Crohn disease - InDepth
Crohn's disease - InDepth; Inflammatory bowel disease - Crohn's disease - InDepth; Regional enteritis - InDepth; Ileitis - InDepth; Granulomatous ileocolitis - InDepth; IBD - Crohn disease - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of Crohn disease.
Highlights
Crohn Disease
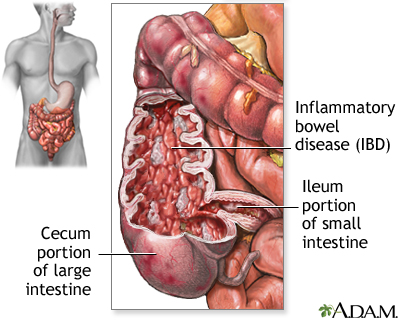
Crohn disease and ulcerative colitis are inflammatory bowel diseases. All inflammatory bowel diseases cause chronic inflammation in the digestive system.
- Crohn disease most commonly occurs at the lower end of the small intestine (ileum) and the beginning of the large intestine (colon), but it can affect any part of the gastrointestinal tract (digestive system) from the mouth to the anus.
- Ulcerative colitis affects only the lining of the large intestine (colon).
Symptoms
Specific symptoms of Crohn disease vary depending on where the disease is located in the intestinal tract (ileum, colon, stomach, duodenum, or jejunum). Common symptoms of Crohn disease include:
- Abdominal pain, usually in lower right side
- Diarrhea
- Weight loss
- Rectal bleeding
- Fever
Complications
Crohn disease can cause many different kinds of complications depending on its severity such as:
- Blockages or obstructions in the intestinal tract due to strictures (narrowing) of the intestine due to chronic inflammation.
- Fistulas and abscesses around the anus; fistulas can also form other parts of the intestinal tract or abdominal wall.
- Malnutrition.
- Increased risk for colorectal cancer.
Treatment for Crohn Disease
Crohn disease is a chronic condition that cannot be cured, but appropriate treatment can help suppress the inflammatory response and manage symptoms. Treatment approaches include:
- Diet and nutrition management
- Drug treatment to resolve symptoms and prevent disease flare-ups
- Surgery if medications and diet and lifestyle changes no longer help
Introduction
Inflammatory bowel disease (IBD) is a general term that includes two main disorders:
-
Ulcerative colitis (UC)
Ulcerative colitis (UC)
An in-depth report on the causes, diagnosis, treatment, and prevention of ulcerative colitis.
 Image
ImageRead Article Now Book Mark Article - Crohn disease (CD)
These two diseases are related, but they are considered separate disorders with somewhat different treatment options. The basic distinctions between UC and CD are location and severity. However, some people with early-stage IBD have features and symptoms of both disorders. (This is called indeterminate colitis.)
Crohn disease is a chronic inflammation of the intestines. It is usually found in the lower end of the small intestine, the ileum, but not infrequently in the colon.
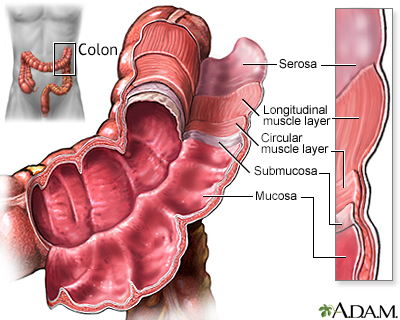
Crohn DiseaseCrohn disease can occur in any part of the gastrointestinal tract (digestive system) from the mouth to the anus. The inflammation associated with Crohn disease affects all layers of the intestine and can extend into the deep layers of the intestinal wall.
Crohn disease is found most often in the area bridging the small and large intestines, specifically in the terminal ileum and the cecum, sometimes referred to as the ileocecal region. Less often, Crohn disease develops in other parts of the gastrointestinal tract, including the anus, stomach, esophagus, and even the mouth. It may affect the entire colon or form a string of connected ulcers in one part of the colon. It may also develop as multiple scattered clusters of ulcers throughout the gastrointestinal tract, skipping healthy tissue in between.
Ulcerative Colitis
Ulcerative colitis is an inflammatory disease that affects only the lining (top layer) of the large intestine (colon) and rectum.
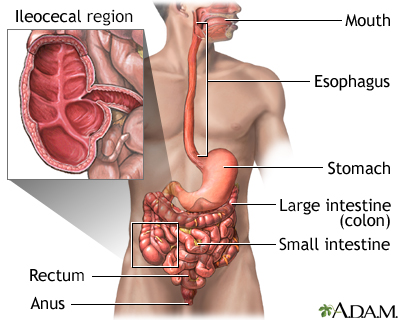
The Gastrointestinal Tract
The gastrointestinal tract (the digestive system) is a tube that extends from the mouth to the anus. It is a complex organ system that first carries food from the mouth down the esophagus to the stomach and then through the small and large intestine to be expelled out through the rectum and anus.
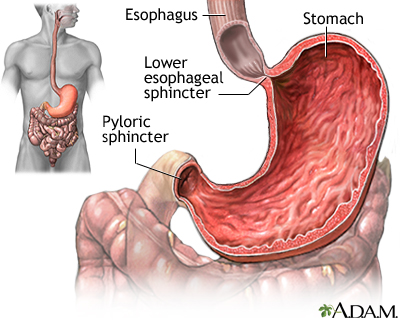
EsophagusThe esophagus, commonly called the food pipe, is a narrow muscular tube, about 9 1/2 inches (24 centimeters) long, that begins below the tongue and ends at the stomach.
StomachIn the stomach, acids and stomach motion break food down into particles small enough so that nutrients can be absorbed by the small intestine.
