Imperforate anus repair
Anorectal malformation repair; Perineal anoplasty; Anorectal anomaly; Anorectal plastyImperforate anus repair is surgery to correct a birth defect involving the rectum and anus.
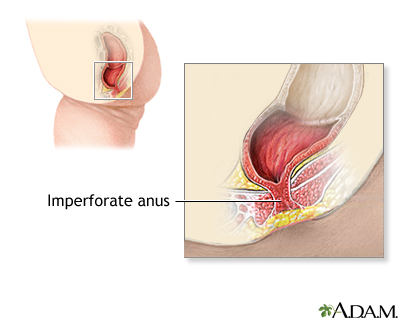
An imperforate anus defect prevents most or all stool from passing out of the rectum.
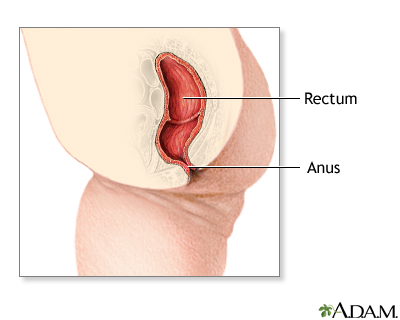
Imperforate anus
Imperforate anus is a defect in which the opening to the anus is missing or blocked. The anus is the opening to the rectum through which stools leav...

Description
How this surgery is performed depends on the type of imperforate anus. The surgery is done under general anesthesia. This means the infant is asleep and feels no pain during the procedure.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
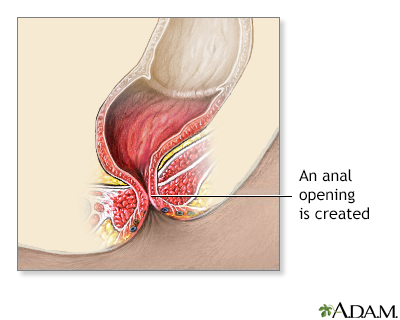
For mild imperforate anus defects:
- The first step involves enlarging the opening where the stool drains, so stool can pass more easily.
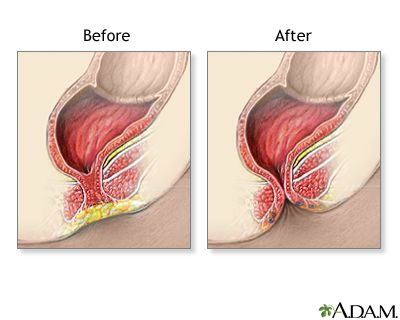
- Surgery involves closing any small tube-like openings (fistulas), creating an anal opening, and putting the rectal pouch into the anal opening. This is called an anoplasty.
Tube-like openings
A fistula is an abnormal connection between two body parts, such as an organ or blood vessel and another structure. Fistulas are usually the result ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - The child must often take stool softeners for weeks to months.
Two surgeries are often needed for more severe imperforate anus defects:
- The first surgery is called a colostomy. The surgeon creates an opening (stoma) in the skin and muscle of the abdominal wall. The end of the large intestine is attached to the opening. Stool will drain into a bag attached to the abdomen.
Colostomy
Colostomy is a surgical procedure that brings one end of the large intestine out through an opening (stoma) made in the abdominal wall. Stools movin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - The baby is often allowed to grow for 3 to 6 months.
- In the second surgery, the surgeon moves the colon to a new position. A cut is made in the anal area to pull the rectal pouch down into place and create an anal opening.
- The colostomy will likely be left in place for 2 to 3 more months.
Your child's surgeon can tell you more about the exact way the surgeries will be done.
Why the Procedure Is Performed
The surgery repairs the defect so that stool can move through the rectum.
Risks
Risks from anesthesia and surgery in general include:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
Risks of this procedure include:
- Damage to the urethra (tube that carries urine out of the bladder)
- Damage to the ureter (tube that carries urine from the kidneys to the bladder)
- Hole that develops through the wall of the intestine (perforation)
- Abnormal connection (fistula) between the anus and vagina or skin
- Narrowed opening of the anus
- Long-term problems with bowel movements because of damage to the nerves and muscles to the colon and rectum (may be constipation or incontinence)
Incontinence
Bowel incontinence is the loss of bowel control, causing you to unexpectedly pass stool. This can range from sometimes leaking a small amount of sto...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Temporary paralysis of the bowel (paralytic ileus)
Paralytic ileus
Intestinal obstruction is a partial or complete blockage of the bowel. The contents of the intestine cannot pass through it.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Before the Procedure
Follow instructions on how to prepare your baby for the surgery.
After the Procedure
Your baby may be able to go home later the same day if a mild defect is repaired. Or, your baby may need to spend several days in the hospital.
Your health care provider will use an instrument to stretch (dilate) the new anus. This is done to improve muscle tone and prevent narrowing. This stretching must be done for several months.
Outlook (Prognosis)
Most defects can be corrected with surgery. Children with mild defects usually do very well. But, constipation may be a problem.
Children who have more complex surgeries still usually have control of their bowel movements. But, they often need to follow a bowel program. This includes eating high-fiber foods, taking stool softeners, and sometimes using enemas.
Some children may need more surgery. Most of these children will need to be followed-up closely for life.
Children with imperforate anus may also have other birth defects, including problems with the heart, kidneys, arms, legs, or spine.
References
Bischoff A, De La Torre L, Peña A. Imperforate anus. In: Wyllie R, Hyams JS, Kay M, eds. Pediatric Gastrointestinal and Liver Disease. 6th ed. Philadelphia, PA: Elsevier; 2021:chap 55.
Shanti CM. Surgical conditions of the anus and rectum. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 371.
Review Date: 9/9/2023
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.