Osteoporosis - InDepth
Thin bones - InDepth; Low bone density - InDepth; Metabolic bone disease - InDepth; Hip fracture - osteoporosis - InDepth; Compression fracture - osteoporosis - InDepth; Wrist fracture - osteoporosis - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of osteoporosis.
Highlights
Osteoporosis Risk Factors
- Older age
- Family history of osteoporosis
- Low body weight and small body frame
- Calcium and vitamin D deficiencies
- Smoking
- Heavy alcohol consumption
- Sedentary lifestyle
- Northern European or Asian descent
- Use of corticosteroid medications
- Diagnosis of rheumatoid arthritis
Screening for Osteoporosis
- The American College of Obstetricians and Gynecologists (ACOG) and the US Preventative Services Task Force (USPSTF) recommend that women receive bone mineral density (BMD) screening beginning at age 65. Postmenopausal women younger than age 65 should also be screened if they have significant risk factors for osteoporosis or a history of bone fracture.
- The latest USPSTF recommendations conclude that there is insufficient evidence to evaluate the benefits and harms of screening for osteoporosis in men.
- Current practice recommends BMD retesting every 2 years. However, some research suggests that certain women may be able to wait a much longer time between their screening tests, perhaps as long as 5 to 15 years. Discuss with your doctor how often you should be tested.
In men the decision to screen for osteoporosis is based on individual risk factors, including:
- Radiographic osteopenia
- History of low-trauma fractures
- Loss of more than 1.5 inches in height
- Long-term glucocorticoid therapy
- Androgen deprivation therapy for prostate cancer
- Hypogonadism
- Primary hyperparathyroidism
- Intestinal disorders
Calcium and Vitamin D Supplement Recommendations in Healthy Women
Healthy postmenopausal women with good diets do not need to take calcium and vitamin D supplements, according to recommendations from the USPSTF. According to the USPSTF, daily low-dose amounts of vitamin D and calcium supplements do not prevent fractures in healthy people and can increase the risk for kidney stones. The USPSTF also notes that there is currently no definition on what exact levels indicate vitamin D deficiency. Talk with your health care provider about whether or not you need these supplements.
Introduction
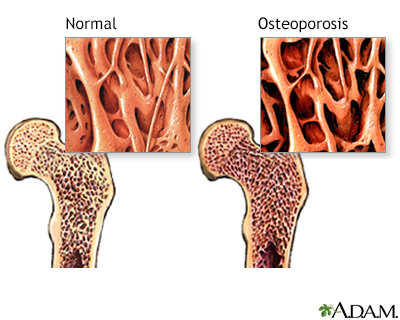
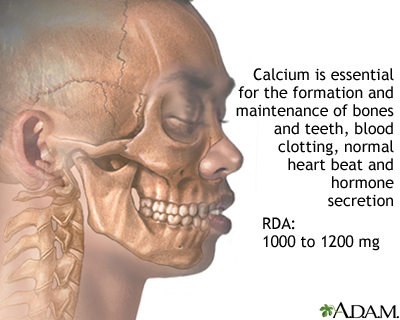
Osteoporosis is a progressive and usually age-related skeletal disease in which bones become thin, weak, brittle, and prone to fracture. Osteoporosis literally means "porous bones." Thinning bones are caused by loss of bone density. Calcium and other minerals contribute to the bone mineral density (BMD) that helps strengthen and protect bones.
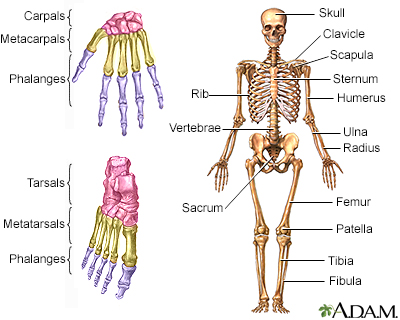
The skeleton consists of groups of bones that protect and move the body.
The Bones
Bones are made of living tissue that is constantly being broken down and formed again. The balance of bone buildup (formation) and breakdown (resorption) is controlled by a complex mix of hormones and chemical factors. If bone resorption occurs at a greater rate than bone formation, your bones lose density and you are at increased risk for osteoporosis.
Until a healthy adult is around age 30, the process of formation and resorption is a nearly perfectly coupled system, with one phase balancing the other. As a person ages, or in the presence of certain conditions, this system breaks down and the two processes become out of sync. Eventually, the breakdown of bone overtakes the buildup.
In women, estrogen loss after menopause is particularly associated with rapid resorption and loss of bone density. Postmenopausal women are therefore at highest risk for osteoporosis and subsequent fractures.
Causes
Estrogen and Testosterone
Women experience a rapid decline in bone density after menopause, when the ovaries stop producing estrogen. Estrogen can have an impact on bone density in various ways, including slowing bone breakdown (resorption).
In men, the most important androgen (male hormone) is testosterone. Androgens are converted to estrogen in various parts of a man's body, including bone. As men age, declining levels of testosterone and estrogen can contribute to bone density loss. Both hormones are important for bone strength in men.
