Acute arterial occlusion - kidney
Acute renal arterial thrombosis; Renal artery embolism; Acute renal artery occlusion; Embolism - renal arteryAcute arterial occlusion of the kidney is a sudden, severe blockage of the artery that supplies blood to the kidney.
Causes
The kidneys need a good blood supply. The main artery to the kidney is called the renal artery. Reduced blood flow through the renal artery can hurt kidney function. A complete blockage of blood flow to the kidney can often result in permanent kidney failure.
Renal
The term "renal" refers to the kidney. For example, renal failure means kidney failure. Related topics:Kidney diseaseKidney disease - dietKidney fai...

Acute arterial occlusion of the renal artery can occur after injury or trauma to the abdomen, side, or back. Blood clots that travel through the bloodstream (emboli) can lodge in the renal artery. Pieces of plaque from the walls of the arteries can come loose (on their own or during a medical procedure that affects an artery). This debris can block the main kidney artery or one of the smaller vessels.
Emboli
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...

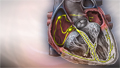
The risk of renal artery blockages increases in people who have certain heart disorders, which make them likely to form blood clots. These include mitral stenosis and atrial fibrillation.
Mitral stenosis
Mitral stenosis is a disorder in which the mitral valve does not fully open. This restricts the flow of blood.

Atrial fibrillation
Atrial fibrillation (AFib) and atrial flutter are common types of abnormal heart rhythms (arrhythmias) which affect the upper chambers (atria) of the...
A narrowing of the renal artery is called renal artery stenosis. This condition increases the risk of a sudden blockage.
Renal artery stenosis
Renovascular hypertension is high blood pressure due to narrowing of the arteries that carry blood to the kidneys. This condition is also called ren...

Symptoms
You may not have symptoms when one kidney does not function because the second kidney can filter the blood. However, high blood pressure (hypertension) may come on suddenly and be difficult to control.
If your other kidney is not working fully, blockage of the renal artery may cause symptoms of acute kidney failure. Other symptoms of acute arterial occlusion of the renal artery include:
Acute kidney failure
Acute kidney failure is the rapid (less than 2 days) loss of your kidneys' ability to remove waste and help balance fluids and electrolytes in your b...

- Abdominal pain
- Abrupt decrease in urine output
- Back pain
-
Blood in the urine
Blood in the urine
Blood in your urine is called hematuria. The amount may be very small and only detected with urine tests or under a microscope. In other cases, the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Flank pain or pain in the side
Flank pain
Flank pain is pain in one side of the body between the upper belly area (abdomen) and the back.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Symptoms of high blood pressure such as headache, change in vision, and swelling
Note: There may be no pain. Pain, if it is present, most often develops suddenly.
Exams and Tests
The health care provider will not be able to identify the problem with just an exam unless you have developed kidney failure.
Tests you may need include:
- Duplex Doppler ultrasound exam of the renal arteries to test blood flow
-
MRI of the kidney arteries, which can show a lack of blood flow to the affected kidney
MRI
A magnetic resonance imaging (MRI) scan is an imaging test that uses powerful magnets and radio waves to create pictures of the body. It does not us...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Renal arteriography shows the exact location of the blockage
Renal arteriography
Renal arteriography is a special x-ray of the arteries of the kidneys.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ultrasound of the kidney to check kidney size
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Some people do not need treatment. Blood clots may get better on their own over time.
You may have treatment to open the artery if the blockage is discovered quickly or it is affecting your only working kidney. Treatment to open the artery may include:
- Clot-dissolving medicines (thrombolytics)
- Medicines that prevent the blood from clotting (anticoagulants), such as warfarin (Coumadin)
- Surgical repair of the renal artery
- Insertion of a tube (catheter) into the renal artery to open the blockage
You may need temporary dialysis to treat acute kidney failure. Medicines to lower cholesterol may be needed if the blockage is due to clots from plaque buildup in the arteries.
Dialysis
Dialysis treats end-stage kidney failure. It removes harmful substances from the blood when the kidneys cannot. This article focuses on peritoneal d...
Read Article Now Book Mark ArticleOutlook (Prognosis)
Damage caused by arterial occlusion may go away. However, in most cases, it is permanent.
If only one kidney is affected, the healthy kidney may take over filtering the blood and producing urine. If you have only one working kidney, arterial occlusion leads to acute kidney failure. This can develop into chronic kidney disease or failure.
Chronic kidney disease or failure
Chronic kidney disease is the slow loss of kidney function over time. The main job of the kidneys is to remove wastes and excess water from the body...

Possible Complications
Complications may include:
- Acute kidney failure
- Chronic kidney disease
- High blood pressure
-
Malignant hypertension
Malignant hypertension
Malignant hypertension is very high blood pressure that comes on suddenly and quickly.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Contact your provider if:
- You stop producing urine
- You feel sudden, severe pain in the back, flank, or abdomen
Get emergency medical help right away if you have symptoms of arterial occlusion and have only one working kidney.
Prevention
In many cases, the disorder is not preventable. The most important way to reduce your risk is to stop smoking.
People at risk for developing blood clots may need to take anti-clotting medicines. Taking steps to control diseases related to atherosclerosis (hardening of the arteries) may reduce your risk.
References
Bellomo R. Acute kidney injury. In: Bersten AD, Handy JM, eds. Oh's Intensive Care Manual. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 47.
Cameron J. Vascular surgery. In: Cameron J, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:993-1214.
DuBose TD, Santos RM. Vascular disorders of the kidney. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 116.
Myers DJ, Myers SI. Systemic complications: renal. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 46.
-
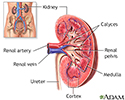
Kidney anatomy - illustration
The kidneys are responsible for removing wastes from the body, regulating electrolyte balance and blood pressure, and the stimulation of red blood cell production.
Kidney anatomy
illustration
-
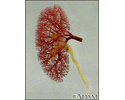
Kidney - blood and urine flow - illustration
This is the typical appearance of the blood vessels (vasculature) and urine flow pattern in the kidney. The blood vessels are shown in red and the urine flow pattern in yellow.
Kidney - blood and urine flow
illustration
-
Kidney blood supply - illustration
The renal arteries supply the kidneys with blood.
Kidney blood supply
illustration
-
Kidney anatomy - illustration
The kidneys are responsible for removing wastes from the body, regulating electrolyte balance and blood pressure, and the stimulation of red blood cell production.
Kidney anatomy
illustration
-
Kidney - blood and urine flow - illustration
This is the typical appearance of the blood vessels (vasculature) and urine flow pattern in the kidney. The blood vessels are shown in red and the urine flow pattern in yellow.
Kidney - blood and urine flow
illustration
-
Kidney blood supply - illustration
The renal arteries supply the kidneys with blood.
Kidney blood supply
illustration
-
Peripheral artery disease and intermittent claudication - InDepth
(In-Depth)
-
Stroke - InDepth
(In-Depth)
Review Date: 4/12/2023
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.