Choking - adult or child over 1 year
Abdominal thrusts - adult or child over 1 year; Heimlich maneuver - adult or child over 1 year; Choking - back blows - adult or child over 1 yearChoking is when someone is having a very hard time breathing because food, a toy, or other object is blocking the throat or windpipe (airway).
A choking person's airway may be blocked so that not enough oxygen reaches the lungs. Without oxygen, brain damage can occur in as little as 4 minutes. Rapid first aid for choking can save a person's life.
Causes
Choking can be caused by any of the following:
- Eating too fast, not chewing food well, or eating with dentures that do not fit well
- Drinking alcohol (even a small amount of alcohol affects awareness)
- Being unconscious and breathing in vomit
- Breathing in small objects (young children)
- Injury to the head and face (for example, swelling, bleeding, or a deformity can cause choking)
- Swallowing problems after a stroke
- Enlarged tonsils or tumors of the neck and throat
- Problems with the esophagus (food pipe or swallowing tube)
Symptoms
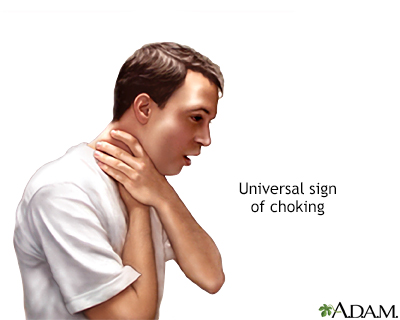
When an older child or adult is choking, they will often grab their throat with the hand. If the person does not do this, look for these danger signs:
- Inability to speak
- Difficulty breathing
- Noisy breathing or high-pitched sounds while inhaling
- Weak, ineffective coughing
- Bluish skin color (cyanosis)
- Loss of consciousness (unresponsiveness) if blockage is not cleared
First Aid
First ask, "Are you choking? Can you speak?" DO NOT perform first aid if the person is coughing forcefully and is able to speak. A strong cough can dislodge the object. Encourage the person to keep coughing to dislodge the object.
If the person cannot speak or is having a hard time breathing, you need to act fast to help the person. You can perform abdominal thrusts, back blows, or both.
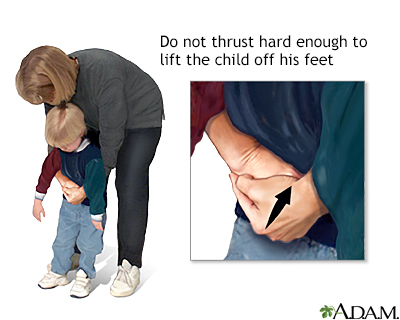
To perform abdominal thrusts (Heimlich maneuver):
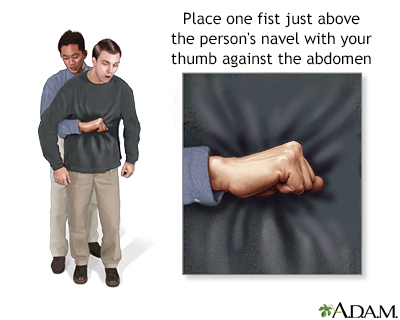
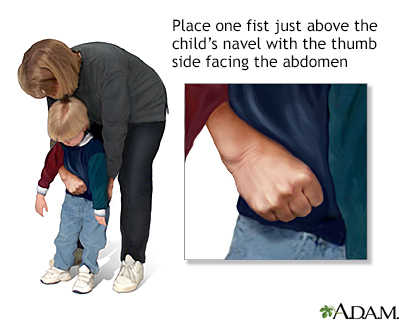
- Stand behind the person and wrap your arms around the person's waist. For a child, you may have to kneel.
- Make a fist with one hand. Place the thumb side of your fist just above the person's navel, well below the breastbone.
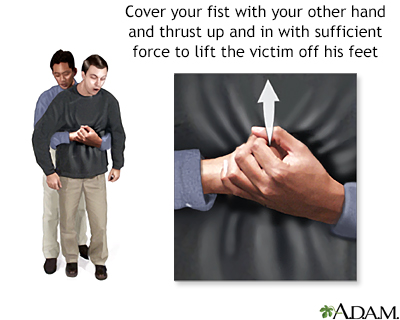
- Grasp the fist tightly with your other hand.