Vitamin D and Parathyroid Hormone Imbalances
Low levels of vitamin D and high levels of parathyroid hormone (PTH) are associated with bone density loss in women after menopause:
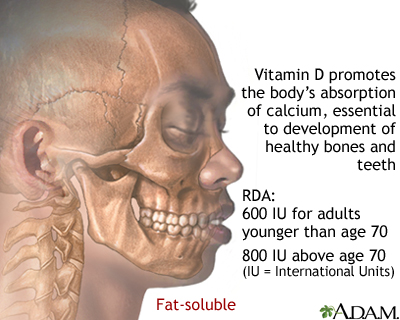
- Vitamin D is a vitamin with hormone-like properties. It is essential for the absorption of calcium and for normal bone growth. Lower levels result in impaired calcium absorption, which in turn causes an increase in parathyroid hormone (PTH).
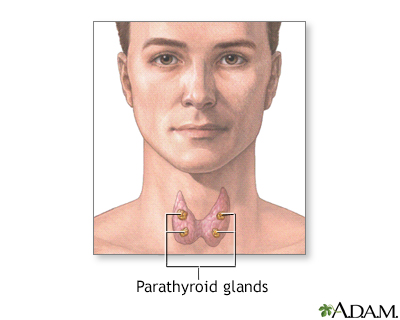
- Parathyroid hormone is produced by the parathyroid glands. These are four small glands located on the surface of the thyroid gland. They regulate calcium levels in the blood. When calcium levels are low, the glands secrete more PTH, which then increases blood calcium levels. Persistently high levels of PTH stimulate bone resorption and lead to bone mineral loss.
Other Causes
Secondary osteoporosis results from medications or other medical conditions.
Medications
Medications that can cause osteoporosis include:
- Oral corticosteroids (also called steroids or glucocorticoids) can reduce bone mass. Inhaled steroids may also cause bone loss when taken at higher doses for long periods of time.
- Loop diuretics, such as furosemide (Lasix, generic), increase the kidneys' excretion of calcium, which can lead to thinning bones.
- Hormonal contraceptives that use progestin without estrogen (such as Depo-Provera injection or other progestin-based contraceptives) can cause loss of bone density.
- Anticonvulsant (anti-seizure) drugs increase the risk for bone loss (as does epilepsy itself).
- Proton pump inhibitors (PPIs), which are used to treat gastroesophageal reflux disease ("heartburn"), can increase the risk for bone loss and fractures when they are used at high doses for more than a year. These drugs include omeprazole (Prilosec, generic), lansoprazole (Prevacid, generic), and esomeprazole (Nexium).
- Other drugs that increase the risk for bone loss include the blood-thinning drug heparin, and hormonal drugs that suppress estrogen (such as gonadotropin-releasing hormone agonists and aromatase inhibitors).
Medical Conditions
Osteoporosis can be secondary to many other medical conditions. They include alcoholism, diabetes, rheumatoid arthritis, thyroid imbalances, liver or kidney disease, Crohn disease, celiac disease, and anorexia nervosa.
Risk Factors
The main risk factors for osteoporosis are:
- Female sex
- Age over 65
- Menopause
- Low body weight
- Smoking and excessive alcohol use
- Family history of hip fractures associated with osteoporosis
- Northern European or Asian descent
- Use of corticosteroids or other medications that promote bone loss
Sex
Women are much more likely to develop osteoporosis than men. Men start with higher bone density and lose calcium at a slower rate than women, which is why their risk is lower. Nevertheless, older men are also at risk for osteoporosis.
Age
As people age, their risks for osteoporosis increase. Aging causes bones to thin and weaken. Osteoporosis is most common among postmenopausal women, and screening for low bone density is recommended for all women over age 65.
Ethnicity
Although adults from all ethnic groups are susceptible to developing osteoporosis, white and Asian women and men face a comparatively greater risk.
Body Type
Osteoporosis is more common in people who have a small, thin body frame and bone structure. Low body mass index (a BMI less than 21) is a risk factor for osteoporosis.
Family History
Osteoporosis tends to run in families. People whose parents had a hip fracture due to osteoporosis are themselves at increased risk for osteoporosis.
Hormonal Deficiencies
Women
Estrogen deficiency is a primary risk factor for osteoporosis in women. Estrogen deficiency is associated with:
- Menopause
- Surgical removal of ovaries (oophorectomy)
- Eating disorders such as anorexia nervosa
Men
Low levels of testosterone increase osteoporosis risk. Certain types of medical conditions (hypogonadism) and treatments (prostate cancer androgen deprivation) can cause testosterone deficiency.
Lifestyle Factors
Dietary Factors
Diet plays an important role in both preventing and speeding up bone loss in men and women. Calcium and vitamin D deficiencies are risk factors for osteoporosis.
The body requires adequate vitamin D in order to absorb calcium. In the United States, many food sources of calcium, such as milk, are fortified with vitamin D.