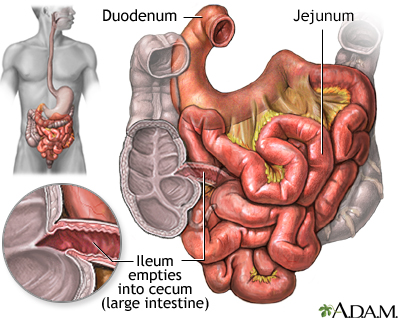
Small IntestineThe small intestine, despite its name, is the longest part of the gastrointestinal tract. It extends from the stomach to the large intestine and is about 20 feet long. Food passes from the stomach through the small intestine's three parts:
- First it enters the
duodenum
- Then the
jejunum
- Finally the
ileum
Most of the digestive process occurs in the small intestine.
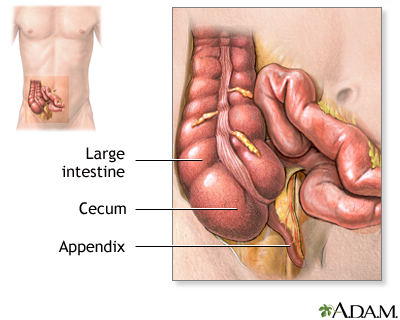
Large IntestineUndigested material, such as plant fiber, is passed next to the large intestine, or colon, mostly in liquid form. The colon is wider than the small intestine but only about 6 feet long. The colon absorbs excess water and salts into the blood. The remaining waste matter is converted to feces through bacterial action. The colon is a continuous structure, but it is characterized as having several components.Cecum and AppendixThe cecum is the first part of the colon. The appendix is attached to the cecum. These structures are located in the lower-right part of the abdomen.- The first section, the
ascending colon
, extends upward from the cecum on the right side of the abdomen. - The second section, the
transverse colon
, crosses the upper abdomen to the left side. - The third section extends downward on the left side of the abdomen toward the pelvis and is called the
descending colon
. - The final section is the
sigmoid colon
.
Causes
Doctors do not know exactly what causes inflammatory bowel disease (IBD). IBD appears to be due to an interaction of many complex factors including:
- Genetics
- Impaired immune system response
- Environmental triggers
The result is an abnormal immune system reaction, which in turn causes an inflammatory response in the body's intestinal regions. Crohn disease and ulcerative colitis are considered autoimmune disorders.
The Inflammatory Response
An inflammatory response occurs when the body tries to protect itself from what it perceives as invasion by a foreign substance (antigen). Antigens may be viruses, bacteria, or other harmful substances.
In Crohn disease and ulcerative colitis, the body mistakenly targets harmless substances (components of food, beneficial bacteria, or the intestinal tissue itself) as harmful. To fight infection, the body releases various chemicals and white blood cells, which in turn produce byproducts that cause chronic inflammation in the intestinal lining. Over time, the inflammation damages and permanently changes the intestinal lining.
Genetic Factors
Genetic factors are certainly involved in IBD. Several identified genes and chromosome locations play a role in the development of ulcerative colitis, Crohn disease, or both. Genetic factors appear to be more important in Crohn disease than ulcerative colitis, although there is evidence that both forms of inflammatory bowel disease have common genetic defects.
Environmental Factors
IBD is much more common in industrialized nations, urban areas, and northern geographical latitudes. It is not clear how or why these factors increase the risk for IBD. It could be that "Western" lifestyle factors (smoking, lack of exercise, diets high in fat and sugar, stress) play a role. However, there is no strong evidence that diet or stress cause Crohn disease or ulcerative colitis, although they can aggravate the conditions.
Other possible environmental causes for Crohn may be reduced exposure to sunlight and subsequent lower levels of Vitamin D, and reduced exposure during childhood to certain types of stomach bacteria and other microorganisms. So far, these theories have not been confirmed.
Risk Factors
About 1 million Americans have inflammatory bowel disease (IBD). About one half of these people have Crohn disease. There are several risk factors for Crohn disease.
Age
Crohn disease can occur at any age, but it is most frequently diagnosed in people ages 15 to 35. About 10% of people with Crohn disease are children under age 18.
Sex
Men and women are almost equally at risk of developing Crohn disease.
Family History
Crohn disease tends to run in families. People who have a first-degree relative (father, mother, brother, sister) with Crohn disease are at significantly increased risk of developing the disorder.
Race and Ethnicity
Among racial categories, the highest prevalence rates of Crohn disease are reported in white populations of North America and Europe. Black and Asian populations have significantly lower prevalence rates of Crohn disease. Jewish people of Ashkenazi (Eastern European) descent are at 4 to 5times higher risk than the general population.
Smoking
Smoking increases the risk of developing Crohn disease, and can worsen the course of the disease. (Conversely, smoking appears to decrease the risk of ulcerative colitis. However, because of the hazards of smoking, it should never be used to protect against ulcerative colitis.)
Appendectomy
Removal of the appendix (appendectomy) may possibly increase the risk of developing Crohn disease, but decrease the risk for ulcerative colitis.
Symptoms
The two major inflammatory bowel diseases, ulcerative colitis and Crohn disease, share certain characteristics:
- Symptoms usually appear in young adults.
- Symptoms can develop gradually or have a sudden onset.
- Crohn disease and ulcerative colitis are chronic conditions. In both diseases, people experience sporadic episodes of symptom flare-ups (relapse) in between symptom-free periods (remission).
- Symptoms can be mild or very severe. Severe symptoms can lead to complications.
Crohn disease and ulcerative colitis can cause similar symptoms but the conditions affect different areas in the gastrointestinal tract. The specific symptoms of Crohn disease vary depending on where the disease is located in the gastrointestinal tract (ileum, colon, stomach, duodenum, or jejunum).
Common symptoms of Crohn disease include:
- Abdominal pain and cramping, usually in lower right side
- Diarrhea, loose stools, and frequent urgent bowel movements
- Rectal bleeding and blood in stools
- Reduced appetite and weight loss
- Fever
- Low energy and fatigue
- Nausea and vomiting (associated with severe abdominal pain)
Other Symptoms
The inflammation associated with inflammatory bowel disease (IBD) can cause symptoms outside of the gastrointestinal tract.
JointsArthritis is the most common non-intestinal symptom. There are three types of arthritis associated with IBD.
