Peripheral artery disease - legs
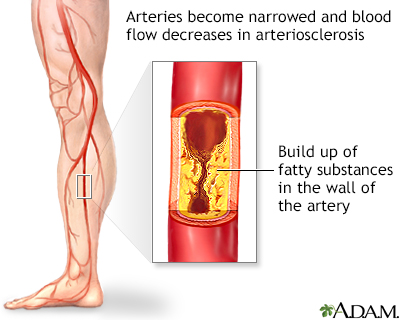
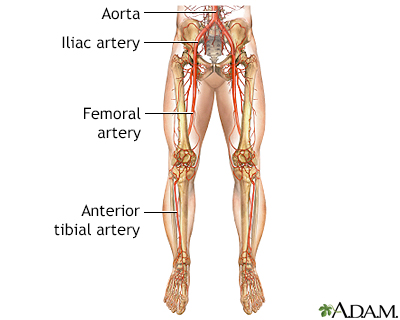
Peripheral vascular disease; PVD; PAD; Arteriosclerosis obliterans; Blockage of leg arteries; Claudication; Intermittent claudication; Vaso-occlusive disease of the legs; Arterial insufficiency of the legs; Recurrent leg pain and cramping; Calf pain with exercisePeripheral artery disease (PAD) is a condition of the blood vessels that supply the legs and feet. It occurs due to narrowing of the arteries in the legs. This causes decreased blood flow, which can injure nerves and other tissues.
Causes
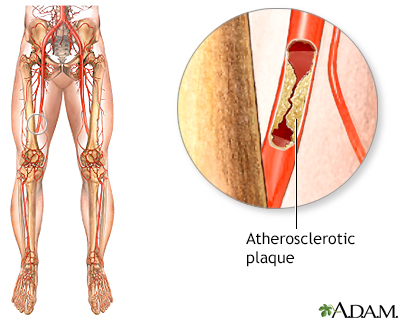
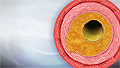
PAD is commonly caused by atherosclerosis. This problem occurs when fatty material (plaque) builds up on the walls of your arteries and makes them narrower. The walls of the arteries also become stiffer and cannot widen (dilate) to allow greater blood flow when needed.
Atherosclerosis
Atherosclerosis, sometimes called "hardening of the arteries," occurs when fat, cholesterol, and other substances build up in the walls of arteries. ...
As a result, the muscles of your legs cannot get enough blood and oxygen when they are working harder (such as during exercise or walking). If PAD becomes severe, there may not be enough blood and oxygen, even when the muscles are resting.
PAD is a common disorder. It most often affects men over age 50, but women can have it as well. People are at higher risk if they have a history of:
- Abnormal blood cholesterol level
-
Diabetes
Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Heart disease (coronary artery disease)
- High blood pressure (hypertension)
Hypertension
Blood pressure is a measurement of the force exerted against the walls of your arteries as your heart pumps blood to your body. Hypertension is the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Kidney disease involving hemodialysis
- Smoking
- Stroke (cerebrovascular disease)
Cerebrovascular disease
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
The main symptoms of PAD are pain, achiness, fatigue, burning, or discomfort in the muscles of your feet, calves, or thighs. These symptoms most often appear during walking or exercise, and go away after several minutes of rest.
- At first, these symptoms may appear only when you walk uphill, walk faster, or walk for longer distances.
- Over time, these symptoms occur more quickly and with less exercise.
- Your legs or feet may feel numb when you are at rest. The legs also may feel cool to the touch, and the skin may look pale.
When PAD becomes severe, you may have:
-
Impotence
Impotence
An erection problem occurs when a man cannot get or keep an erection that is firm enough for intercourse. You may not be able to get an erection at ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pain and cramps at night
- Pain or tingling in the feet or toes, which can be so severe that even the weight of clothes or bed sheets is painful
- Pain that is worse when you elevate your legs, and improves when you dangle your legs over the side of the bed
- Skin that looks dark and blue
- Sores that do not heal
Exams and Tests
During an exam, the health care provider may find:
- A whooshing sound when the stethoscope is held over the artery (arterial bruits)
- Decreased blood pressure in the affected limb
- Weak or absent pulses in the limb
When PAD is more severe, findings may include:
- Calf muscles that shrink (wither or atrophy)
Atrophy
Muscle atrophy is the wasting (thinning) or loss of muscle tissue.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hair loss over the legs, feet, and toes
- Painful, non-bleeding sores on the feet or toes (most often black) that are slow to heal
- Paleness of the skin or blue color in the toes or foot (cyanosis)
Cyanosis
A bluish color to the skin or mucous membrane is usually due to a lack of oxygen in the blood. The medical term is cyanosis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Shiny, tight skin
- Thick toenails
Blood tests may show high cholesterol or diabetes.
