Retinitis pigmentosa
RP; Vision loss - RP; Night vision loss - RP; Rod Cone dystrophy; Peripheral vision loss - RP; Night blindnessRetinitis pigmentosa is an eye disease in which there is damage to the retina. The retina is the layer of tissue at the back of the inner eye. This layer converts light images to nerve signals and sends them to the brain.
Retina
The retina is the light-sensitive layer of tissue at the back of the eyeball. Images that come through the eye's lens are focused on the retina. Th...

Causes
Retinitis pigmentosa can run in families. The disorder can be caused by several genetic defects.
The cells controlling night vision (rods) are most likely to be affected. However, in some cases, retinal cone cells are damaged the most. The main sign of the disease is the presence of dark deposits in the retina.
The main risk factor is a family history of retinitis pigmentosa. It is a rare condition affecting about 1 in 4,000 people in the United States.
Symptoms
Symptoms often first appear in childhood. However, severe vision problems do not often develop before early adulthood.
- Decreased vision at night or in low light. Early signs may include having a harder time moving around in the dark.
- Loss of side (peripheral) vision, causing "tunnel vision."
- Loss of central vision (in advanced cases). This will affect the ability to read.
Central
The central nervous system is composed of the brain and spinal cord. Your brain and spinal cord serve as the main "processing center" for your entir...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Loss of color vision
- Sensitivity to bright light
Exams and Tests
Tests to evaluate the retina:
- Color vision
- Exam of the retina by ophthalmoscopy after the pupils have been dilated
Ophthalmoscopy
Ophthalmoscopy is an examination of the back part of the eye (fundus), which includes the retina, optic disc, choroid, and blood vessels.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fluorescein angiography
Fluorescein angiography
Fluorescein angiography is an eye test that uses a special dye and camera to look at blood flow in the retina and choroid. These are the two layers ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Intraocular pressure
Intraocular pressure
Tonometry is a test to measure the pressure inside your eyes. The test is used to screen for glaucoma. It is also used to measure how well glaucoma...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Measurement of the electrical activity in the retina (electroretinogram)
Electroretinogram
Electroretinography is a test to measure the electrical response of the eye's light-sensitive cells, called rods and cones. These cells are part of ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pupil reflex response
-
Refraction test
Refraction test
A refraction is an eye exam that measures a person's prescription for eyeglasses or contact lenses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Retinal photography
Retinal photography
Fluorescein angiography is an eye test that uses a special dye and camera to look at blood flow in the retina and choroid. These are the two layers ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Side vision test (visual field test)
-
Slit lamp examination
Slit lamp examination
The slit-lamp examination looks at structures that are at the front of the eye.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Visual acuity
Visual acuity
The visual acuity test is used to determine the smallest letters you can read on a standardized chart (Snellen chart) or a card held 20 feet (6 meter...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
There is no effective treatment for this condition. Wearing sunglasses to protect the retina from ultraviolet light may help preserve vision.
Some studies suggest that treatment with antioxidants (such as high doses of vitamin A palmitate) may slow the disease. However, taking high doses of vitamin A can cause serious liver problems. The benefit of treatment has to be weighed against risks to the liver.
Clinical trials are in progress to assess new treatments for retinitis pigmentosa, including the:
- Use of DHA, which is an omega-3 fatty acid.
- Treatments related to the possible genetic causes of this disorder
Other treatments, such as microchip implants into the retina that act like a microscopic video camera, are in the early stages of development. These treatments may be useful for treating blindness associated with RP and other serious eye conditions.
A vision specialist can help you adapt to vision loss. Make regular visits to an eye care specialist, who can detect cataracts or retinal swelling. Both of these problems can be treated.
Outlook (Prognosis)
The disorder will continue to progress slowly. Complete blindness is uncommon.
Possible Complications
Peripheral and central loss of vision will occur over time.
Loss of vision
Blindness is a lack of vision. It may also refer to a loss of vision that cannot be corrected with glasses or contact lenses. Partial blindness mean...

People with retinitis pigmentosa often develop cataracts at an early age. They may also develop swelling of the retina (macular edema). Cataracts can be removed if they contribute to vision loss.
When to Contact a Medical Professional
Contact your health care provider if you have problems with night vision or you develop other symptoms of this disorder.
Prevention
Genetic counseling and testing may help determine whether your children are at risk for this disease.
References
American Academy of Ophthalmology website. New treatments for retinitis pigmentosa. www.aao.org/eye-health/tips-prevention/gene-therapy-new-retinitis-pigmentosa-lca-luxturna. Updated August 16, 2021. Accessed February 20, 2024.
Cioffi GA, Liebmann JM. Diseases of the visual system. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 391.
Cukras CA, Zein WM, Sieving PA. Progressive and 'stationary' inherited retinal degenerations. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 6.12.
Gregory-Evans K, Yang P, Pennesi ME. Retinitis pigmentosa and allied disorders. In: Sadda SR, Sarraf D, Freund KB, et al , eds. Ryan's Retina. 7th ed. Philadelphia, PA: Elsevier; 2023:chap 43.
Olitisky SE, Marsh JD. Disorders of the retina and vitreous. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 648.
-
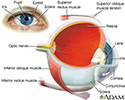
Eye - illustration
The eye is the organ of sight, a nearly spherical hollow globe filled with fluids (humors). The outer layer (sclera, or white of the eye, and cornea) is fibrous and protective. The middle layer (choroid, ciliary body and the iris) is vascular. The innermost layer (retina) is sensory nerve tissue that is light sensitive. The fluids in the eye are divided by the lens into the vitreous humor (behind the lens) and the aqueous humor (in front of the lens). The lens itself is flexible and suspended by ligaments which allow it to change shape to focus light on the retina, which is composed of sensory neurons.
Eye
illustration
-
Slit-lamp exam - illustration
A slit-lamp, which is a specialized magnifying microscope, is used to examine the structures of the eye (including the cornea, iris, vitreous, and retina). The slit-lamp is used to examine, treat (with a laser), and photograph (with a camera) the eye.
Slit-lamp exam
illustration
-
Eye - illustration
The eye is the organ of sight, a nearly spherical hollow globe filled with fluids (humors). The outer layer (sclera, or white of the eye, and cornea) is fibrous and protective. The middle layer (choroid, ciliary body and the iris) is vascular. The innermost layer (retina) is sensory nerve tissue that is light sensitive. The fluids in the eye are divided by the lens into the vitreous humor (behind the lens) and the aqueous humor (in front of the lens). The lens itself is flexible and suspended by ligaments which allow it to change shape to focus light on the retina, which is composed of sensory neurons.
Eye
illustration
-
Slit-lamp exam - illustration
A slit-lamp, which is a specialized magnifying microscope, is used to examine the structures of the eye (including the cornea, iris, vitreous, and retina). The slit-lamp is used to examine, treat (with a laser), and photograph (with a camera) the eye.
Slit-lamp exam
illustration
Review Date: 1/29/2024
Reviewed By: Audrey Tai, DO, MS, Athena Eye Care, Mission Viejo, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.