Peripheral arthritis
affects the elbows, wrists, knees, and ankles.Axial arthritis
causes stiffness in the lower spine and back. A more severe form of axial arthritis, calledankylosing spondylitis
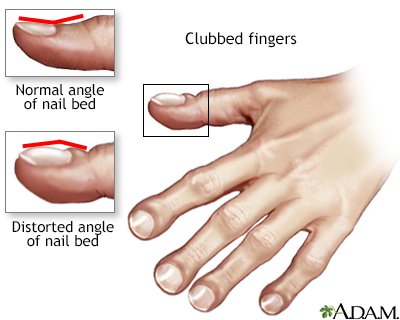
, is often accompanied by inflammation of the eyes, lungs, and heart valves. Ankylosing spondylitis is more common with Crohn disease than ulcerative colitis. People with Crohn disease are also at risk for clubbing (abnormal thickening and widening at the ends of fingers and toes).
There are many types of skin problems associated with IBD. They often tend to appear during disease flare-ups and resolve when symptoms are controlled. Canker sores (mouth ulcers) are very common. People with Crohn disease often have skin tags that surround hemorrhoids around the anal area but these tags are not usually painful or serious.
Skin disorders that tend to be seen more with ulcerative colitis than Crohn disease include red knot-like swellings (erythema nodosum) and pus-filled skin ulcers on the shins and ankles (pyoderma gangrenosum). EyesInflammatory bowel disease is sometimes associated with various eye problems. A common complication is inflammation in the pigmented part of the eye, a condition called uveitis.Complications
Complications in the Intestine
Intestinal BlockageBlockage or obstruction in the intestinal tract is a common complication of Crohn disease. Inflammation from Crohn disease produces scar tissue known as strictures that can constrict the intestines, causing bowel obstruction with severe cramps and vomiting. Strictures usually occur in the small intestine but can also occur in the large intestine.
Fistulas and AbscessesInflammation around the anal area can cause fistulas and abscesses. Fistulas (abnormal channels between tissues) frequently develop from the deep ulcers that can form with Crohn. If fistulas develop between the loops of the small and large intestines, they can interfere with absorption of nutrients. They often lead to pockets of infection, or abscesses, which may become life threatening if not treated.
Malabsorption and MalnutritionMalabsorption is the inability of the intestines to absorb nutrients. In IBD, this occurs as a result of bleeding and diarrhea, as a side effect from some of the medications, or as a result of surgery. Malnutrition usually develops slowly and tends to become severe, with multiple nutritional deficiencies. It is very common in people with Crohn disease.
Toxic MegacolonToxic megacolon is a serious complication that can occur if inflammation spreads into the deeper layers of the colon. In such cases, the colon enlarges and becomes paralyzed. In severe cases, it may rupture, which is a life-threatening event that requires emergency surgery.
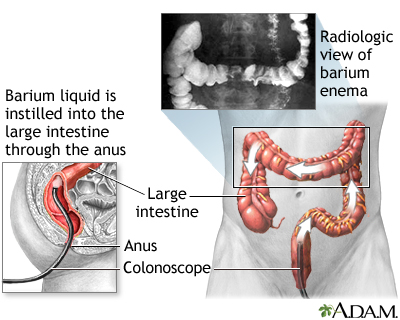
Colorectal CancersIBD increases the risk for colorectal cancer. The risk is highest for people who have had IBD for at least 8 years or who have extensive areas of colon involvement. The more severe the disease, and the more it has spread throughout the colon, the higher the risk. Having a family history of colorectal cancer may also increase risk. People with Crohn disease also have an increased risk for small bowel cancer. (However, small bowel cancer is a very rare type of cancer.) If you have an IBD, discuss with your doctor how often you should have a colonoscopy screening test for colorectal cancer.
Most guidelines recommend that people with IBD receive an initial colonoscopy earlier than people with no risk factors for colon cancer. Schedules for follow-up colonoscopies are based on various risk factors. Some of these risk factors include:
- Severity of Crohn disease
- Family history of colorectal cancer
- Presence of primary sclerosing cholangitis
- Personal history of abnormal biopsies (dysplasia) in the colon
- Presence of colonic strictures
IBD can increase susceptibility to Clostridium difficile, a species of intestinal bacteria that causes severe diarrhea. It is usually acquired in a hospital. However, studies indicate that C difficile infection is increasing among people with IBD including outside of hospital settings. People with ulcerative colitis are at particularly high risk.
Complications outside the Intestine
Bones
Crohn disease, and the corticosteroid drugs used to treat it, can cause osteopenia (low bone density) and osteoporosis (bone loss).
AnemiaAnemia is a lack of red blood cells. Red blood cell count can be affected by factors such as iron and vitamin B12 deficiency. In Crohn disease, bleeding from the intestinal tract and poor absorption of iron can result in iron-deficiency anemia. Crohn disease can also affect proper absorption of vitamins, which can cause vitamin B12 deficiency anemia.
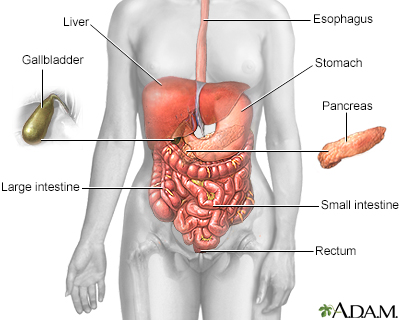
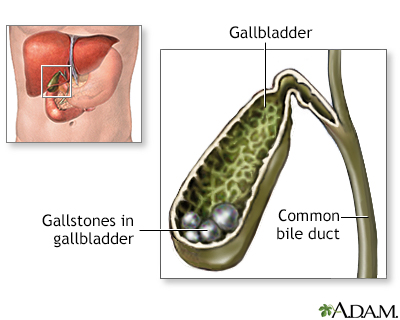
Liver and Gallbladder DisordersIn severe cases, IBD can cause problems with the liver and pancreas and increase the risk for gallstones.