High cholesterol
Cholesterol is a fat (also called a lipid) that your body needs to work properly. Too much bad cholesterol in your blood can increase your chance of...
Tests for PAD include:
-
Angiography of the legs
Angiography of the legs
Extremity angiography is a test used to see the arteries in the hands, arms, feet, or legs. It is also called peripheral angiography. Angiography u...
Read Article Now Book Mark Article - Blood pressure measured in the arms and legs for comparison (ankle/brachial index, or ABI)
-
Doppler ultrasound exam of an extremity
Doppler ultrasound exam of an extremity
This test uses ultrasound to look at the blood flow in the large arteries and veins in the arms or legs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Magnetic resonance angiography or CT angiography
Magnetic resonance angiography
Magnetic resonance angiography (MRA) is an MRI exam of the blood vessels. Unlike traditional angiography that involves placing a tube (catheter) int...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Things you can do to control PAD include:
- Balance exercise with rest. Walk or do another activity to the point of pain and alternate it with rest periods. Over time, your circulation may improve as new, small blood vessels form. Always talk to the provider before starting an exercise program.
- Stop smoking. Smoking narrows the arteries, decreases the blood’s ability to carry oxygen, and increases the risk for forming clots (thrombi and emboli).
Thrombi and emboli
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Take care of your feet, especially if you also have diabetes. Wear shoes that fit properly. Pay attention to any cuts, scrapes, or injuries, and see your provider right away. Tissues heal slowly and are more likely to get infected when there is decreased circulation.
- Make sure your blood pressure is well-controlled.
- If you are overweight, reduce your weight.
- If your cholesterol is high, eat a low-cholesterol and low-fat diet.
Low-cholesterol and low-fat diet
A healthy diet is an important factor in reducing your risk for heart disease.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Monitor your blood sugar level if you have diabetes, and keep it under control.
Medicines may be needed to control the disorder, including:
- Aspirin or a medicine called clopidogrel (Plavix), which keeps your blood from forming clots in your arteries. DO NOT stop taking these medicines without first talking with your provider.
- Cilostazol, a drug that works to enlarge (dilate) the affected artery or arteries for moderate-to-severe cases that are not candidates for surgery.
- Medicine to help lower your cholesterol.
- Pain relievers.
If you are taking medicines for high blood pressure or diabetes, take them as your provider has prescribed.
Surgery may be performed if the condition is severe and is affecting your ability to work or do important activities, you are having pain at rest, or you have sores or ulcers on your leg that do not heal. Options are:
-
Procedure to open narrowed or blocked blood vessels that supply blood to your legs
Procedure to open narrowed or blocked b...
Angioplasty is a procedure to open narrowed or blocked blood vessels that supply blood to your legs. Fatty deposits can build up inside the arteries...
Read Article Now Book Mark Article -
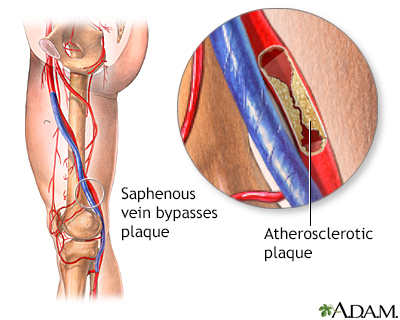
Surgery to reroute the blood supply around a blocked artery
Surgery to reroute the blood supply
Peripheral artery bypass is surgery to reroute the blood supply around a blocked artery in one of your legs. Fatty deposits can build up inside the ...
Read Article Now Book Mark Article
Some people with PAD may need to have the limb removed (amputated).
Outlook (Prognosis)
Most cases of PAD of the legs can be controlled without surgery. Although surgery provides good symptom relief in severe cases, angioplasty and stenting procedures are being used in place of surgery more and more often.
Possible Complications
Complications may include:
- Blood clots or emboli that block small arteries
-
Coronary artery disease
Coronary artery disease
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called co...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Impotence
- Open sores (ischemic ulcers on the lower legs)
Ulcers
An ulcer is a crater-like sore on the skin or mucous membrane. Ulcers form when the top layers of skin or tissue have been removed. They can occur ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tissue death (gangrene)
- The affected leg or foot may need to be amputated
Amputated
Leg or foot amputation is the removal of a leg, foot or toes from the body. These body parts are called extremities. Amputations are done either by...
