Breast infection
Mastitis; Infection - breast tissue; Breast abscess - post partum mastitis; Breastfeeding - mastitisA breast infection is an infection in the tissue of the breast.
Causes
Breast infections are usually caused by common bacteria (Staphylococcus aureus) found on normal skin. The bacteria enter through a break or crack in the skin, usually on the nipple.
The infection takes place in the fatty tissue of the breast and causes swelling. This swelling pushes on the milk ducts. The result is pain and lumps in the infected breast.
Swelling
Swelling is the enlargement of organs, skin, or other body parts. It is caused by a buildup of fluid in the tissues. The extra fluid can lead to a ...

Breast infections usually occur in women who are breastfeeding. Breast infections inflammation that are not related to breastfeeding might be due to a rare form of breast cancer.
Breast cancer
Breast cancer is cancer that starts in the tissues of the breast. There are two main types of breast cancer:Ductal carcinoma starts in the tubes (du...

Symptoms
Symptoms of a breast infection may include:
-
Breast enlargement or fullness on one side only
Breast enlargement
Premenstrual swelling and tenderness of both breasts often occurs during the second half of the menstrual cycle.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Breast lump
Breast lump
A breast lump is swelling, growth, or mass in the breast. Breast lumps in both men and women raise concern for breast cancer, even though most lumps...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Breast pain
Breast pain
Breast pain is any discomfort or pain in the breast.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fever and flu-like symptoms, including nausea and vomiting
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Itching
Itching
Itching is a tingling or irritation of the skin that makes you want to scratch the area. Itching may occur all over the body or only in one location...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nipple discharge (may contain pus)
Nipple discharge (may contain pus)
Nipple discharge is any fluid that comes out of the nipple area in your breast.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Swelling, tenderness, and warmth in breast tissue
Swelling
Swelling is the enlargement of organs, skin, or other body parts. It is caused by a buildup of fluid in the tissues. The extra fluid can lead to a ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Skin redness, most often in wedge shape
- Tender or enlarged lymph nodes in armpit on the same side
Enlarged lymph nodes
Lymph nodes are present throughout your body. They are an important part of your immune system. Lymph nodes help your body recognize and fight germ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your health care provider will perform physical exam to rule out complications such as a swollen, pus-filled lump (abscess). Sometimes an ultrasound is done to check for an abscess.
For infections that keep returning, milk from the nipple may be cultured. In women who are not breastfeeding, tests done may include:
-
Breast biopsy
Breast biopsy
A breast biopsy is the removal of breast tissue to examine it for signs of breast cancer or other disorders. There are several types of breast biopsi...
Read Article Now Book Mark Article -
Breast MRI
Breast MRI
A breast MRI (magnetic resonance imaging) scan is an imaging test that uses powerful magnets and radio waves to create pictures of the breast and sur...
Read Article Now Book Mark Article -
Breast ultrasound
Breast ultrasound
Breast ultrasound is a test that uses sound waves to examine the breasts.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Mammogram
Mammogram
A mammogram is an x-ray picture of the breasts. It is used to evaluate some breast symptoms and to find breast cancer in women with no symptoms....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Self-care may include applying moist heat to the infected breast tissue for 15 to 20 minutes four times a day. You may also need to take pain relievers.
Antibiotics are very effective in treating a breast infection. If you take antibiotics, you must continue to breastfeed or pump to relieve breast swelling from milk production.
If there is an abscess that does not go away, needle aspiration under ultrasound guidance is done, along with antibiotics. If this method fails to cure the abscess, then incision and drainage is the treatment of choice.
Outlook (Prognosis)
The condition usually clears quickly with antibiotic therapy.
Possible Complications
In severe infections, an abscess may develop. Abscesses need to be drained, either as an office procedure or with surgery. A wound dressing would be needed to help with healing after the procedure. Women with an abscess may be told to temporarily stop breastfeeding.
Abscess
An abscess is a collection of pus in any part of the body. In most cases, the area around an abscess is swollen and inflamed.