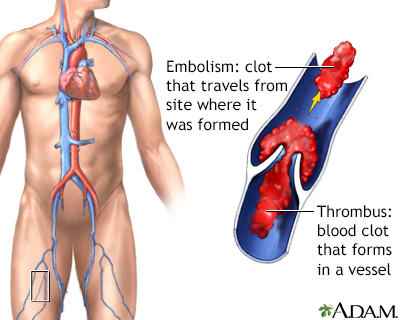
Thromboembolism (Blood Clots)
People with IBD are at a higher risk for blood clots, especially deep venous thromboembolism, where blood clots form in the legs. They are also at risk for pulmonary embolism, when a blood clot travels from the legs to the lungs.
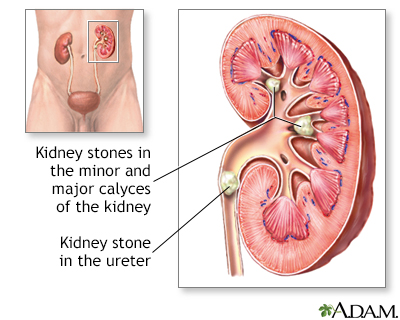
Urinary Tract and Kidney Disorders
IBD may increase the risk for urinary tract and bladder infections, and kidney stones.
Delayed Growth and Development in Children
Up to one half of children with Crohn disease have impaired physical growth and development, and nearly all are underweight.
Emotional FactorsLiving with Crohn disease can pose many emotional challenges. Feelings of frustration, humiliation, and loss of control are common. Although symptoms can be emotionally stressful, and symptom flare-ups are sometimes associated with stressful life events, there is no evidence that stress or psychological factors cause IBD.
Prognosis
The outlook for Crohn disease varies widely. Crohn disease can range from mild (when limited Crohn disease occurs only around the anus) to very severe. Some people may experience only one episode while others have chronic problems.
Most people with Crohn disease experience periodic recurrences of symptoms, but sometimes disease-free periods can last for years or decades. Although Crohn disease cannot be cured, treatments are available that can offer significant help. Many people do eventually require surgery. Crohn disease is rarely a direct cause of death, and most people can live a normal lifespan with this condition.
Diagnosis
There is no definitive diagnostic test for Crohn disease. A health care provider will diagnose Crohn disease based on:
- Medical history and physical examination
- The results of laboratory, endoscopic (appearance and biopsy results), and imaging tests.
Laboratory Tests
Blood and stool tests may be used:
- Blood tests are used for various purposes, including determining the presence of anemia (low red blood cell count). An increased number of white blood cells or elevated levels of inflammatory markers such as C-reactive protein may indicate the presence of inflammation. Low vitamin levels may suggest a problem with properly absorbing food. Antibodies (such as those called pANCA and ASCA) can be used to help distinguish Crohn.
- A stool sample may be taken and examined for blood, infectious organisms, or both. Inflammatory markers measured in stool samples can be used for assessing the disease in patients who have undergone surgery. A stool test called fecal calprotectin can be of help in determining if symptoms are indicative of a flare-up of disease.
Endoscopy
Flexible Sigmoidoscopy and ColonoscopyFlexible sigmoidoscopy and colonoscopy are procedures that involve snaking a fiber-optic tube called an endoscope (videoscope) through the rectum to view the lining of the colon:
Sigmoidoscopy
, which is used to examine only the rectum and left (sigmoid) colon, lasts about 10 minutes and is done without sedation. It may be mildly uncomfortable, but it is not painful.Colonoscopy
allows a view of the entire colon and requires a sedative, but it is still a painless procedure performed on an outpatient basis. A colonoscopy can also help screen for colon cancer.
The doctor can also insert instruments through the endoscope to remove tiny tissue samples (biopsies). A pathologist will view the tissue sample under a microscope to look for signs of inflammation. These procedures can help a doctor to distinguish between ulcerative colitis and Crohn disease, as well as other diseases.
Wireless Capsule EndoscopyWireless capsule endoscopy (WCE) is a newer imaging approach that is sometimes used for diagnosing Crohn disease. With WCE, the person swallows a capsule containing a tiny camera that records and transmits images as it passes through the gastrointestinal tract.
Imaging Procedures
Upper and Lower Gastrointestinal Barium X-RaysAn upper gastrointestinal barium x-ray may be used if Crohn disease is suspected in the small intestine. Swallowed barium passes into the small intestine and shows up on an x-ray image, which may reveal inflammation, ulcers, and other abnormalities. In a barium enema, the x-ray contrast is put into the rectum to show the large intestine.
Other Imaging Tests
Transabdominal ultrasound, magnetic resonance imaging (MRI) and computed tomography (CT) scans may also be used to evaluate the condition of the gastrointestinal tract. Special MRI and CT scans can be used to look at parts of the small intestine that are hard to reach with scopes.
Ruling Out Diseases Resembling Crohn Disease
Ulcerative ColitisBoth Crohn disease and ulcerative colitis cause diarrhea, but it is more often bloody in ulcerative colitis. Abdominal pain may be more constant with Crohn disease than with ulcerative colitis. Fistulas and strictures are common with Crohn disease but very rare with ulcerative colitis. Endoscopy and imaging tests often reveal more extensive involvement through the entire gastrointestinal tract with Crohn disease than with ulcerative colitis. Ulcerative colitis affects only the large intestine (colon) whereas Crohn disease can occur throughout the digestive tract.
Irritable Bowel SyndromeIrritable bowel syndrome (IBS), also known as spastic colon, functional bowel disease, and spastic colitis, may cause some of the same symptoms as inflammatory bowel disease (IBD). Bloating, diarrhea, constipation, and abdominal cramps are all symptoms of IBS. However, IBS is not the same as IBD. In IBS, no pathologic changes are found anywhere in the entire gastrointestinal tract. Behavioral therapy may be helpful in treating IBS. Psychological therapy does not improve IBD, although it can help people cope.
