Idiopathic hypersomnia
Hypersomnia - idiopathic; Drowsiness - idiopathic; Somnolence - idiopathicIdiopathic hypersomnia (IH) is a sleep disorder in which a person is excessively sleepy (hypersomnia) during the day and has great difficulty being awakened from sleep. Idiopathic means there is not a clear cause.
Hypersomnia
Drowsiness refers to feeling more sleepy than normal during the day. People who are drowsy may fall asleep when they do not want to or at times whic...

Causes
IH is similar to narcolepsy in that you are extremely sleepy. It is different from narcolepsy because IH doesn't usually involve suddenly falling asleep (sleep attacks) or losing muscle control due to strong emotions (cataplexy). Also, unlike narcolepsy, naps in IH are usually not refreshing.
Narcolepsy
Narcolepsy is a nervous system problem that causes extreme sleepiness and attacks of daytime sleep.

Symptoms
Symptoms often develop slowly during the teens or young adulthood. They include:
- Daytime naps that do not relieve drowsiness
- Difficulty waking from a long sleep -- may feel confused or disoriented (''sleep drunkenness'')
- Increased need for sleep during the day -- even while at work, or during a meal or conversation
- Increased sleep time -- up to 14 to 18 hours a day
Other symptoms may include:
- Anxiety
- Feeling irritated
- Loss of appetite
- Low energy
- Restlessness
- Slow thinking or speech
- Trouble remembering
Exams and Tests
Your health care provider will ask about your sleep history. The usual approach is to consider other possible causes of excessive daytime sleepiness.
Other sleep disorders that may cause daytime sleepiness include:
- Narcolepsy
-
Obstructive sleep apnea
Obstructive sleep apnea
Obstructive sleep apnea (OSA) is a problem in which your breathing pauses during sleep. This occurs because of narrowed or blocked airways.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Restless leg syndrome
Restless leg syndrome
Restless legs syndrome (RLS) is a nervous system problem that causes you to feel an unstoppable urge to get up and pace or walk. You feel uncomforta...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other causes of excessive sleepiness include:
-
Depression
Depression
Depression may be described as feeling sad, blue, unhappy, miserable, or down in the dumps. Most of us feel this way at one time or another for shor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Certain medicines
- Drug and alcohol use
-
Low thyroid function
Low thyroid function
Hypothyroidism is a condition in which the thyroid gland does not make enough thyroid hormone. This condition is often called underactive thyroid....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Previous head injury
Tests that may be ordered include:
- Multiple-sleep latency test (a test to see how long it takes you to fall asleep during a daytime nap)
- Sleep study (polysomnography, to identify other sleep disorders)
Polysomnography
Polysomnography is a sleep study. This test records certain body functions as you sleep, or try to sleep. Polysomnography is used to diagnose sleep...
Read Article Now Book Mark Article
A mental health evaluation for depression may also be done.
Treatment
Your provider will likely prescribe stimulant medicines such as amphetamine, methylphenidate, or modafinil. These medicines may not work as well for this condition as they do for narcolepsy.
Other medicines for idiopathic hypersomnia, which are also commonly used for narcolepsy, include sodium oxybate (or oxybate salts) and newer wake-promoting agents such as pitolisant and solriamfetol.
Lifestyle changes that can help ease symptoms and prevent injury include:
- Avoid alcohol and medicines that can make the condition worse
- Avoid operating motor vehicles or using dangerous equipment
- Avoid working at night or social activities that delay your bedtime
When to Contact a Medical Professional
Discuss your condition with your provider if you have repeated episodes of daytime sleepiness. They may be due to a medical problem that needs further testing.
References
Avidan AY. Sleep and its disorders. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 101.
Dauvilliers Y, Bassetti CLA. Idiopathic hypersomnia. In: Kryger M, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 113.
Nallu S, Benbadis SR. Disorders of sleep. In: Wing EJ, Schiffman FJ, eds. Cecil Essentials of Medicine. 10th ed. Philadelphia, PA: Elsevier; 2022:chap 108.
-
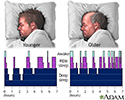
Sleep patterns in the young and aged - illustration
Sleep patterns change with age, anxiety levels and many other factors. Normally, younger people have more concentrated periods of deep sleep compared to older people.
Sleep patterns in the young and aged
illustration
Review Date: 4/20/2023
Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.