Interstitial lung disease
Diffuse parenchymal lung disease; Alveolitis; Idiopathic pulmonary pneumonitis (IPP)Interstitial lung disease (ILD) is a group of lung disorders in which the lung tissues become inflamed and then damaged.
Causes
The lungs contain tiny air sacs (alveoli), which is where oxygen is absorbed. These air sacs expand with each breath.
The tissue around these air sacs is called the interstitium. In people with interstitial lung disease, this tissue becomes inflamed, stiff, or scarred, and the air sacs are not able to expand as much. As a result, not as much oxygen can get to the body.
ILD can occur without a known cause. This is called idiopathic ILD. Idiopathic pulmonary fibrosis (IPF) is the most common disease of this type.
Idiopathic pulmonary fibrosis
Idiopathic pulmonary fibrosis (IPF) is scarring or thickening of the lungs without a known cause.

There are also dozens of known causes of ILD, including:
- Autoimmune diseases (in which the immune system attacks the body) such as lupus, rheumatoid arthritis, sarcoidosis, and scleroderma.
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSarcoidosis
Sarcoidosis is a disease in which inflammation occurs in the lymph nodes, lungs, liver, eyes, skin, and/or other tissues.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleScleroderma
Scleroderma is a disease that involves the buildup of fibrous tissue in the skin and elsewhere in the body. It also damages the cells that line the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lung inflammation due to breathing in a foreign substance such as certain types of dust, fungus, or mold (hypersensitivity pneumonitis).
Hypersensitivity pneumonitis
Hypersensitivity pneumonitis is inflammation of the lungs due to breathing in dust, fungus, molds, or other substances.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Medicines (such as nitrofurantoin, sulfonamides, bleomycin, amiodarone, methotrexate, gold, infliximab, etanercept, and other chemotherapy medicines).
-
Radiation treatment to the chest.
Radiation
Radiation therapy uses high-powered radiation (such as x-rays or gamma rays), particles, or radioactive seeds to kill cancer cells.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Working with or around asbestos, coal dust, cotton dust, and silica dust (called occupational lung disease).
- Infection and partial recovery from diseases like COVID-19.
Cigarette smoking may increase the risk of developing some forms of ILD and may cause the disease to be more severe.
Symptoms
Shortness of breath is a main symptom of ILD. You may breathe faster or need to take deep breaths:
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air

- At first, shortness of breath may not be severe and is only noticed with exercise, climbing stairs, and other activities.
- Over time, it can occur with less strenuous activity such as bathing or dressing, and as the disease worsens, even with eating or talking.
Most people with this condition also have a dry cough. A dry cough means you do not cough up any mucus or sputum.
Over time, weight loss, fatigue, and muscle and joint pain are also present.
People with more advanced ILD may have:
- Abnormal enlargement and curving of the base of the fingernails (clubbing).
Clubbing
Clubbing is changes in the areas under and around the toenails and fingernails that occur with some disorders. The nails may also show changes....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blue color of the lips, skin, or fingernails due to low blood oxygen levels (cyanosis).
Cyanosis
A bluish color to the skin or mucous membrane is usually due to a lack of oxygen in the blood. The medical term is cyanosis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Symptoms of the other diseases such as arthritis or trouble swallowing (scleroderma), associated with ILD.
Exams and Tests
Your health care provider will perform a physical exam. Dry, crackling breath sounds may be heard when listening to your chest with a stethoscope.
The following tests may be done:
- Blood tests to check for autoimmune diseases
-
Bronchoscopy with or without biopsy
Bronchoscopy
Bronchoscopy is a test to view the airways and diagnose lung disease. It may also be used during the treatment of some lung conditions.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleBiopsy
A biopsy is the removal of a small piece of tissue for laboratory examination.
Read Article Now Book Mark Article -
Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - High resolution CT scan of the chest
CT scan
A computed tomography (CT) scan is an imaging method that uses x-rays to create pictures of cross-sections of the body. Related tests include:Abdomin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI chest
MRI chest
A chest MRI (magnetic resonance imaging) scan is an imaging test that uses powerful magnetic fields and radio waves to create pictures of the chest (...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Echocardiogram
- Open lung biopsy
Lung biopsy
A lung needle biopsy is a method to remove a piece of lung tissue for examination. If it is done through the wall of your chest, it is called a tran...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Measurement of the blood oxygen level at rest or when active
-
Blood gases
Blood gases
Blood gases are a measurement of how much oxygen and carbon dioxide are in your blood. They also determine the acidity (pH) of your blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Pulmonary function tests
Pulmonary function tests
Pulmonary function tests are a group of tests that measure breathing and how well the lungs are functioning.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Six minute walk test (checks how far you can walk in 6 minutes and how many times you need to stop to catch your breath)
People who are heavily exposed to known causes of lung disease in the workplace are usually routinely screened for lung disease. These jobs include coal mining, sand blasting, and working on a ship.
Treatment
Treatment depends on the cause and duration of the disease. Medicines that suppress the immune system and reduce swelling in the lungs are prescribed if an autoimmune disease is causing the problem. For some people who have IPF or certain other autoimmune diseases, pirfenidone and nintedanib are two medicines that may be used to slow worsening of the disease. If there is no specific treatment for the condition, the aim is to make you more comfortable and support lung function:
- If you smoke, ask your provider about how to stop smoking.
- People with low blood oxygen levels will receive oxygen therapy in their home. A respiratory therapist will help you set up the oxygen. Families need to learn proper oxygen storage and safety.
Oxygen therapy in their home
Because of your medical problem, you may need to use oxygen to help you breathe. You will need to know how to use and store your oxygen.
Read Article Now Book Mark ArticleProper oxygen storage and safety
Oxygen makes things burn much faster. Think of what happens when you blow into a fire; it makes the flame bigger. If you are using oxygen in your h...
Read Article Now Book Mark Article
Lung rehabilitation can provide support, and help you learn:
- Different breathing methods
- How to set up your home to save energy
- How to eat enough calories and nutrients
- How to stay active and strong
Some people with advanced ILD may need a lung transplant.
Support Groups
You can ease the stress of illness by joining a support group. Sharing with others who have common experiences and problems can help you not feel alone.
Support group
The following organizations are good resources for information on lung disease:American Lung Association -- www. lung. orgNational Heart, Lung, and B...

