Parathyroid gland removal
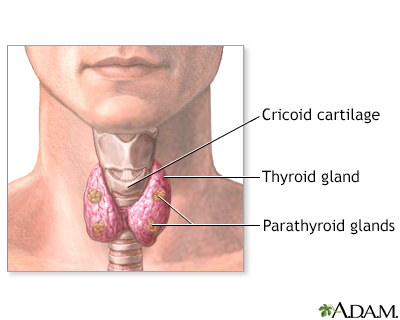
Removal of parathyroid gland; Parathyroidectomy; Hyperparathyroidism - parathyroidectomy; PTH - parathyroidectomyParathyroidectomy is surgery to remove the parathyroid glands or parathyroid tumors. The parathyroid glands are right behind your thyroid gland in your neck. These glands help your body regulate the calcium level in your blood.
Description
You will receive general anesthesia (asleep and pain-free) for this surgery.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
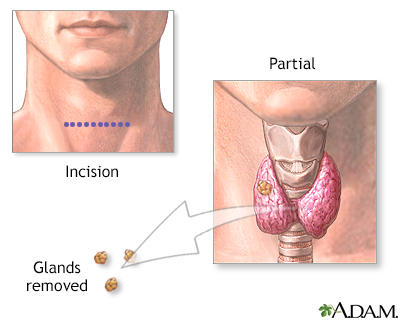
Read Article Now Book Mark ArticleUsually the parathyroid glands are removed using a 2 to 4 inch (in) or 5 to 10 centimeters (cm) surgical cut on your neck. During surgery:
- The cut is usually made in the center of your neck just under your Adam's apple.
- Your surgeon will look for the four parathyroid glands and remove any that are diseased.
- You may have a special blood test during surgery that will tell if all the diseased glands were removed.
- In rare cases, when all four of these glands need to be removed, part of one is transplanted into the forearm. Or, it is transplanted into a muscle in the front of your neck next to the thyroid gland. This helps ensure your body's calcium level stays at a healthy level.
The specific type of surgery depends on where the diseased parathyroid glands are. Types of surgery include:
- Minimally invasive parathyroidectomy. You may receive a shot of a very small amount of radioactive tracer before this surgery. This helps highlight the diseased glands. If you have this shot, your surgeon will use a special probe, like a Geiger counter, to locate the parathyroid gland. Your surgeon will make a small cut (1 to 2 in; or 2.5 to 5 cm) on one side of your neck, and then remove the diseased gland through it. This procedure takes about 1 hour.
- Video-assisted parathyroidectomy. Your surgeon will make two small cuts in your neck. One is for instruments, and the other is for a scope with a camera. Your surgeon will use the camera to view the area and will remove the diseased glands with the instruments.
- Endoscopic parathyroidectomy. Your surgeon will make two or three small cuts in the front of your neck and one cut above the top of your collarbone. This reduces visible scarring, pain, and recovery time. This cut is less than 2 in (5 cm) long. The procedure to remove any diseased parathyroid glands is similar to video-assisted parathyroidectomy.
Why the Procedure Is Performed
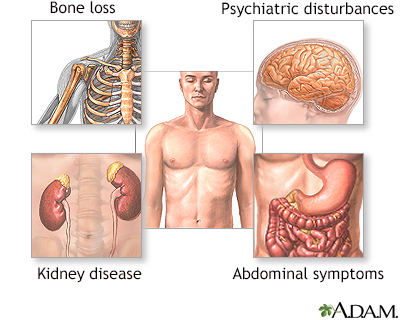
Your health care provider may recommend this surgery if one or more of your parathyroid glands is producing too much parathyroid hormone. This condition is called hyperparathyroidism. It is often caused by a small non-cancerous (benign) tumor called an adenoma.
Hyperparathyroidism
Hyperparathyroidism is a condition in which 1 or more of the parathyroid glands in your neck produce too much parathyroid hormone (PTH).

Your surgeon will consider many factors when deciding whether to do surgery and what type of surgery would be best for you. Some of these factors are:
- Your age
- Calcium levels in your urine and blood
- Whether you have symptoms
Risks
Risks of anesthesia and surgery in general are:
- Reactions to medicines or breathing problems
Breathing problems
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bleeding, blood clots, or infection
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internal)Outside the body (external)Bleeding may occur:Inside the body when blood le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleBlood clots
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks of parathyroidectomy are:
- Injury to the thyroid gland or the need to remove part of the thyroid gland.
- Hypoparathyroidism (parathyroid glands not producing enough parathyroid hormone). This can lead to low calcium levels that are dangerous to your health.
Hypoparathyroidism
Hypoparathyroidism is a disorder in which the parathyroid glands in the neck do not produce enough parathyroid hormone (PTH).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injury to the nerves going to the muscles that move your vocal cords. You may have a hoarse or weaker voice which could be temporary or permanent.
- Difficulty breathing. This is not common and usually goes away several weeks or months after surgery.
Before the Procedure
Parathyroid glands are very small. You may need to have tests that show exactly where your glands are. This will help your surgeon find your parathyroid glands during surgery. Two of the tests you may have are a CT scan and an ultrasound. Sometimes your surgeon will order a nuclear medicine scan, known as a Sestamibi scan prior to your surgery to locate all of the parathyroid glands.
CT scan
A computed tomography (CT) scan is an imaging method that uses x-rays to create pictures of cross-sections of the body. Related tests include:Abdomin...

Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.

Tell your surgeon or nurse if:
- You are or could be pregnant
- You are taking any medicines, including medicines, supplements, or herbs you bought without a prescription
During the week before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
Often, people can go home the same day they have surgery. You can start your everyday activities in a few days. It will take about 1 to 3 weeks for you to fully heal.
The surgery area must be kept clean and dry. You may need to drink liquids and eat soft foods for a day.
Contact your surgeon if you have any numbness or tingling around your mouth in the 24 to 48 hours after surgery. This is caused by low calcium. Follow instructions about how to take your calcium supplements.
After this procedure, you should have periodic blood tests to check your calcium level.
Outlook (Prognosis)
People usually recover soon after this surgery. Recovery may be faster when less invasive techniques are used.
Sometimes, another surgery is needed to remove more of the parathyroid glands.
References
Bobanga I, McHenry CR. The parathyroid glands. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 38.
Karzai S, Prescott JD. Primary hyperparathyroidism. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:860-866.
Parathyroidectomy - illustration
In a parathyroidectomy procedure a small horizontal incision is created just under the Adam's apple to get access to the parathyroid glands. Parathyroidectomy is recommended when the parathyroid glands produce excessive amounts of parathyroid hormone (hyperparathyroidism). After surgery, complete healing without complications usually occurs within 4 weeks. The long term outlook is excellent.
Parathyroidectomy
illustration
Parathyroidectomy - normal anatomy
Presentation
Parathyroidectomy - illustration
In a parathyroidectomy procedure a small horizontal incision is created just under the Adam's apple to get access to the parathyroid glands. Parathyroidectomy is recommended when the parathyroid glands produce excessive amounts of parathyroid hormone (hyperparathyroidism). After surgery, complete healing without complications usually occurs within 4 weeks. The long term outlook is excellent.
Parathyroidectomy
illustration
Parathyroidectomy - normal anatomy
Presentation
Review Date: 9/30/2024
Reviewed By: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.