Hydrocarbon pneumonia
Pneumonia - hydrocarbonHydrocarbon pneumonia is caused by drinking or breathing in gasoline, kerosene, furniture polish, paint thinner, or other oily materials or solvents. Many of these hydrocarbons are thin liquids. If you drank one of these hydrocarbons, it is likely some will slip down your windpipe and into your lungs (aspiration) rather than going down your food pipe (esophagus) and into your stomach. This can easily happen if you try to siphon gas out of a gas tank with a hose and your mouth.
Gasoline
This article discusses the harmful effects from swallowing gasoline or breathing in its fumes. This article is for information only. DO NOT use it t...
Read Article Now Book Mark ArticleKerosene
Kerosene is an oil used as a fuel for lamps, as well as heating and cooking. This article discusses the harmful effects from swallowing or breathing...
Read Article Now Book Mark ArticleFurniture polish
Furniture polish poisoning occurs when someone swallows or breathes in (inhales) liquid furniture polish. Some furniture polishes may also be spraye...
Read Article Now Book Mark ArticleHydrocarbons may be inhaled intentionally for intoxication, especially by adolescents. This is referred to as “huffing.”
These products cause fairly rapid changes in the lungs, including inflammation, swelling, and bleeding.
Symptoms
Symptoms may include any of the following:
-
Coma (lack of responsiveness)
Coma
Decreased alertness is a state of reduced awareness and is often a serious condition. A coma is the most severe state of decreased alertness from whi...
Read Article Now Book Mark Article -
Coughing or grunting respiration
Coughing
Coughing is an important way to keep your throat and airways clear. But too much coughing may mean you have a disease or disorder. Some coughs are d...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blue lips and fingernails (cyanosis)
-
Fever
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Shortness of breath
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Smell of a hydrocarbon product on the breath
-
Stupor (decreased level of alertness)
Stupor
Decreased alertness is a state of reduced awareness and is often a serious condition. A coma is the most severe state of decreased alertness from whi...
Read Article Now Book Mark Article -
Vomiting
Vomiting
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up forces the contents of the stomach up t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Wheezing
Exams and Tests
At the emergency room, the health care provider will check vital signs, including temperature, pulse, breathing rate, and blood pressure.
The following tests and interventions (actions taken for improvement) may be done in the emergency department:
- Arterial blood gas (acid-base balance) monitoring
- Breathing support, including oxygen, inhalation treatment, breathing tube and ventilator (breathing machine), in severe cases
- Complete blood count (CBC)
- Chest x-ray
- ECG (electrocardiogram, or heart tracing)
- Fluids by vein (intravenous or IV)
- Blood metabolic panel
Metabolic panel
A comprehensive metabolic panel is a group of blood tests. They provide an overall picture of your body's chemical balance and metabolism. Metaboli...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Toxicology screen
Toxicology screen
A toxicology screen refers to various tests that determine the type and approximate amount of legal and illegal drugs a person has taken by measuring...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Those with mild symptoms should be evaluated by doctors in an emergency room, but may not require a hospital stay. The minimum observation period after inhalation of a hydrocarbon is 6 hours.
People with moderate and severe symptoms are usually admitted to the hospital, occasionally to an intensive care unit (ICU).
Hospital treatment will likely include continuing some or all of the interventions started in the emergency department.
Outlook (Prognosis)
Most children who drink or inhale hydrocarbon products and develop chemical pneumonitis (lung inflammation without infection) recover fully following treatment. Highly toxic hydrocarbons may rapidly cause respiratory failure and death. Repeated ingestions or inhalations may lead to permanent brain damage (including memory, attention and judgment deficits, chronic confusion, dementia and psychiatric problems), liver damage, and other organ damage.
Chemical pneumonitis
Chemical pneumonitis is inflammation of the lungs or breathing difficulty due to inhaling chemical fumes or breathing in and choking on certain chemi...

Respiratory
The words "respiratory" and "respiration" refer to the lungs and breathing.

Possible Complications
Complications may include any of the following:
-
Pleural effusion (fluid surrounding the lungs)
Pleural effusion
A pleural effusion is a buildup of fluid between the layers of tissue that line the lungs and chest cavity.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pneumothorax (collapsed lung from huffing)
Pneumothorax
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung between the lung and chest wall. This buil...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Secondary bacterial infections
When to Contact a Medical Professional
If you know or suspect that your child has swallowed or inhaled a hydrocarbon product, take them to the emergency room immediately. DO NOT use ipecac to make the person throw up.
Prevention
If you have young children, be sure to identify and carefully store materials containing hydrocarbons.
References
Kuschner WG, Blanc PD. Acute responses to toxic exposures. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 103.
Wang GS, Buchanan JA. Hydrocarbons. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 147.
-
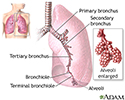
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
Review Date: 1/2/2023
Reviewed By: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.