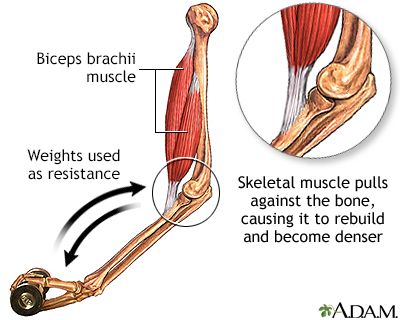
Exercise
Lack of weight-bearing exercise and a sedentary lifestyle increase the risk for osteoporosis. People who are chair-bound or bedbound due to medical infirmities and who do not bear weight on the bones are at risk for osteoporosis.
Smoking
Cigarette smoking can affect calcium absorption and estrogen levels.
Alcohol
Excessive consumption of alcoholic beverages can increase the risk for bone loss.
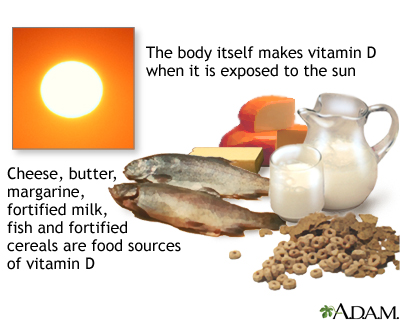
Lack of Sunlight
Vitamin D is made in the skin using energy from the ultraviolet rays in sunlight. Vitamin D is necessary for the absorption of calcium in the stomach and gastrointestinal tract, and is the essential companion to calcium in maintaining strong bones.
Risk Factors in Children and Adolescents
The maximum density that bones achieve during the growing years affects whether a person goes on to develop osteoporosis. People, usually women, who never develop adequate peak bone mass in early life are at high risk for osteoporosis later on.
Risk factors that increase the risk for low peak bone mass in children include:
- Premature birth
- Malnourishment
- Anorexia nervosa
- Delayed puberty or abnormal absence of menstrual periods
- Chronic disease
Exercise and good nutrition are very important during the first three decades of life, when peak bone mass is gained. They are excellent safeguards against osteoporosis (and other health problems).
Complications
Low bone density increases the risk for fracture. Bone fractures are the most serious complication of osteoporosis.
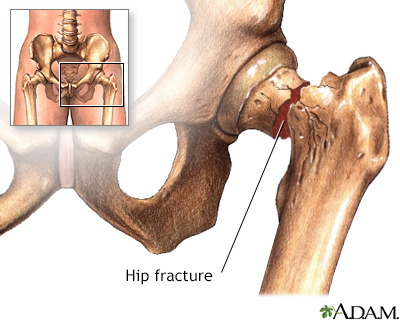
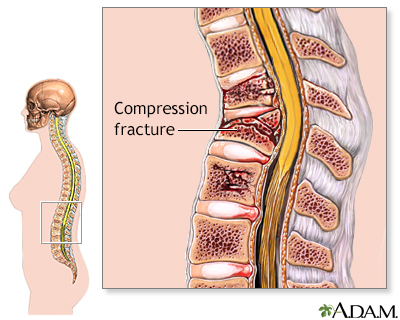
Spinal vertebral fractures (compression fractures) are the most common type of osteoporosis-related fracture, followed by hip fractures, wrist fractures, and other types of broken bones. About 80% of these fractures occur after relatively minor falls or accidents. Compression fractures can occur, without falling, from even everyday motions such as bending or turning.
Hip fractures, in addition to causing disability, can increase the risk of early death. Complications of hip fractures include hospital-acquired infections and blood clots in the lungs.
Symptoms
Osteoporosis is usually asymptomatic until a fracture occurs, so bone density testing is important. A fracture of the spine, wrist, or hip is often the first sign of osteoporosis. These fractures can occur even after relatively minor trauma, such as bumping into an object or falling from a standing position. They can also occur from simple movements such as reaching, turning, or bending over.
Compression fractures occur in the vertebrae of the spine as a result of weakened bones. These fractures can occur suddenly, most commonly near the waistline or just above or below it.
Compression fractures can cause severe back pain, which can take weeks or months to go away:
- The pain is most commonly felt near where the fracture occurs.
- The pain is sharp and "knife-like."
- The pain may get worse with walking, standing, or sitting. It goes away with lying down and rest.
Compression fractures may be mistaken for arthritis or the aches and pains of aging. Often, they are discovered when x-rays of the spine are done for other reasons.
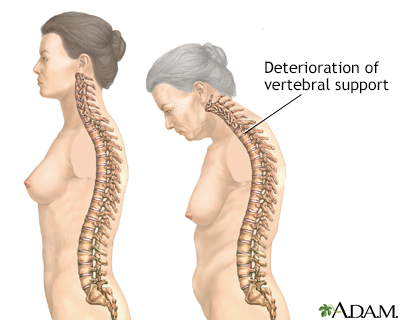
Over time, the following symptoms may occur:
- Loss of height, as much as 6 inches over time
- Stooped-over posture (kyphosis), also known as dowager's hump
Diagnosis
Who Should Get a Bone Density Test
A bone density test can help your health care provider detect osteoporosis and predict your risk for bone fractures. Testing is important because osteoporosis can occur with few or no symptoms.
Bone density testing is recommended for all women age 65 years and older.
