growth, sex life, and fertility.
References
Boswell B, Thomas AA. Pediatric genitourinary and renal tract disorders. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 168.
Elder JS. Disorders and anomalies of the scrotal contents. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2020:chap 560.
Goldstein M. Surgical management of male infertility. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 67.
Taylor JM, Smith TG, Coburn M. Urologic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 74.
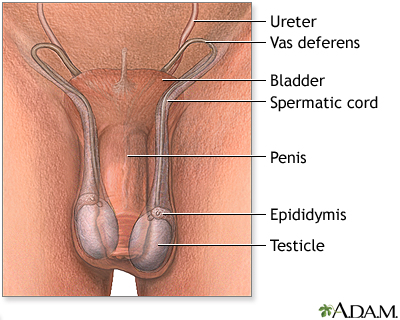
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
Testicular torsion repair - series
Presentation
Review Date: 7/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.