When to Contact a Medical Professional
Contact your provider if:
- Any portion of your breast tissue becomes reddened, tender, swollen, or hot
- You are breastfeeding and develop a high fever
- The lymph nodes in your armpit become tender or swollen
Prevention
The following may help reduce the risk of breast infections:
- Careful nipple care to prevent irritation and cracking
- Feeding often and pumping milk to prevent the breast from getting swollen (engorged)
- Proper breastfeeding technique with good latching by the baby
- Weaning slowly, over several weeks, rather than quickly stopping breastfeeding
- Timely treatment of a breast infection before it progresses to a breast abscess
References
Dabbs DJ, Rakha EA. Metaplastic breast carcinoma. In: Dabbs DJ, ed. Breast Pathology. 2nd ed. Philadelphia, PA: Elsevier; 2017:chap 25.
Dabbs DJ, Weidner N. Infections of the breast. In: Dabbs DJ, ed. Breast Pathology. 2nd ed. Philadelphia, PA: Elsevier; 2017:chap 3.
Dinulos JGH. Bacterial infections. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 9.
Klimberg VS, Hunt KK. Diseases of the breast. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 35.
Woods CR. Subcutaneous tissue infections and abscesses. In: Long SS, ed. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 73.
-
Breast engorgement
Animation
-
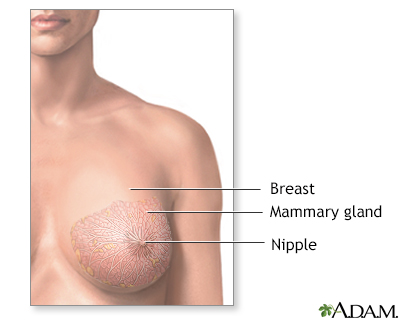
Normal female breast anatomy - illustration
The female breast is composed mainly of fatty tissue interspersed with fibrous or connective tissue. The circular region around the nipple is often a different color or pigmented. This region is called the areola.
Normal female breast anatomy
illustration
-
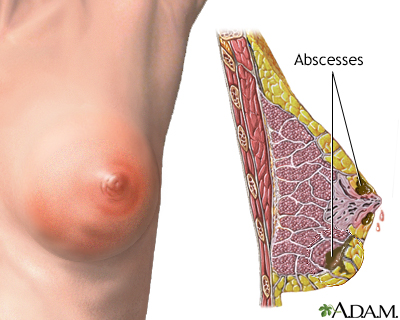
Breast infection - illustration
Most breast infections occur in breastfeeding women when bacteria enters the breast through cracks in the nipple. In severe infections, abscesses may occur. Antibiotics may be indicated for treatment.
Breast infection
illustration
-
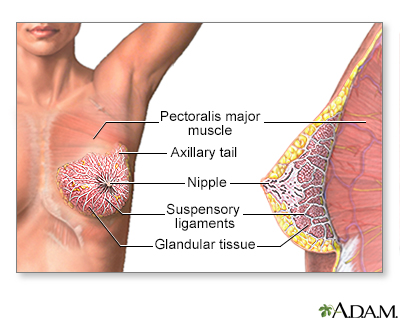
Female Breast - illustration
The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Female Breast
illustration
-
Mastitis - illustration
Mastitis is inflammation of the breast, most commonly due to infection. Mastitis usually occurs in breastfeeding women if milk ducts are blocked, and milk cannot flow out. Bacteria can enter through a duct opening or a crack in the skin of the nipple, and multiply in the milk. Symptoms of mastitis include breast pain, swelling, warmth, and redness.
Mastitis
illustration
-
Normal female breast anatomy - illustration
The female breast is composed mainly of fatty tissue interspersed with fibrous or connective tissue. The circular region around the nipple is often a different color or pigmented. This region is called the areola.
Normal female breast anatomy
illustration
-
Breast infection - illustration
Most breast infections occur in breastfeeding women when bacteria enters the breast through cracks in the nipple. In severe infections, abscesses may occur. Antibiotics may be indicated for treatment.
Breast infection
illustration
-
Female Breast - illustration
The female breast is either of two mammary glands (organs of milk secretion) on the chest.
Female Breast
illustration
-
Mastitis - illustration
Mastitis is inflammation of the breast, most commonly due to infection. Mastitis usually occurs in breastfeeding women if milk ducts are blocked, and milk cannot flow out. Bacteria can enter through a duct opening or a crack in the skin of the nipple, and multiply in the milk. Symptoms of mastitis include breast pain, swelling, warmth, and redness.
Mastitis
illustration
Review Date: 10/10/2022
Reviewed By: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.