There is not full agreement on whether men should undergo this type of testing. Some groups recommend testing of men at age 70 while others state that the evidence is not clear enough to say whether men at this age benefit from screening.
Younger women, as well as men of any age, may also need bone density testing if they have risk factors for osteoporosis. These risk factors include:
- Fracturing a bone after age 50
- Strong family history of osteoporosis
- History of treatment for prostate cancer or breast cancer
- History of medical conditions such as rheumatoid arthritis, diabetes, thyroid imbalances, or anorexia nervosa
- Early menopause (either from natural causes or hysterectomy)
- Long-term use of medications such as corticosteroids, thyroid hormone, or aromatase inhibitors
- Low body weight (less than 127 pounds) or low body mass index (less than 21)
- Significant loss of height
- Long-term tobacco or excessive alcohol use
Tests Used for Measuring Bone Density
Central DXA
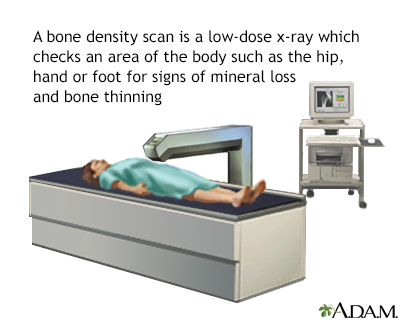
Bone densitometry is a test for measuring bone density and predicting fracture risk. The standard technique for determining bone mineral density (BMD) is called dual-energy x-ray absorptiometry (DXA).
DXA is simple and painless and takes 2 to 4 minutes. It uses low-dose x-rays. You lie on a soft table while the scanner passes over your lower back and hip. The test measures concentrations of calcium and other bone minerals in these areas. You should not take any calcium supplements in the 24 hours before the test.
A radiologist (a doctor specially trained to interpret imaging tests) will review the results of the test and send a report to your health care provider.
Central DXA measures the bone mineral density at the hip, upper thigh bone (femoral neck), and spine.
Other Tests
Other tests may be used, but they are not usually as accurate as DXA. They include ultrasound techniques, DXA of the wrist, heels, fingers, or leg (peripheral DXA) and quantitative computed tomography (QCT) scan.
Screening tests using these technologies are sometimes given at health fairs or other non-medical settings. These screening tests typically measure peripheral bone density in the heels, fingers, or leg bones. The results of these tests may vary from DXA measurements of the spine and hip. While these peripheral tests may help indicate who requires further BMD testing, a central DXA test is required to diagnose osteoporosis and to monitor treatment response.
Diagnosing Osteoporosis and Predicting the Risk for Fracture
Osteoporosis is diagnosed when bone density has decreased to the point where fractures can result from mild stress, the so-called fracture threshold. This is determined by measuring bone density and comparing the results with the norm, which is defined as the average bone mineral density in the hipbones of a healthy 30-year-old adult.
The doctor then uses this comparison to determine the standard deviation (SD) from this norm. Standard deviation results are given as Z and T scores:
- The T score gives the standard deviation of the person tested in relationship to the norm in young adults. Doctors often use the T-score and other risk factors to determine the risk for fracture.
- The Z score gives the standard deviation of the person tested in relationship to the norm in other people of the same age group and body size. Z scores may be used for diagnosing osteoporosis in younger men and women. They are not normally used for postmenopausal women or for men age 50 and older.
Results of T-scores indicate:
- Higher than -1 indicates normal bone density.
- Between -1 and -2.5 indicates low bone density (osteopenia).
- A score of -2.5 or lower indicates a diagnosis of osteoporosis.
The lower the T-score, the lower the bone density, and the greater the risk for fracture. In general, doctors recommend beginning medication when T-scores are -2.5 or below.
People who have other risk factors may need to begin medication when they have osteopenia (scores between -1 and -2.5). Osteopenia refers to bone mineral density that is lower than normal, but not low enough to be classified as osteoporosis. Osteopenia is considered a precursor to osteoporosis.
Doctors don't yet know the best testing schedule for people whose first test does not reveal osteoporosis. Current practice recommends that older people have a bone mineral density test every 2 years. However, some recent research suggests that low-risk women who have normal test results may be able to wait for up to 15 years to be rescreened. (Women at higher risk would need to have another test at much shorter intervals.) Discuss with your doctor how often you should be tested based on your individual risk factors.
Laboratory Tests
In certain cases, your health care provider may recommend that you have a blood test to measure your vitamin D levels. A standard test measures 25-hydroxyvitamin D, also called 25(OH)D. Depending on the results, your provider may recommend that you take a vitamin D supplement if you are at high risk for fractures. There is currently no consensus on what levels of vitamin D indicate deficiency, or what the optimal levels should be.
Lifestyle Changes
Healthy lifestyle habits, including adequate intake of calcium and vitamin D, are important for preventing osteoporosis and supporting medical treatment.
Calcium and Vitamin D
A combination of calcium and vitamin D may reduce the risk of osteoporosis. (For strong bones, people need enough of both calcium and vitamin D.) The best sources are from calcium-rich and vitamin D-fortified foods.
