Interstitial keratitis
Keratitis interstitial; Cornea - keratitisInterstitial keratitis is inflammation of the tissue of the cornea, the clear window on the front of the eye. This condition can lead to vision loss.
Causes
Interstitial keratitis is a serious condition in which blood vessels grow into the cornea. Such growth can cause loss of the normal clearness of the cornea. This condition is often caused by infections.
Syphilis is the most common cause of interstitial keratitis, but rare causes include:
- Autoimmune diseases, like rheumatoid arthritis and sarcoidosis
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSarcoidosis
Sarcoidosis is a disease in which inflammation occurs in the lymph nodes, lungs, liver, eyes, skin, and/or other tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Leprosy
Leprosy
Leprosy is a disease caused by the bacterium Mycobacterium leprae. This disease causes skin sores, nerve damage, and muscle weakness that gets worse...
Read Article Now Book Mark Article -
Lyme disease
Lyme disease
Lyme disease is a bacterial infection that is spread through the bite of one of several types of ticks.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Tuberculosis
Tuberculosis
Pulmonary tuberculosis (TB) is a contagious bacterial infection that involves the lungs. It may spread to other organs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
In the United States, most cases of syphilis are recognized and treated before this eye condition develops.
However, interstitial keratitis accounts for 10% of avoidable blindness in the least developed countries worldwide.
Symptoms
Symptoms may include:
-
Eye pain
Eye pain
Pain in the eye may be described as a burning, throbbing, aching, or stabbing sensation in or around the eye. It may also feel like you have a forei...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Excessive tearing
- Sensitivity to light (photophobia)
Exams and Tests
Interstitial keratitis can be easily diagnosed by slit-lamp examination of the eyes. Blood tests and chest x-rays will most often be needed to confirm the infection or disease that is causing the condition.
Slit-lamp examination
The slit-lamp examination looks at structures that are at the front of the eye.

Chest x-rays
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.

Treatment
The underlying disease must be treated. Treating the cornea with corticosteroid drops may minimize scarring and help keep the cornea clear.
Once the active inflammation has passed, the cornea may be left severely scarred and with abnormal blood vessels. The only way to restore vision at this stage is with a cornea transplant.
Outlook (Prognosis)
Diagnosing and treating interstitial keratitis and its cause early can preserve the clear cornea and good vision.
Possible Complications
A corneal transplant is not as successful for interstitial keratitis as it is for most other corneal diseases. The presence of blood vessels in the diseased cornea brings white blood cells to the newly transplanted cornea and increases the risk of rejection.
When to Contact a Medical Professional
People with interstitial keratitis need to be followed closely by an ophthalmologist and a medical specialist with knowledge of the underlying disease.
A person with the condition should be checked immediately if:
- Pain gets worse
- Redness increases
- Vision decreases
This is particularly crucial for people with corneal transplants.
Prevention
Prevention consists of avoiding the infection that causes interstitial keratitis. If you do get infected, get prompt and thorough treatment and follow-up.
References
Gauthier A-S, Noureddine S, Delbosc B. Interstitial keratitis diagnosis and treatment. J Fr Ophtalmol. 2019;42(6):e229-e237. PMID: 31103357 pubmed.ncbi.nlm.nih.gov/31103357/.
Starnes TW, Vasaiwala RA, Bouchard CS. Noninfectious keratitis. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 4.17.
World Health Organization website. Eye care, vision impairment and blindness. www.who.int/health-topics/blindness-and-vision-loss#tab=tab_1. Accessed August 9, 2024.
-
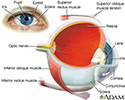
Eye - illustration
The eye is the organ of sight, a nearly spherical hollow globe filled with fluids (humors). The outer layer (sclera, or white of the eye, and cornea) is fibrous and protective. The middle layer (choroid, ciliary body and the iris) is vascular. The innermost layer (retina) is sensory nerve tissue that is light sensitive. The fluids in the eye are divided by the lens into the vitreous humor (behind the lens) and the aqueous humor (in front of the lens). The lens itself is flexible and suspended by ligaments which allow it to change shape to focus light on the retina, which is composed of sensory neurons.
Eye
illustration
-
Eye - illustration
The eye is the organ of sight, a nearly spherical hollow globe filled with fluids (humors). The outer layer (sclera, or white of the eye, and cornea) is fibrous and protective. The middle layer (choroid, ciliary body and the iris) is vascular. The innermost layer (retina) is sensory nerve tissue that is light sensitive. The fluids in the eye are divided by the lens into the vitreous humor (behind the lens) and the aqueous humor (in front of the lens). The lens itself is flexible and suspended by ligaments which allow it to change shape to focus light on the retina, which is composed of sensory neurons.
Eye
illustration
Review Date: 7/9/2024
Reviewed By: Audrey Tai, DO, MS, Athena Eye Care, Mission Viejo, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.