Intestinal infectionsInfections of the gut including infectious colitis, intestinal parasites, and complications of appendicitis may mimic some of the symptoms of Crohn.
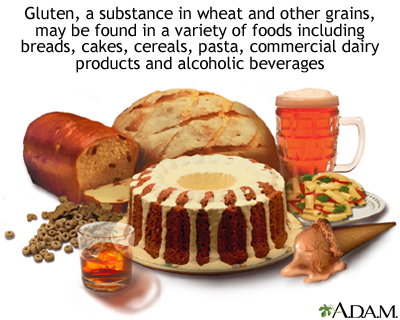
Celiac SprueCeliac sprue, or celiac disease, is intolerance to gluten (a substance found in wheat) that triggers inflammation in the small intestine and causes diarrhea, vitamin deficiencies, and stool abnormalities. It occurs in some people with IBD.
Acute Appendicitis
Crohn disease may cause tenderness in the right lower part of the abdomen, where the appendix is located, that resembles appendicitis.
Cancer
Colon or rectal cancers must always be ruled out when symptoms of IBD occur.
Intestinal Ischemia (Ischemic Colitis)Symptoms similar to IBD can be caused by blockage of blood flow in the intestine. This condition is more likely to occur in older people.
Treatment
Crohn disease is a chronic condition marked by variable periods of no symptoms (remission) and active symptoms (flare-ups). Crohn disease cannot be cured, but appropriate treatment can help suppress the inflammatory response and manage symptoms. A treatment plan for Crohn disease includes:
- Diet and nutrition
- Medications
- Surgery
Diet and Nutrition
Malnutrition is not uncommon in Crohn disease. People with Crohn disease have reduced appetite and may have weight loss. In addition, diarrhea and poor absorption of nutrients can deplete the body of fluid and necessary vitamins and minerals.
It is important to eat a well-balanced healthy diet and focus on getting enough calories, protein, and essential nutrients from a variety of food groups. These include:
- Protein sources such as meat, chicken, fish, or soy
- Dairy products such as milk, yogurt, and cheese (if you are not lactose-intolerant)
- Fruits and vegetables
Depending on your nutritional status, your health care provider may recommend that you take a multivitamin or iron supplement. Sometimes other supplements such as vitamin D, B12, or folate, are needed. It is very important to get enough vitamin D in the diet. If you are lactose intolerant, there are many lactose-free dairy products available. If you are lactose intolerant, make sure that the lactose free products that you eat are enriched with vitamin D.
In cases of severe malnutrition, particularly for children, enteral nutrition may be required. Enteral nutrition uses a feeding tube that is inserted either through the nose and down the throat or directly through the abdominal wall into the gastrointestinal tract. It is the preferred method for feeding people with malnutrition who cannot tolerate eating by mouth. However, enteral nutrition is not likely to help people with malabsorption caused by extensive intestinal disease though it can be effective for helping maintain remission.
Medications
The goals of drug therapy for Crohn disease are to:
- Resolve symptoms (induce remission)
- Prevent disease flare-ups (maintain remission)
Depending on the severity of the condition, different types of drugs are used. The choice of treatment also depends on which areas of the intestinal tract are affected, and the person's age and health status.
The main medications for Crohn disease include:
Aminosalicylates (5-ASAs).
Anti-inflammatory drugs, which may be used to treat mild-to-moderate disease. The standard aminosalicylate used for Crohn disease is sulfasalazine (Azulfidine, generic). Other options are mesalamine (Pentasa, Asacol HD) and balsalazide (Colazal, generic). People with Crohn in the colon may respond better to these drugs than those who have disease in other areas of the GI tract.Corticosteroids.
Used to treat moderate-to-severe disease. Common corticosteroids include prednisone (Deltasone, generic) and budesonide (Entocort). Because corticosteroids can have severe side effects, they are used short-term to induce remission, but not for maintenance therapy.Immunosuppressives
, also called immunomodulators or immune modifiers, block actions in the immune system that are involved with the inflammatory response. Standard immunosuppressives include azathioprine (Imuran, Azasan ), 6-mercaptopurine (6-MP, Purinethol, generic), and methotrexate (Rheumatrex, generic). These drugs may be used for long-term maintenance therapy after people have achieved remission with steroids.Biologic drugs.
A first-line treatment for inducing and maintaining remission in moderate-to-severe disease. They include infliximab (Remicade), adalimumab (Humira), and certolizumab (Cimzia). These drugs target tumor necrosis factor (TNF). Other biologic drugs include natalizumab (Tysabri) and vedolizumab (Entyvio).
Other types of drugs may also be used to treat specific complications and symptoms. Antibiotics, usually ciprofloxacin or metronidazole, can help treat fistulas and abscesses. Anti-diarrheal medications such as loperamide (Imodium) can help control diarrhea, but you should check with your provider first.
Drug therapy for Crohn disease is considered successful if it can push the disease into remission (and keep it there) without causing significant side effects. The condition is considered in remission when the intestinal lining has healed and symptoms such as diarrhea, abdominal cramps, and tenesmus (painful defecation) are normal or close to normal.
Surgery
Many people with Crohn disease eventually need some type of surgery. However, surgery cannot cure Crohn disease. Problems with fistulas and abscesses may occur after surgeries. New disease usually recurs in other areas of the intestine. Surgery may be helpful for relieving symptoms and to correct intestinal blockage, bowel perforation, fistulas, or bleeding.
Basic types of surgery used for Crohn disease include:
Strictureplasty.
Helps open up strictures, narrowed areas of intestine.Resection.
Removes damaged sections of the bowel. The surgeon reattaches the cut ends of the intestine in a procedure called an anastomosis. Repeat resections may be needed if the disease recurs at a different site near the anastomosis.Colectomy
(removal of the colon) orproctocolectomy
(removal of the colon and rectum) may be performed in cases of severe Crohn disease. After a proctocolectomy is completed, the surgeon performs anileostomy
in which the end of the small intestine (ileum) is connected to a small opening in the abdomen (called a stoma). People who have had a proctocolectomy and ileostomy need to wear a pouch over the stoma to collect waste. People who have had a colectomy can continue to pass stool naturally.Other surgical procedures.