The National Osteoporosis Foundation (NOF) recommends:
- Adults under age 50 should have 1,000 mg of calcium and 400 to 800 IU of vitamin D daily.
- Calcium supplements should be used only if dietary intake is not adequate. In adults 50 years or older, the average daily dietary calcium intake is between 600 and 700 mg per day.
- Adult men age 50 to 70 should have 1,000 mg of calcium, and 1,200 mg when over 70.
- Adult women age 50 and older should have 1,200 mg of calcium.
- Calcium intake above these amounts has not shown to provide additional bone strength and may increase the risk of kidney stones, heart disease, and stroke.
- For vitamin D, the Institute of Medicine recommends 600 IU per day through age 70 and 800 IU per day over age 70.
Sources
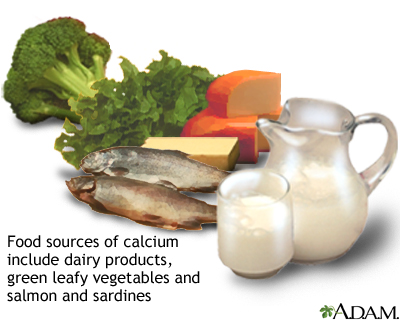
Good dietary sources of calcium include:
- Milk, yogurt, and other dairy products
- Dark green vegetables such as collard greens, kale, and broccoli
- Sardines and salmon with bones
- Calcium-fortified foods and beverages such as cereals, orange juice, and soymilk
Certain types of foods can interfere with calcium absorption. These include foods high in oxalate (such as spinach and beet greens) or phytate (peas, pinto beans, navy beans, wheat bran). Diets high in animal protein, sodium, or caffeine may also interfere with calcium absorption.
Sources of vitamin D include:
- Fatty fish such as salmon, mackerel, and tuna
- Egg yolks
- Liver
- Vitamin D-fortified milk, orange juice, soy milk, or cereals
- Sunlight
However, many Americans do not get enough vitamin D solely from diet or exposure to sunlight.
Supplements
Doctors are currently reconsidering the use of calcium and vitamin D supplements based on studies suggesting that supplements do not make much difference in bone mineral density protection. The U.S. Preventive Services Task Force (USPSTF) advises that healthy postmenopausal women don't need to take these supplements.
According to the USPSTF, taking daily low-dose vitamin D supplements (less than 400 IU), with or without calcium supplements (less than 1,000 mg), does not prevent fractures. For higher doses, the USPSTF says there is not enough evidence to make a recommendation. In addition to possible lack of benefit, these supplements are associated (even at lower doses) with certain risks, like kidney stones.
Vitamin D and calcium supplements may be appropriate for certain people, including those who do not get enough vitamin D through sunlight exposure and those who do not consume enough calcium in their diet. They are also helpful for people who have been diagnosed with osteoporosis.
Calcium and vitamin D supplements can be taken as separate supplements or as a combination supplement. If separate preparations are used, they do not need to be taken at the same time.
- Calcium supplements include calcium carbonate (Caltrate, Os-Cal, Tums), calcium citrate (Citracal), calcium gluconate, and calcium lactate. Although each kind provides calcium, they all have different calcium concentrations, absorption capabilities, and other actions.
- Vitamin D is available either as D2 (ergocalciferol) or D3 (cholecalciferol). They work equally well for bone health.
Given the controversies over the benefits and safety of these supplements, be sure to discuss with your doctor whether supplements are a good choice for you. As an alternative to supplements, many doctors recommend making dietary changes to increase calcium and vitamin D intake, and getting 15 minutes a day of sun exposure.
Exercise
Exercise is very important for slowing the progression of osteoporosis. Although mild exercise does not protect bones, moderate exercise (more than 3 days a week for more than a total of 90 minutes a week) reduces the risk for osteoporosis and fracture in both older men and women. Exercise should be regular and life-long. Before beginning any strenuous exercise program, talk to your doctor.
Some exercises may be better than others:
- Weight-bearing exercise applies tension to muscle and bone and can help increase bone density in younger people. Weight training is also beneficial for middle-aged and older people.
- Regular brisk long walks improve bone density and mobility. Most older people should avoid high-impact aerobic exercises (step aerobics), which increase the risk for osteoporotic fractures. Although low-impact aerobic exercises such as swimming and bicycling do not increase bone density, they are excellent for cardiovascular fitness and should be part of a regular regimen.
- Exercises specifically targeted to strengthen the back may help prevent fractures later in life and can be beneficial in improving posture and reducing kyphosis (hunchback).
- Low-impact exercises that improve concentration, balance, and strength, particularly yoga and tai chi, may help decrease the risk of falling.
Exercise plays an important role in preserving bone density in the aging person. Studies show that exercises requiring muscles to pull on bones cause the bones to retain and possibly gain calcium and strength.
Other Lifestyle Factors
Other lifestyle changes that can help prevent osteoporosis include:
- Limit alcohol consumption. Excessive drinking is associated with brittle bones.
- Limit caffeine consumption. Caffeine may interfere with the body's ability to absorb calcium.
- Quit smoking. The risk for osteoporosis from cigarette smoking appears to diminish after quitting.