Read Article Now Book Mark Article
When to Contact a Medical Professional
Contact your provider if you have:
- A leg or foot that becomes cool to the touch, pale, blue, or numb
- Chest pain or shortness of breath with leg pain
- Leg pain that does not go away, even when you are not walking or moving (called rest pain)
- Legs that are red, hot, or swollen
- New sores/ulcers
- Signs of infection (fever, redness, general ill feeling)
General ill feeling
Malaise is a general feeling of discomfort, illness, or lack of well-being.
Read Article Now Book Mark Article - Symptoms of arteriosclerosis of the extremities
Prevention
There is no screening test recommended to identify PAD in patients without symptoms.
Some of the risks for artery disease that you CAN change are:
- Not smoking. If you do smoke, quit.
- Controlling your cholesterol through diet, exercise, and medicines.
- Controlling high blood pressure through diet, exercise, and medicines, if needed.
- Controlling diabetes through diet, exercise, and medicines, if needed.
- Exercising at least 30 minutes a day.
- Keeping to a healthy weight by eating healthy foods, eating less, and joining a weight loss program, if you need to lose weight.
- Learning healthy ways to cope with stress through special classes or programs, or things like meditation or yoga.
- Limiting how much alcohol you drink to 1 drink a day for women and 2 a day for men.
References
Bonaca MP, Creager MA. Peripheral artery disease. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 64.
Ridker PM, Libby P, Buring JE. Risk markers and the primary prevention of cardiovascular disease. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 45.
Simons JP, Schanzer A. Lower extremity arterial disease: decision making and medical treatment. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 108.
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(2):177-183. PMID: 29998344 pubmed.ncbi.nlm.nih.gov/29998344/.
White CJ. Atherosclerotic peripheral arterial disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 71.
-
Peripheral artery disease (PAD): Treatment and management
Animation
-
Arteriosclerosis of the extremities - illustration
Arteriosclerosis of the extremities is a disease of the peripheral blood vessels that is characterized by narrowing and hardening of the arteries that supply the legs and feet. The narrowing of the arteries causes a decrease in blood flow. Symptoms include leg pain, numbness, cold legs or feet and muscle pain in the thighs, calves or feet.
Arteriosclerosis of the extremities
illustration
-
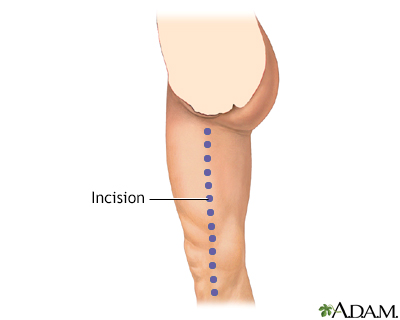
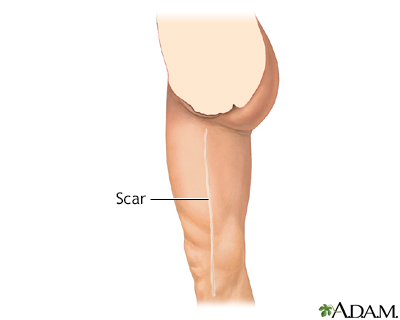
Arterial bypass leg - series - Normal anatomy
Presentation
-
Arteriosclerosis of the extremities - illustration
Arteriosclerosis of the extremities is a disease of the peripheral blood vessels that is characterized by narrowing and hardening of the arteries that supply the legs and feet. The narrowing of the arteries causes a decrease in blood flow. Symptoms include leg pain, numbness, cold legs or feet and muscle pain in the thighs, calves or feet.
Arteriosclerosis of the extremities
illustration
-
Arterial bypass leg - series - Normal anatomy
Presentation
- Atherosclerosis
- Peripheral artery disease and intermittent claudication - InDepth
- Myocardial infarction
- Coronary artery disease - InDepth
- Heart attack and acute coronary syndrome - InDepth
- Stroke - InDepth
- Cholesterol - InDepth
- Diabetes - type 2 - InDepth
- Chronic obstructive pulmonary disease - InDepth
- Diabetes - type 1 - InDepth
Review Date: 5/10/2022
Reviewed By: Deepak Sudheendra, MD, MHCI, RPVI, FSIR, Founder and CEO, 360 Vascular Institute, with an expertise in Vascular Interventional Radiology & Surgical Critical Care, Columbus, OH. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.