Include repairing fistulas that have not been helped by medication, and draining abscesses.
Medications
Aminosalicylates (5-ASAs)
Aminosalicylates contain the compound 5-aminosalicylic acid, or 5-ASA, which helps reduce inflammation. These drugs are sometimes used to prevent relapses and maintain remission in mild-to-moderate Crohn disease. They are used more often to treat ulcerative colitis than Crohn disease.
5-ASA TypesThe standard aminosalicylate drug is sulfasalazine (Azulfidine, generic). This drug combines the 5-ASA drug mesalamine with sulfapyridine, a sulfa antibiotic. The sulfa component of the drug can cause unpleasant side effects, including headache, nausea, and rash.
People who cannot tolerate sulfasalazine, or who are allergic to sulfa drugs, have other options for aminosalicylate drugs, including:
- Mesalamine (Asacol, Pentasa, Apriso, Lialda, generic)
- Olsalazine (Dipentum)
- Balsalazide (Colazal, generic)
These drugs, like sulfasalazine, are available as pills. Mesalamine is also available in enema (Rowasa, generic) and suppository (Canasa) forms.
Side Effects of 5-ASAsCommon side effects of aminosalicylate drugs may include abdominal pain and cramps, diarrhea, gas, headaches, and nausea.
Corticosteroids
Corticosteroids (commonly called steroids) are powerful anti-inflammatory drugs used to treat moderate-to-severe Crohn disease. Because long-term steroid use can cause significant side effects, corticosteroids are used only a short period of time with the goal of inducing remission. Corticosteroids do not prevent flare-ups and are not used for maintenance treatment.
Corticosteroid TypesPrednisone (Deltasone, generic) is the main corticosteroid used for treating Crohn disease. Budesonide (Entocort, Uceris) is a newer type of steroid that is used as an alternative. Prednisone is a systemic steroid, which circulates throughout the body. Budesonide affects only local areas in the intestine so it tends to cause fewer widespread side effects. The choice of which steroid to use depends in part on where in the colon the disease is located.
Prednisone and budesonide are administered as pills, and are sometimes used in combination with the immunosuppressant azathioprine. In very severe cases of Crohn disease, other types of steroids may be used in intravenous or rectal formulations.
Side Effects of CorticosteroidsCommon side effects of short-term treatment with oral steroids can include acne, increased appetite, and insomnia. Long-term treatment with steroids increases the risk for many serious side effects including low bone density (osteoporosis), high blood pressure, and cataracts.
Withdrawing from CorticosteroidsOnce remission is achieved and the intestinal inflammation has subsided, steroids must be withdrawn very gradually. Withdrawal symptoms, including fever, malaise, and joint pain, may occur if the dosage is lowered too rapidly. If this happens, the dosage is increased slightly and maintained until symptoms are gone. More gradual withdrawal is then resumed. To maintain remission, people who are treated with steroids are given an immunomodulator drug (azathioprine, mercaptopurine, or methotrexate) or a biologic (for example, an anti-TNF drug such as infliximab or adalimumab).
Some people cannot stop taking steroids without having a relapse of their symptoms. They may be treated with immunomodulators or biologic drugs, or be candidates for surgery.
Immunosuppressive Drugs (Immunomodulators)
Immunosuppressant drugs, also called immunodulators, suppress or limit actions of the immune system and therefore the inflammatory response that causes Crohn disease. These drugs may be used in combination with an anti-TNF drug to induce remission. They may also be used alone to maintain remission in people who were treated with steroid drugs.
Immunosuppressants allow corticosteroids to be withdrawn while keeping the disease under control. For this reason, immunosuppressants are sometimes referred to as steroid-sparing drugs.
Immunomodulator TypesAzathioprine (Imuran, Azasan, generic) and mercaptopurine (6-MP, Purinethol, generic) are the standard oral immunosuppressant drugs. They belong to a class of medications called thiopurines.
Methotrexate [(MTX), Rheumatrex, generic] is another type of immunosuppressant. It is given as a weekly injection.
Side Effects of ImmunomodulatorsGeneral side effects of immunosuppressants may include nausea, vomiting, susceptibility to infections, and liver or pancreatic inflammation. People who take these drugs should receive frequent blood tests to monitor white blood cell count and liver function.
A serious concern associated with thiopurines is increased risk for lymphoma, a cancer that starts in the immune system. Methotrexate can cause miscarriages and birth defects. Both men and women who take methotrexate should use birth control.
Biologic Drugs
Biologic drugs are genetically engineered to target specific proteins involved with the body's inflammatory response.
Biologic Drug TypesTumor necrosis factor (TNF) blockers, commonly called anti-TNFs, are the main biologic drugs used for treating Crohn disease. The three anti-TNF drugs approved for Crohn disease are infliximab (Remicade), adalimumab (Humira), and certolizumab (Cimzia).
Other types of biologic drugs approved for Crohn disease are natalizumab (Tysabri) and vedolizumab (Entyvio). These drugs are similar to each other and work in a different way than anti-TNF drugs. More recently, ustekinumab (Stelara) has been approved for moderate to severe Crohn disease.
The American Gastroenterological Association recommends an anti-TNF drug as a first-line treatment for inducing and maintaining remission in people with moderate-to-severe Crohn disease. They may be used in combination with a thiopurine drug (azathioprine or mercaptopurine).
AdministrationBiologic drugs are given either as intravenous (IV) injections into the vein or as subcutaneous (under the skin) injections:
- Infliximab is given by IV every 8 weeks
- Adalimumab is given as a subcutaneous injection every other week
- Certolizumab is given as a monthly subcutaneous injection
- Natalizumab is given as a monthly IV
- Vedolizumab is given by IV every 8 weeks
- Ustekinumab is given by IV every 8 to 12 weeks
All of these drugs require more frequent administration during the initial weeks of therapy. Sometimes these drugs need to be given more often to keep the disease under control.