Preventing Falls and Fractures
An important component in reducing the risk for fractures is preventing falls. Risk factors for falling include:
- Slow walking
- Inability to walk in a straight line
- Certain medications (such as tranquilizers and sleeping pills)
- Low blood pressure when rising in the morning
- Poor vision
Recommendations for preventing falls or fractures from falls include:
- Exercise to maintain strength and balance if there are no conflicting medical conditions.
- Do not use loose rugs on floors.
- Move any obstructions for walking, such as loose cords or very low pieces of furniture, away from traveled areas.
- Keep rooms well lit.
- Have regular eye checkups.
- Consider installing grab bars in bathrooms, especially near the shower, tub, and toilet.
- Use of an assistive device such as a cane or walker.
Medications
Two types of drugs are used to prevent and treat osteoporosis:
- Antiresorptive Drugs. Antiresorptives include bisphosphonates, selective estrogen-receptor modulators (SERMs), denosumab, and calcitonin. Bisphosphonates are the standard drugs used for osteoporosis. These drugs block resorption (preventing bone breakdown), which slows the rate of bone remodeling, but they cannot rebuild bone. Because resorption and reformation occur naturally as a continuous process, blocking resorption may eventually also reduce bone formation.
- Anabolic (Bone-Forming) Drugs. Drugs that rebuild bone are known as anabolics. The primary anabolic drug is low-dose parathyroid hormone (PTH), which is administered through injections. This drug may help restore bone and prevent fractures. Romosozumab is another bone-forming drug recently approved by the FDA for osteoporosis.
Both types of drugs are effective in preventing bone loss and fractures, although they may cause different types of side effects. The United States Preventive Services Task Force (USPSTF) recommends that these drugs should be prescribed only to people who have been diagnosed with osteoporosis.
Bisphosphonates
Bisphosphonates are the primary drugs for preventing and treating osteoporosis. They can help reduce the risk for both spinal and hip fractures, including among people with prior bone breaks.
Studies indicate that these drugs are effective and safe for up to 5 years. However, bone loss continues with bisphosphonates. This may be because rebuilding bone is a continuous cycle that requires two phases: bone breakdown (resorption) and bone formation. Over time, drugs that block bone resorption interfere with bone formation, the second half of the process.
Candidates
Clinical guidelines recommend that the following people should take or consider taking bisphosphonates:
- T score of -2.5 or lower on a DXA scan.
- T score between -1 and -2.5 (indicates low bone density [osteopenia]) and a history of fractures.
- T score between -1 and -2.5 and FRAX score indicating a greater than 3% risk of hip fracture or 20% risk of any fracture in the next 10 years.
Brands
Bisphosphonates for osteoporosis prevention and treatment are available in different forms:
- Oral bisphosphonates. These pills include alendronate (Fosamax, generic), risedronate (Actonel, generic), and ibandronate (Boniva, generic). Alendronate and risedronate are taken once a week. Ibandronate is available as a once-monthly pill. Risedronate is also available as a once-a-month pill and in a pill that contains calcium. Alendronate is available in a formulation that has vitamin D. Risedronate and alendronate are approved for both men and women.
- Injectable bisphosphonates. Zoledronic acid (Reclast) is approved for the treatment and prevention of osteoporosis in postmenopausal women. It is given as a once-yearly injection. The injectable form of ibandronate (Boniva) requires injections 4 times a year. Injectable bisphosphonates are an alternative for people who may have difficulty swallowing pills or sitting upright after oral bisphosphonate treatment.
Side Effects
The most common side effects of bisphosphonates are gastrointestinal problems, particularly stomach cramps and heartburn. Other side effects may include irritation of the esophagus (the tube that connects the mouth to the stomach) and ulcers in the esophagus or stomach. Some people experience muscle and joint pain.
To avoid stomach problems:
- Take the pill on an empty stomach in the morning with 6 to 8 ounces of water (not juice or carbonated or mineral water).
- After taking the pill, remain in an upright position. Do not eat or drink for at least 30 to 60 minutes. (Check your drug's dosing instructions for the exact time.)
- If you develop chest pain, heartburn, or difficulty swallowing, stop taking the drug and see your health care provider.
Other Concerns
The FDA is currently reviewing whether long-term (more than 3 to 5 years) use of bisphosphonate drugs provides any benefits for fracture prevention. Possible concerns for long-term use of bisphosphonates are increased risks for thigh bone (femoral) fractures, esophageal cancer, and osteonecrosis (bone death) of the jaw.
The FDA recommends that health care providers periodically reevaluate people who have been on bisphosphonates for more than 5 years. People who take these drugs should inform their providers if they experience any new thigh or groin pain, swallowing difficulties, or jaw or gum discomfort. Do not stop taking your medication unless your provider tells you to do so. Most people who experience osteonecrosis of the jaw do so after a dental procedure, such as tooth extraction. You should inform your dentist if you are prescribed a bisphosphonate.
For the injectable drug zoledronic acid (Reclast), kidney failure is a rare but serious side effect. Zoledronic acid should not be used by people who have risk factors for kidney failure.
