Skin graft
Skin transplant; Skin autografting; FTSG; STSG; Split thickness skin graft; Full thickness skin graftA skin graft is a patch of skin that is removed by surgery from one area of the body and transplanted, or attached, to another area.
Description
This surgery is usually done while you are under general anesthesia. That means you will be asleep and pain-free.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
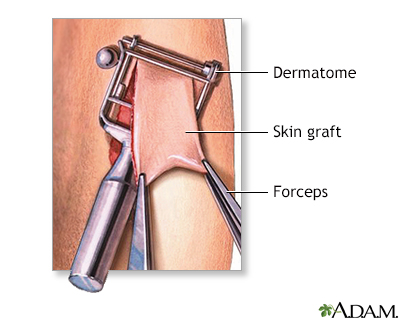
Read Article Now Book Mark ArticleHealthy skin is taken from a place on your body called the donor site. Most people who are having a skin graft have a split-thickness skin graft. This takes the two top layers of skin from the donor site (the epidermis) and the layer under the epidermis (the dermis).
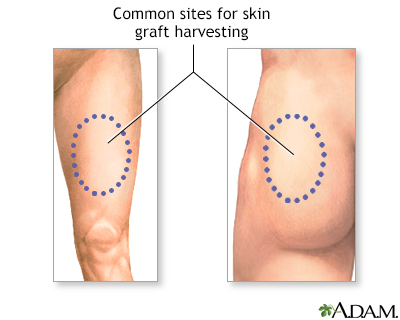
The donor site can be any area of the body. Most times, it is an area that is hidden by clothes, such as the buttock, back, or inner thigh.
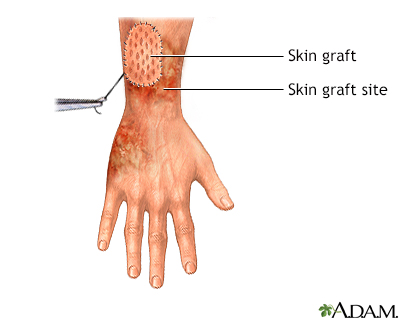
The graft is carefully spread on the bare area where it is being transplanted. It is held in place either by gentle pressure from a well-padded dressing that covers it, or by staples or a few small stitches. The donor-site area is covered with a sterile dressing for 3 to 5 days.
People with deeper tissue loss, or in a cosmetic area such as the face, may need a full-thickness skin graft. This requires the entire thickness of skin from the donor site, not just the top two layers.
A full-thickness skin graft is a more complicated procedure. Common donor sites for full-thickness skin grafts include the chest wall, neck, back, or abdominal wall.
Why the Procedure Is Performed
Skin grafts may be recommended for:
- Areas where there has been infection that caused a large amount of skin loss
- Burns
Burns
Burns commonly occur by direct or indirect contact with heat, electric current, radiation, or chemical agents. Burns can lead to cell death, which c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cosmetic reasons or reconstructive surgeries where there has been skin damage or skin loss
- Skin cancer surgery
- Surgeries that need skin grafts to heal
- Venous ulcers, pressure ulcers, or diabetic ulcers that do not heal
Pressure ulcers
A pressure sore is an area of the skin that breaks down when something keeps rubbing or pressing against the skin.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Very large wounds
- A wound that the surgeon has not been able to close properly
Full-thickness grafts are sometimes done when a lot of tissue is lost. This can happen with open fractures of the lower leg, or after severe infections.
Risks
Risks for anesthesia and surgery in general are:
- Allergic reactions to medicines
- Nausea and vomiting
- Problems with breathing
Problems with breathing
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bleeding, blood clots, or infection
Blood clots
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks for this surgery are:
- Bleeding
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internal)Outside the body (external)Bleeding may occur:Inside the body when blood le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chronic pain (rarely)
- Infection
- Loss of grafted skin (the graft not healing, or the graft healing slowly)
- Reduced or lost skin sensation, or increased sensitivity
- Scarring
- Skin discoloration
- Uneven skin surface
- Poor wound healing and scarring at the donor site
Before the Procedure
Tell your surgeon or nurse if:
- You are or could be pregnant
- You are taking any medicines, including medicines, drugs, supplements, or herbs you bought without a prescription
Planning for your surgery:
- If you have diabetes, heart disease, or other medical conditions, your surgeon may ask you to see the health care provider who treats you for these conditions.