Side Effects of BiologicsBiologic drugs can cause pain and swelling at the injection site. Other common side effects may include upper respiratory infections, headache, rash, stomach and back pain, and nausea. Some people have allergic reactions to these drugs.
These drugs may increase the risk for infections, including tuberculosis and reactivation of hepatitis B. People need to be tested for these infections before starting treatment. Your health care provider should monitor you for any signs of viral, bacterial, or fungal infection. People who take biologic drugs should also receive regular tests for signs of liver problems.
There is a concern that the anti-TNF drugs (infliximab, adalimumab, and certolizumab) may increase the risk for lymphomas and leukemia cancers. However, recent studies have disputed these findings and the benefits of these drugs appear to outweigh the risks for cancer.
Natalizumab may increase the risk for a rare neurological condition called progressive multifocal leukoencephalopathy (PML), which can lead to death or severe disability. The risk for PML increases when patients have more than 24 infusions of natalizumab (2 years of treatment). PML may also be a risk with vedolizumab but it is too early to tell.
Other Medications
AntibioticsAntibiotics may be used as a first-line treatment for mild Crohn disease and for treating:
- Fistulas
- Bacterial overgrowth
- Abscesses
- Infections around the anus and genital areas
Standard antibiotics include ciprofloxacin (Cipro, generic) and metronidazole (Flagyl, generic). Ciprofloxacin is the antibiotic of choice.
Over time, metronidazole can cause peripheral neuropathy, a nerve disorder that can cause numbness and tingling in the hands and feet. Other side effects associated with metronidazole include nausea, vomiting, diarrhea, loss of appetite, dizziness, and headaches.
Although ciprofloxacin causes fewer side effects than metronidazole, it can interact with antacids (Rolaids, Tums) and vitamin and mineral supplements that contain calcium, iron, or zinc. Do not take antacids or vitamin supplements at the same time as the ciprofloxacin dose. You should also avoid sun exposure as ciprofloxacin increases sun sensitivity. Ciprofloxacin may also increase susceptibility to C difficile colitis, an antibiotic-associated bacterial infection that causes severe diarrhea.
Anti-Diarrheal DrugsMild-to-moderate diarrhea may be reduced by daily use of psyllium (Metamucil, generic), though they can worsen symptoms in cases of IBD and should be used cautiously. Standard anti-diarrheal medications include loperamide (Imodium, generic) or a combination of atropine and diphenoxylate (Lomotil, generic).
Surgery
Strictureplasty
The chronic inflammation of Crohn disease can eventually cause scarring, which leads to narrowing in certain segments of the intestine. These narrowed areas are called strictures. If strictures do not respond to medication, a surgical procedure called strictureplasty may be used to open the blockage and widen the narrow passages.
Strictureplasty is usually performed for repairing strictures in the jejunum or ileum sections of the small intestine. It involves cutting open the strictured segment and stitching the tissue crosswise. This helps remove the area obstructing the bowel and enlarges the width of the passageway, without removing any parts of the intestine.
Resection and Anastomosis
When Crohn disease penetrates or severely inflames the bowel or colon, surgical resection may be required. Resection is also performed for people who have signs of small or large bowel perforation. (Perforation is when a hole in the bowel lets waste contents flow into the abdominal cavity.)
Resection involves removing the diseased section of the bowel and then reattaching the healthy ends of the intestine in a procedure called an anastomosis. Resection can be performed either through open surgery involving a wide incision through the abdomen, or through less-invasive laparoscopy.
Disease Recurrence after ResectionAbout one half of people experience a recurrence of active Crohn disease within 5 years of having resection and require a second surgery. The disease usually recurs near the site of the anastomosis. Medications, such as biologics and immunosuppressive drugs, are given to help prevent or delay recurrence.
Colectomy, Proctocolectomy, and Ileostomy
If Crohn disease becomes extremely severe, and other treatments do not help, the entire colon may need to be removed. If the rectum is also affected, it will also need to be removed:
Colectomy
is surgical removal of the entire colonProctocolectomy
is surgical removal of the entire colon and rectum
Proctocolectomy with ileostomy involves the following:
- To perform
proctocolectomy
, the surgeon removes the entire colon, including the lower part of the rectum and the sphincter muscles that control bowel movements. - To perform
ileostomy
, the surgeon makes a small opening in the lower right corner of the abdomen called astoma
. The surgeon then connects cut ends of the small intestine to this opening. An ostomy bag is placed over the opening and accumulates waste matter. It requires emptying several times a day.
Other Surgeries
Surgery may also be performed to treat fistulas or drain abscesses that have not been helped by medication, to control excessive bleeding, and to remove intestinal obstructions.
Lifestyle Changes
Diet and Nutrition
Certain types of foods may worsen diarrhea and gas symptoms, especially during times of active disease. While people vary in their individual sensitivity to foods, general guidelines for dietary management during symptom flare-ups include:
- Eat small amounts of food throughout the day.
- Stay hydrated by drinking lots of water (frequent consumption of small amounts throughout the day).
- Eat soft, bland foods and avoid spicy foods.
- Avoid high-fiber foods (bran, beans, nuts, seeds, and popcorn).
- Avoid fatty greasy or fried foods and sauces (butter, margarine, and heavy cream).
- Limit milk products if you are lactose intolerant (consider taking a lactase supplement to improve tolerance). Otherwise, dairy products are a good source of protein and calcium.
- Avoid or limit alcohol and caffeine consumption.
Dietary Supplements
Your health care provider may recommend you take a multivitamin. Although other types of dietary supplements, such as probiotics ("healthy bacteria," such as lactobacilli) and omega-3 fatty acids, have been investigated for Crohn disease, there is no conclusive evidence that they are effective in controlling symptoms or preventing disease relapses.