Denosumab (Prolia)
Denosumab (Prolia) is a drug approved for treatment of osteoporosis in postmenopausal women who are at high risk for fracture. Denosumab is the only biologic drug approved for osteoporosis. It is considered an antiresorptive drug, but it works in a different way than bisphosphonates. It is a monoclonal antibody that works by targeting RANKL, a chemical factor involved with bone resorption.
Denosumab slows down the bone-breakdown process. However, because it also slows down the bone buildup and remodeling process, it is unclear what its long-term effects may be. Possible concerns are that denosumab may slow the healing time for broken bones or cause unusual fractures. For now, denosumab is recommended for women who cannot tolerate or who have not been helped by other osteoporosis treatments.
Denosumab is given as an injection in a doctor's office twice a year (once every 6 months). Common side effects include back pain, pain in the arms and legs, high cholesterol levels, muscle pain, and bladder infection. Denosumab can lower calcium levels and should not be taken by women who have low blood calcium levels (hypocalcemia) until this condition is corrected.
Because denosumab is a biologic drug, it can affect or weaken the immune system and may increase the risk for serious infections. Other potential adverse effects include inflammation of the skin (dermatitis, rash, eczema) and inflammation of the inner lining of the heart (endocarditis). Denosumab may increase the risk of jaw bone problems such as osteonecrosis. Inform your dentist if you have been prescribed denosumab.
SERMs
Selective estrogen-receptor modulators (SERMs) are a class of drugs that are similar, but not identical, to estrogen. They can provide the bone benefits of estrogen without increasing the risks for estrogen-related breast and uterine cancers.
Raloxifene (Evista)
Raloxifene (Evista) is the only SERM approved for both treatment and prevention of osteoporosis in postmenopausal women. Raloxifene is recommended for postmenopausal women with low bone mass or younger postmenopausal women with osteoporosis. It may help prevent bone loss and reduce the risk of vertebral (spine) fractures. It is less clear how effective it is for preventing other types of fractures. Raloxifene is taken as a pill once a day. Common mild side effects include hot flashes, joint pain, and swelling of the legs, feet, and ankles.
Bazedoxifene and Conjugated Estrogens (Duavee)
Duavee is a drug that combines the SERM bazedoxifene with the conjugated estrogens used in hormone replacement therapy for menopause. The medication is approved both to treat moderate-to-severe menopausal symptoms such as hot flashes, and to prevent postmenopausal osteoporosis. When Duavee is used solely for the prevention of osteoporosis, the FDA recommends that it should be reserved for high-risk women, and that other, non-estrogen drugs should be tried first. Common side effects include muscle spasms, nausea, diarrhea, and upset stomach.
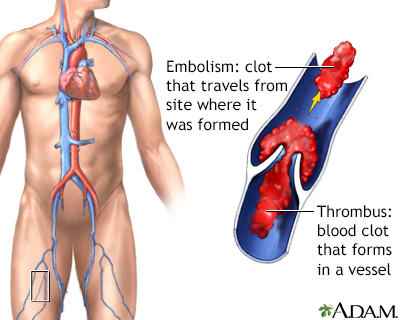
A thrombus is a clot that forms in a blood vessel and remains there. An embolism is a clot that travels from the site where it formed to another location in the body.
Serious Side Effects
All SERMs increase the risk for blood clots in the veins. Because of this side effect, these drugs also increase the risk for stroke (but not other types of cardiovascular disease). These side effects, though rare, are very serious. Women should not take a SERM drug if they have a history of blood clots, or if they have certain risk factors for stroke and heart disease.
Parathyroid Hormone
Teriparatide (Forteo) and abaloparatide (Tymlos) are amino acid synthetic analogs of the parathyroid hormone (PTH). PTH analogs may help reduce the risks for spinal and non-spinal fractures in people with osteoporosis. Although high persistent levels of PTH can cause osteoporosis, daily injections of low doses of analogs of this hormone actually stimulate bone production and increase bone mineral density. Teriparatide and abaloparatide are given as subcutaneous injections and are usually recommended for people with osteoporosis who are at high risk of fracture.
Side effects of PTH analogs are generally mild and include nausea, dizziness, and leg cramps. No significant complications have been reported to date.
Early animal studies reported bone tumors in mice that were given parathyroid long-term. Such effects have not been observed in humans to date. However, people with Paget disease, (a disorder in which bone thickens but also weakens), should not take PTH analogs, because they are at higher than normal risk for bone tumors.
Romosozumab
Romosozumab (Evenity) was recently approved by the FDA to treat osteoporosis in postmenopausal women with a high risk of fracture. This drug is a monoclonal antibody that works by targeting a protein called sclerostin and improving bone formation. It is given by monthly injection.
Romosozumab may increase the risk for heart attacks and stroke, and therefore should not be used in patients with a recent history of cardiovascular events. In patients with other cardiovascular risk factors, benefits should be weighed against potential risk.
Calcitonin
Produced by the thyroid gland, natural calcitonin regulates calcium levels by inhibiting the osteoclastic activity, the breakdown of bone. The drug version, calcitonin salmon, is derived from salmon and is available as a nasal spray (Miacalcin, Fortical, generic) and an injected form (Miacalcin, generic). Calcitonin is used to treat, not prevent, osteoporosis.