- Make a quick, upward and inward thrust with your fist.
- Check if the object is dislodged.
- Continue these thrusts until the object is dislodged or the person loses consciousness (see below).
To perform back blows:
- Stand behind the person. For child, you may have to kneel.
- Wrap one arm around to support the person's upper body. Lean the person forward until the chest is about parallel to the ground.
- Use the heel of your other hand to deliver a firm blow between the person's shoulder blades.
- Check if the object is dislodged.
- Continue back blows until the object is dislodged or the person loses consciousness (see below).
To perform abdominal thrusts AND back blows (5-and-5 approach):
- Give 5 back blows, as described above.
- If the object is not dislodged, give 5 abdominal thrusts.
- Keep performing the 5-and-5 until the object is dislodged or the person loses consciousness (see below).
IF THE PERSON FAINTS OR LOSES CONSCIOUSNESS
- Lower the person to the floor.
- Call 911 or the local emergency number or tell someone else to do so.
- Begin CPR. Chest compressions may help dislodge the object. Abdominal thrusts are for a conscious choking victim. Chest compressions are for an unconscious choking victim.
CPR
CPR stands for cardiopulmonary resuscitation. It is a lifesaving procedure that is done when someone's breathing or heartbeat has stopped. This may...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - If you see something blocking the airway and it is loose, try to remove it. If the object is lodged in the person's throat, DO NOT try to grasp it. This can push the object farther into the airway.
FOR PREGNANT OR OBESE PEOPLE
- Wrap your arms around the person's CHEST.
- Place your fist on the MIDDLE of the breastbone between the nipples.
- Make firm, backward thrusts.
After removing the object that caused the choking, keep the person still and get medical help. Anyone who is choking should have a medical examination. Complications can occur not only from the choking, but also from the first aid measures that were taken.
Do Not
- DO NOT interfere if the person is coughing forcefully, is able to speak, or is able to breathe in and out adequately. But, be ready to act right away if the person's symptoms get worse.
- DO NOT force open the person's mouth to try to grasp and pull out the object if the person is conscious. Perform abdominal thrusts and/or back blows to try to expel the object.
When to Contact a Medical Professional
Seek medical help right away if you find someone unconscious.
When the person is choking:
- Tell someone to call 911 or the local emergency number while you begin first aid/CPR.
- If you are alone, shout for help and begin first aid/CPR.
After the object is successfully dislodged, the person should see a health care provider because complications can arise.
In the days following a choking episode, contact the provider right away if the person develops:
- A cough that does not go away
- Fever
- Difficulty swallowing or speaking
- Shortness of breath
-
Wheezing
Wheezing
Wheezing is a high-pitched whistling sound during breathing. It occurs when air moves through narrowed breathing tubes in the lungs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
The above signs may indicate:
- The object entered the lung instead of being expelled
- Injury to the voice box (larynx)
Prevention
To prevent choking:
- Eat slowly and chew food thoroughly.
- Make sure dentures fit properly.
- Do not drink too much alcohol before or during eating.
- Keep small objects away from young children.
References
American Red Cross. First Aid/CPR/AED Participant's Manual. 2nd ed. Dallas, TX: American Red Cross; 2016. www.pdfdrive.com/american-red-cross-first-aidcpraed-d128296673.html. Accessed February 20, 2023.
Duff JP, Topjian AA, Berg MD, et al. 2019 American Heart Association focused update on pediatric basic life support: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2020;145(1):e20191358. PMID: 31727861 pubmed.ncbi.nlm.nih.gov/31727861/.
Easter JS. Pediatric resuscitation. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 158.
Goodloe JM, Soulek J. Foreign bodies. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 51.
Haas NL, Kurz MC. Adult resuscitation. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 5.
Kleinman ME, Goldberger ZD, Rea T, et al. 2017 American Heart Association focused update on adult basic life support and cardiopulmonary resuscitation quality: an update to the American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2018;137(1):e7-e13. PMID: 29114008 pubmed.ncbi.nlm.nih.gov/29114008/.
-
Gastroesophageal reflux disease and heartburn - InDepth
(In-Depth)
-
Anxiety disorders - InDepth
(In-Depth)
Review Date: 1/2/2023
Reviewed By: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.