- If you smoke, it's important to cut back or quit. Smoking can slow healing and increase the risk for blood clots. Ask your provider for help quitting smoking.
Quitting smoking
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - If needed, prepare your home to make it easier to recover after surgery.
Prepare your home
Getting your home ready after you have been in the hospital often requires much preparation. Set up your home to make your life easier and safer when...
Read Article Now Book Mark Article - Ask your surgeon if you need to arrange to have someone drive you home after your surgery
During the week before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
- Let your surgeon know about any illness you may have before your surgery. This includes COVID-19, cold, flu, fever, herpes breakout, or other illness. If you do get sick, your surgery may need to be postponed.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
You should recover quickly after split-thickness skin grafting. Full-thickness grafts need a longer recovery time. If you received this kind of graft, you may need to stay in the hospital for recovery.
After you are discharged from the hospital, follow instructions on how to care for your skin graft, including:
- Wearing a dressing for 1 to 2 weeks. Ask your provider how you should care for the dressing, such as protecting it from getting wet.
- Protecting the graft from trauma for 3 to 4 weeks. This includes avoiding being hit or doing any exercise that might injure or dislodge the graft.
- Getting physical therapy, if your surgeon recommends it.
Outlook (Prognosis)
Most skin grafts are successful, but some do not heal well. You may need additional procedures to get the desired result.
References
Loder S, Levi B, Clark A. Skin grafting. In: Gurtner GC, Pusic AL, eds. Plastic Surgery, Volume 1: Principles. 5th ed. Philadelphia, PA: Elsevier; 2024:chap 17.
Padilla PL, Khoo KH, Ho T, Cole EL, Sirvent RZ, Phillips LG. Plastic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 69.
Ratner D, Nayyar PM. Grafts. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2025:chap 148.
Skin graft - illustration
A skin graft is a surgical procedure in which a piece of skin is transplanted from one area to another. Often skin will be taken from unaffected areas on the injured person and used to cover a defect, often a burn. If the area of the skin defect is especially large, the harvested skin may be meshed to stretch it into a larger patch. If the defect involves a great loss of tissue, a full thickness graft, a flap of skin with underlying muscle and blood vessles, may be required. Taking the graft from the injured person makes rejection of the tissue unlikely.
Skin graft
illustration
Skin layers - illustration
The skin is the largest organ of the body. The skin and its derivatives (hair, nails, sweat and oil glands) make up the integumentary system. One of the main functions of the skin is protection. It protects the body from external factors such as bacteria, chemicals, and temperature. The skin contains secretions that can kill bacteria and the pigment melanin provides a chemical pigment defense against ultraviolet light that can damage skin cells. Another important function of the skin is body temperature regulation. When the skin is exposed to a cold temperature, the blood vessels in the dermis constrict. This allows the blood which is warm, to bypass the skin. The skin then becomes the temperature of the cold it is exposed to. Body heat is conserved since the blood vessels are not diverting heat to the skin anymore. Among its many functions the skin is an incredible organ always protecting the body from external agents.
Skin layers
illustration
Skin graft - series
Presentation
Skin graft - illustration
A skin graft is a surgical procedure in which a piece of skin is transplanted from one area to another. Often skin will be taken from unaffected areas on the injured person and used to cover a defect, often a burn. If the area of the skin defect is especially large, the harvested skin may be meshed to stretch it into a larger patch. If the defect involves a great loss of tissue, a full thickness graft, a flap of skin with underlying muscle and blood vessles, may be required. Taking the graft from the injured person makes rejection of the tissue unlikely.
Skin graft
illustration
Skin layers - illustration
The skin is the largest organ of the body. The skin and its derivatives (hair, nails, sweat and oil glands) make up the integumentary system. One of the main functions of the skin is protection. It protects the body from external factors such as bacteria, chemicals, and temperature. The skin contains secretions that can kill bacteria and the pigment melanin provides a chemical pigment defense against ultraviolet light that can damage skin cells. Another important function of the skin is body temperature regulation. When the skin is exposed to a cold temperature, the blood vessels in the dermis constrict. This allows the blood which is warm, to bypass the skin. The skin then becomes the temperature of the cold it is exposed to. Body heat is conserved since the blood vessels are not diverting heat to the skin anymore. Among its many functions the skin is an incredible organ always protecting the body from external agents.
Skin layers
illustration
Skin graft - series
Presentation
Review Date: 1/21/2025
Reviewed By: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.