Side effects may include headache, dizziness, anorexia, diarrhea, skin rashes, and edema (swelling). The most common adverse effect experienced with the injection is nausea, with or without vomiting. The nasal spray may cause nosebleeds, sinusitis, and inflammation of the membranes in the nose. Many people who take calcitonin develop resistance or allergic reactions after long-term use.
In 2013, an FDA advisory committee recommended against the use of calcitonin products for osteoporosis due to concerns that the drug may increase the risk for cancer. However, due to a lack of evidence of a causal relationship, the FDA continues to allow calcitonin products to be used in postmenopausal women with osteoporosis. Calcitonin products are only indicated in patients for whom other treatments are not suitable and patients are encouraged to discuss their risk and options with their providers.
Hormone Therapy
Hormone therapy (HT) is mainly used for short-term treatment of menopause symptoms, such as hot flashes. HT was formerly used to prevent osteoporosis, but it is rarely used for this purpose today. Studies showed that the estrogen in HT increases the risk for breast cancer, blood clots, strokes, and heart attacks. For this reason, women need to balance the benefits of HT on bone-loss protection with the risks it carries for other serious health conditions.
The United States Preventive Services Task Force (USPSTF) recommends against the use of hormone therapy for prevention of osteoporosis or other chronic health conditions.
Resources
- National Osteoporosis Foundation -- www.nof.org
- National Institute of Arthritis and Musculoskeletal and Skin Diseases -- www.bones.nih.gov/health-info/bone/bone-basics
- International Osteoporosis Foundation -- www.iofbonehealth.org
- North American Menopause Society -- www.menopause.org
References
Akkawi I, Zmerly H. Osteoporosis: current concepts. Joints. 2018;6(2):122-127. PMID: 30051110 pubmed.ncbi.nlm.nih.gov/30051110/.
Black DM, Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2016;374(3):254-262. PMID: 26789873 pubmed.ncbi.nlm.nih.gov/26789873/.
Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract. 2020;26(Suppl 1):1-46. PMID: 32427503 pubmed.ncbi.nlm.nih.gov/32427503/.
Chapurlat RD, Genant HK. Osteoporosis. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 69.
Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364-376. PMID: 30696576 pubmed.ncbi.nlm.nih.gov/30696576/.
De Paula FJA, Black DM, Rosen CJ. Osteoporosis: basic and clinical aspects. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 30.
Eastell R, Rosen CJ, Black DM, et al. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1595-1622. PMID: 30907953 pubmed.ncbi.nlm.nih.gov/30907953/.
Expert Panel on Musculoskeletal Imaging; Ward RJ, Roberts CC, Bencardino JT, et al. ACR Appropriateness Criteria Osteoporosis and Bone Mineral Density. J Am Coll Radiol. 2017;14(5S):S189-S202. PMID: 28473075 pubmed.ncbi.nlm.nih.gov/28473075/.
Kanis JA, Cooper C, Rizzoli R, Reginster JY; Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30(1):3-44. PMID: 30324412 pubmed.ncbi.nlm.nih.gov/30324412/.
Kendler DL, Bauer DC, Davison KS, et al. Vertebral fractures: clinical importance and management. Am J Med. 2016;129(2):221.e1-221.e10. PMID: 26524708 pubmed.ncbi.nlm.nih.gov/26524708/.
LeFevre ML; U.S. Preventive Services Task Force. Screening for vitamin D deficiency in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;162(2):133-140. PMID: 25419853 pubmed.ncbi.nlm.nih.gov/25419853/.
Moyer VA; U.S. Preventive Services Task Force. Menopausal hormone therapy for the primary prevention of chronic conditions: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;158(1):47-54. PMID: 23090711 pubmed.ncbi.nlm.nih.gov/23090711/.
Moyer VA; U.S. Preventive Services Task Force. Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;158(9):691-696. PMID: 23440163 pubmed.ncbi.nlm.nih.gov/23440163/.
Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839. PMID: 28492856 pubmed.ncbi.nlm.nih.gov/28492856/.
Shoback D, Rosen CJ, Black DM, et al. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society guideline update. J Clin Endocrinol Metab. 2020;105(3):dgaa048. PMID: 32068863 pubmed.ncbi.nlm.nih.gov/32068863/.
US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(24):2521-2531. PMID: 29946735 pubmed.ncbi.nlm.nih.gov/29946735/.
US Preventive Services Task Force, Grossman DC, Curry SJ, Owens DK, et al. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(15):1592-1599. PMID: 29677309 pubmed.ncbi.nlm.nih.gov/29677309/.
Vidal M, Thibodaux RJ, Neira LFV, Messina OD. Osteoporosis: a clinical and pharmacological update. Clin Rheumatol. 2019;38(2):385-395. PMID: 30542797 pubmed.ncbi.nlm.nih.gov/30542797/.
Weber TJ. Osteoporosis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier Saunders; 2020:chap 230.
Review Date: 7/26/2021
Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.