Familial hypercholesterolemia
Type II hyperlipoproteinemia; Hypercholesterolemic xanthomatosis; Low density lipoprotein receptor mutationFamilial hypercholesterolemia is a disorder that is passed down through families. It causes LDL (bad) cholesterol level to be very high. The condition begins at birth and can cause heart attacks at an early age.
Related topics include:
-
Familial combined hyperlipidemia
Familial combined hyperlipidemia
Familial combined hyperlipidemia is a disorder that is passed down through families. It causes high blood cholesterol and triglyceride levels....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Familial hypertriglyceridemia
Familial hypertriglyceridemia
Familial hypertriglyceridemia is a common disorder passed down through families. It causes a higher-than-normal level of triglycerides (a type of fa...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Familial dysbetalipoproteinemia
Familial dysbetalipoproteinemia
Familial dysbetalipoproteinemia is a disorder passed down through families. It causes high amounts of cholesterol and triglycerides in the blood....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Causes
Familial hypercholesterolemia is a genetic disorder. It is caused by a gene variant on chromosome 19.
The defect makes the body unable to remove low density lipoprotein (LDL, or bad) cholesterol from the blood. This results in a high level of LDL in the blood. This makes you more likely to have narrowing of the arteries from atherosclerosis at an early age. The condition is typically passed down through families in an autosomal dominant manner. That means you only need to get the abnormal gene from one parent in order to inherit the disease.
Atherosclerosis
Atherosclerosis, sometimes called "hardening of the arteries," occurs when fat, cholesterol, and other substances build up in the walls of arteries. ...

Autosomal dominant
Autosomal dominant is one of many ways that a genetic trait or disorder can be passed down through families. In an autosomal dominant disease, if you...

In rare cases, a child may inherit the gene from both parents. When this occurs, the increase in cholesterol level is much more severe. The risk for heart attacks and heart disease are high, even in childhood.
Symptoms
In the early years there may be no symptoms.
Symptoms that may occur include:
- Fatty skin deposits called xanthomas over parts of the hands, elbows, knees, ankles and around the cornea of the eye
- Cholesterol deposits in the eyelids (xanthelasmas)
- Chest pain (angina) or other signs of coronary artery disease may be present at a young age
Angina
Angina is a type of chest discomfort or pain due to poor blood flow through the blood vessels (coronary arteries) of the heart muscle (myocardium). ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCoronary artery disease
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called co...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cramping of one or both calves when walking
- Sores on the toes that do not heal
- Sudden stroke-like symptoms such as trouble speaking, drooping on one side of the face, weakness of an arm or leg, and loss of balance
Exams and Tests
A physical exam may show fatty skin growths called xanthomas and cholesterol deposits in the eye (corneal arcus).
xanthomas
Xanthoma is a skin condition in which certain fats build up under the surface of the skin.

The health care provider will ask questions about your personal and family medical history. There may be:
- A strong family history of familial hypercholesterolemia or early heart attacks
- High level of LDL cholesterol in either or both parents
People from families with a strong history of early heart attacks should have blood tests done to determine lipid levels.
Blood tests may show:
- High level of total cholesterol
Total cholesterol
Cholesterol is a fat (also called a lipid) that your body needs to work properly. Too much bad cholesterol in your blood can increase your chance of...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High LDL level
- Normal triglyceride levels
Triglyceride
The triglyceride level is a blood test to measure the amount of triglycerides in your blood. Triglycerides are a type of fat. Your body makes some t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other tests that may be done include:
- Studies of cells called fibroblasts to see how the body absorbs LDL cholesterol
- Genetic test for the variant associated with this condition
Treatment
The goal of treatment is to reduce the risk of atherosclerotic heart disease. People who get only one copy of the defective gene from their parents may do well with diet changes and statin drugs.
Atherosclerotic heart disease
Atherosclerosis, sometimes called "hardening of the arteries," occurs when fat, cholesterol, and other substances build up in the walls of arteries. ...

LIFESTYLE CHANGES
The first step is to change what you eat. Most of the time, the provider will recommend that you try this for several months before prescribing medicines. Diet changes include lowering the amount of fat you eat so that it is less than 30% of your total calories. If you are overweight, losing weight is very helpful.
Change what you eat
A healthy diet is an important factor in reducing your risk for heart disease.