Be sure to tell your provider of any herbs or supplements you are taking or considering taking as some of these may be unsafe or interact with medications.
Smoking Cessation
Smoking is bad for everyone but it causes additional specific problems for people with Crohn disease. Smokers who have Crohn disease are at increased risk of developing fistulas and of needing surgery. They are more likely to need stronger immune-suppressing medications than non-smokers. Smoking also makes it more likely that Crohn disease that is in remission will return. For these, and many more reasons, it is very important to quit smoking. Talk with your provider about finding a smoking cessation strategy that works for you.
Stress Management
Stress does not cause Crohn disease or ulcerative colitis, but it can trigger and worsen symptoms. Many people find that stress management techniques help them cope better with living with IBD. Stress management can include:
- Meditation
- Yoga and relaxation response training
- Getting adequate sleep
- Exercising regularly
- Building a healthy support network of family and friends
Some people may also benefit from psychological counseling.
Resources
- Crohn's & Colitis Foundation of America -- www.crohnscolitisfoundation.org
- American Gastroenterological Association -- www.gastro.org
- American College of Gastroenterology -- gi.org
- National Institute of Diabetes and Digestive and Kidney Diseases -- www.niddk.nih.gov
References
Adamina M, Bonovas S, Raine T, et al. ECCO Guidelines on therapeutics in Crohn's disease: surgical treatment. J Crohns Colitis. 2020;14(2):155-168. PMID: 31742338 pubmed.ncbi.nlm.nih.gov/31742338/.
Ananthakrishnan AN, Regueiro MD. Management of inflammatory bowel disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116.
Bye WA, Nguyen TM, Parker CE, Jairath V, East JE. Strategies for detecting colon cancer in patients with inflammatory bowel disease. Cochrane Database Syst Rev. 2017;9:CD000279. PMID: 28922695 pubmed.ncbi.nlm.nih.gov/28922695/.
Chande N, Townsend CM, Parker CE, MacDonald JK. Azathioprine or 6-mercaptopurine for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2016;10:CD000545. PMID: 27783843 pubmed.ncbi.nlm.nih.gov/27783843/.
Cheifetz AS. Management of active Crohn disease. JAMA. 2013;309(20):2150-2158. PMID: 23695484 pubmed.ncbi.nlm.nih.gov/23695484/.
Cushing K, Higgins PDR. Management of Crohn disease: a review. JAMA. 2021;325(1):69-80. PMID: 33399844 pubmed.ncbi.nlm.nih.gov/33399844/.
Farraye FA, Odze RD, Eaden J, et al. AGA medical position statement on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138(2):738-745. PMID: 20141808 pubmed.ncbi.nlm.nih.gov/20141808/.
Feuerstein JD, Ho EY, Shmidt E, et al; American Gastroenterological Association Institute Clinical Guidelines Committee. AGA Clinical Practice Guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn's disease. Gastroenterology. 2021;160(7):2496-2508. PMID: 34051983 pubmed.ncbi.nlm.nih.gov/34051983/.
Kaplan GG, Ng SC. Epidemiology, pathogenesis, and diagnosis of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 115.
Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 132.
Lim WC, Wang Y, MacDonald JK, Hanauer S. Aminosalicylates for induction of remission or response in Crohn's disease. Cochrane Database Syst Rev. 2016;7:CD008870. PMID: 27372735 pubmed.ncbi.nlm.nih.gov/27372735/.
Nguyen GC, Loftus EV Jr, Hirano I, et al; AGA Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on the management of Crohn's disease after surgical resection. Gastroenterology. 2017;152(1):271-275. PMID: 27840074 pubmed.ncbi.nlm.nih.gov/27840074/.
Rezaie A, Kuenzig ME, Benchimol EI, et al. Budesonide for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2015;(6):CD000296. PMID: 26039678 pubmed.ncbi.nlm.nih.gov/26039678/.
Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015;169(11):1053-1060. PMID: 26414706 pubmed.ncbi.nlm.nih.gov/26414706/.
Shouval DS, Rufo PA. The role of environmental factors in the pathogenesis of inflammatory bowel diseases: a review. JAMA Pediatr. 2017;171(10):999-1005. PMID: 28846760 pubmed.ncbi.nlm.nih.gov/28846760/.
Singh S, Proctor D, Scott FI, Falck-Ytter Y, Feuerstein JD. AGA technical review on the medical management of moderate to severe luminal and perianal fistulizing Crohn's disease. Gastroenterology. 2021;160(7):2512-2556.e9. PMID: 34051985 pubmed.ncbi.nlm.nih.gov/34051985/.
Strong S, Steele SR, Boutrous M, et al; Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. Clinical practice guideline for the surgical management of Crohn's disease. Dis Colon Rectum. 2015;58(11):1021-1036. PMID: 26445174 pubmed.ncbi.nlm.nih.gov/26445174/.
Terdiman JP, Gruss CB, Heidelbaugh JJ, Sultan S, Falck-Ytter YT; AGA Institute Clinical Practice and Quality Management Committee. American Gastroenterological Association Institute guideline on the use of thiopurines, methotrexate, and anti-TNF-a biologic drugs for the induction and maintenance of remission in inflammatory Crohn's disease. Gastroenterology. 2013;145(6):1459-1463. PMID: 24267474 pubmed.ncbi.nlm.nih.gov/24267474/.
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet. 2017;389(10080):1741-1755. PMID: 27914655 pubmed.ncbi.nlm.nih.gov/27914655/.
Torres J, Bonovas S, Doherty G, et al. ECCO Guidelines on therapeutics in Crohn's disease: medical treatment. J Crohns Colitis. 2020;14(1):4-22. PMID: 31711158 pubmed.ncbi.nlm.nih.gov/31711158/.
Veauthier B, Hornecker JR. Crohn's Disease: diagnosis and management. Am Fam Physician. 2018;98(11):661-669. PMID: 30485038 pubmed.ncbi.nlm.nih.gov/30485038/.
Review Date: 6/6/2021
Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.