Outlook (Prognosis)
The chance of recovering or ILD getting worse depends on the cause and how severe the disease was when it was first diagnosed.
Some people with ILD develop heart failure and high blood pressure in the blood vessels of their lungs (pulmonary hypertension).
Pulmonary hypertension
Pulmonary hypertension is high blood pressure in the arteries of the lungs. It makes the right side of the heart work harder than normal.

Idiopathic pulmonary fibrosis has a poor outlook.
When to Contact a Medical Professional
Contact your provider if:
- Your breathing is getting harder, faster, or more shallow than before
- You cannot get a deep breath, or need to lean forward when sitting
- You are having headaches more often
- You feel sleepy or confused
- You have a fever
- You are coughing up dark mucus
- Your fingertips or the skin around your fingernails is blue
References
Corte TJ, Wells AU. Connective tissue diseases. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 92.
Graney BA, Lee JS, King TE. Nonspecific interstitial pneumonitis and other idiopathic interstitial pneumonias. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 90.
Raghu G, Martinez FJ. Interstitial lung disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 80.
-
Clubbing - illustration
Clubbing may result from chronic low blood-oxygen levels. This can be seen with cystic fibrosis, congenital cyanotic heart disease, and several other diseases. The tips of the fingers enlarge and the nails become extremely curved from front to back.
Clubbing
illustration
-
Coal workers pneumoconiosis - stage II - illustration
This chest x-ray shows stage II coal workers pneumoconiosis (CWP). There are diffuse, small light areas on both sides of the lungs. Other diseases that may explain these x-ray findings include simple silicosis, disseminated tuberculosis, metastatic lung cancer, and other diffuse, infiltrative pulmonary diseases.
Coal workers pneumoconiosis - stage II
illustration
-
Coal workers pneumoconiosis - stage II - illustration
This chest x-ray shows coal workers pneumoconiosis - stage II. There are diffuse, small (2 to 4 mm each), light areas throughout both lungs. In the right upper lung (seen on the left side of the picture), there is a light area (measuring approximately 2 cm by 4 cm) with poorly defined borders, representing coalescence (merging together) of previously distinct light areas. Diseases which may explain these x-ray findings include simple coal workers pneumoconiosis (CWP) - stage II, silico-tuberculosis, disseminated tuberculosis, metastatic lung cancer, and other diffuse infiltrative pulmonary diseases.
Coal workers pneumoconiosis - stage II
illustration
-
Coal workers pneumoconiosis, complicated - illustration
This picture shows complicated coal workers pneumoconiosis. There are diffuse, small, light areas (3 to 5 mm) in all areas on both sides of the lungs. There are large light areas which run together with poorly defined borders in the upper areas on both sides of the lungs. Diseases which may explain these X-ray findings include complicated coal workers pneumoconiosis (CWP), silico-tuberculosis, disseminated tuberculosis, metastatic lung cancer, and other diffuse infiltrative pulmonary diseases.
Coal workers pneumoconiosis, complicated
illustration
-
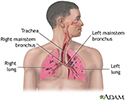
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
-
Clubbing - illustration
Clubbing may result from chronic low blood-oxygen levels. This can be seen with cystic fibrosis, congenital cyanotic heart disease, and several other diseases. The tips of the fingers enlarge and the nails become extremely curved from front to back.
Clubbing
illustration
-
Coal workers pneumoconiosis - stage II - illustration
This chest x-ray shows stage II coal workers pneumoconiosis (CWP). There are diffuse, small light areas on both sides of the lungs. Other diseases that may explain these x-ray findings include simple silicosis, disseminated tuberculosis, metastatic lung cancer, and other diffuse, infiltrative pulmonary diseases.
Coal workers pneumoconiosis - stage II
illustration
-
Coal workers pneumoconiosis - stage II - illustration
This chest x-ray shows coal workers pneumoconiosis - stage II. There are diffuse, small (2 to 4 mm each), light areas throughout both lungs. In the right upper lung (seen on the left side of the picture), there is a light area (measuring approximately 2 cm by 4 cm) with poorly defined borders, representing coalescence (merging together) of previously distinct light areas. Diseases which may explain these x-ray findings include simple coal workers pneumoconiosis (CWP) - stage II, silico-tuberculosis, disseminated tuberculosis, metastatic lung cancer, and other diffuse infiltrative pulmonary diseases.
Coal workers pneumoconiosis - stage II
illustration
-
Coal workers pneumoconiosis, complicated - illustration
This picture shows complicated coal workers pneumoconiosis. There are diffuse, small, light areas (3 to 5 mm) in all areas on both sides of the lungs. There are large light areas which run together with poorly defined borders in the upper areas on both sides of the lungs. Diseases which may explain these X-ray findings include complicated coal workers pneumoconiosis (CWP), silico-tuberculosis, disseminated tuberculosis, metastatic lung cancer, and other diffuse infiltrative pulmonary diseases.
Coal workers pneumoconiosis, complicated
illustration
-
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Review Date: 11/25/2023
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron, Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.