Here are some ways to cut saturated fat out of your diet:
- Eat less beef, chicken, pork, and lamb
- Replace full-fat dairy products with low-fat products
- Eliminate trans fats
You can lower the amount of cholesterol you eat by eliminating egg yolks and organ meats such as liver.
It may help to talk to a dietitian who can give you advice about changing your eating habits. Weight loss and regular exercise may also help lower your cholesterol level.
MEDICINES
If lifestyle changes do not change your cholesterol level, your provider may recommend that you take medicines. There are several types of drugs available to help lower blood cholesterol level, and they work in different ways. Some are better at lowering LDL cholesterol, some are good at lowering triglycerides, while others help raise HDL cholesterol. Many people will be on several medicines.
Statin medicines are commonly used and are very effective. These medicines help lower your risk of heart attack and stroke.
They include:
- Lovastatin (Mevacor)
- Pravastatin (Pravachol)
- Simvastatin (Zocor)
- Fluvastatin (Lescol)
- Atorvastatin (Lipitor)
- Pitivastatin (Livalo)
- Rosuvastatin (Crestor)
Other cholesterol-lowering medicines include:
- Bile acid-sequestering resins.
- Ezetimibe.
- Fibrates (such as gemfibrozil or fenofibrate).
-
Nicotinic acid.
Nicotinic acid
Niacin is a type of B vitamin. It is a water-soluble vitamin. It is not stored in the body. Water-soluble vitamins dissolve in water. Leftover am...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - PCSK9 inhibitors, such as alirocumab (Praluent) and evolocumab (Repatha). These represent a newer class of medicines to treat high cholesterol.
People with a severe form of the disorder may need a treatment called apheresis. Blood or plasma is removed from the body. Special filters remove the extra LDL cholesterol, and the blood plasma is then returned to the body.
Outlook (Prognosis)
How well you do depends on how closely you follow your provider's treatment advice and how well you respond to the recommended treatment. Making diet changes, exercising, and taking your medicines correctly can lower cholesterol level. These changes can help delay a heart attack, especially for people with a milder form of the disorder.
Men and women with familial hypercholesterolemia typically are at increased risk of early heart attacks.
The risk of death varies among people with familial hypercholesterolemia. If you inherit two copies of the variant gene, you have a poorer outcome. That type of familial hypercholesterolemia does not respond well to treatment and may cause an early heart attack.
Possible Complications
Complications may include:
- Heart attack at an early age
- Heart disease
- Stroke
- Peripheral vascular disease
When to Contact a Medical Professional
Seek medical care right away if you have chest pain or other warning signs of a heart attack.
Contact your provider if you have a personal or family history of high cholesterol level.
Prevention
A diet low in cholesterol and saturated fat and rich in unsaturated fat may help to control your LDL level.
People with a family history of this condition, particularly if both parents carry the variant gene, may want to seek genetic counseling.
References
Genest J, Mora S, Libby P. Lipoprotein disorders and cardiovascular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 27.
Robinson JG. Disorders of lipid metabolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 190.
-
Xanthoma - close-up - illustration
Xanthomas are lesions on the skin containing cholesterol and fats. They are often associated with inherited disorders of lipid metabolism (inherited problems with the way that fats are broken down and used).
Xanthoma - close-up
illustration
-
Xanthoma on the knee - illustration
Xanthomas are raised, waxy-appearing, frequently yellowish-colored skin lesions, seen here on the knee. These may be associated with an underlying lipid (cholesterol/triglyceride) abnormality.
Xanthoma on the knee
illustration
-
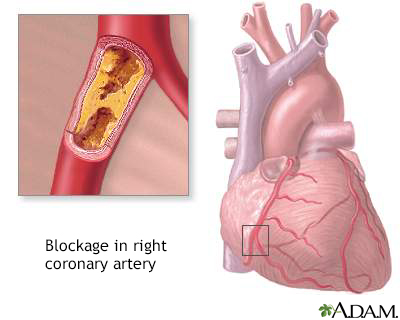
Coronary artery blockage - illustration
Atherosclerosis is a common disorder of the arteries. Fat, cholesterol, and other substances collect in the walls of arteries. Larger accumulations are called atheromas or plaque and can damage artery walls and block blood flow. Severely restricted blood flow in the heart muscle leads to symptoms such as chest pain.
Coronary artery blockage
illustration
-
Xanthoma - close-up - illustration
Xanthomas are lesions on the skin containing cholesterol and fats. They are often associated with inherited disorders of lipid metabolism (inherited problems with the way that fats are broken down and used).
Xanthoma - close-up
illustration
-
Xanthoma on the knee - illustration
Xanthomas are raised, waxy-appearing, frequently yellowish-colored skin lesions, seen here on the knee. These may be associated with an underlying lipid (cholesterol/triglyceride) abnormality.
Xanthoma on the knee
illustration
-
Coronary artery blockage - illustration
Atherosclerosis is a common disorder of the arteries. Fat, cholesterol, and other substances collect in the walls of arteries. Larger accumulations are called atheromas or plaque and can damage artery walls and block blood flow. Severely restricted blood flow in the heart muscle leads to symptoms such as chest pain.
Coronary artery blockage
illustration
Review Date: 5/8/2024
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.