Fibromyalgia - InDepth
Fibromyositis - InDepth; Fibrositis - InDepth; Myofascial pain syndrome - InDepth; FM - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of fibromyalgia.
Highlights
Fibromyalgia is characterized by:
- Widespread musculoskeletal pain
- Fatigue
- Memory and cognitive problems
- Sleep disturbance
- Mood disturbances
Research is pointing to a mechanism of central nervous system hypersensitivity to pain.
Causes
- The exact cause of fibromyalgia is still unknown.
- Conditions earlier in life that cause long lasting pain are associated with the development of fibromyalgia, but no one trigger has been shown to be the primary cause.
- Sociocultural, hormonal, and psychosocial factors may also contribute.
Risk Factors
Potential risk factors include:
- Being female
- Being middle aged or older
- Having systemic lupus erythematosus (lupus) or rheumatoid arthritis
- Family history of chronic pain
- Painful or stressful condition earlier in life
- Psychological stress
- Viral infections
- Poor sleep habits
- Obesity
- Inactivity
Prognosis
- Fibromyalgia can be mild or disabling, and the emotional toll can be substantial.
- Although fibromyalgia is lifelong, it is not fatal.
Pharmacologic Approach
Many on-label and off-label drugs are prescribed to treat fibromyalgia.
Of those, drugs that are centrally-acting, include:
- Tricyclics
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Gabapentinoids and pregabalin
- Cannabinoids
- Selective serotonin reuptake inhibitors (SSRIs).
Non-pharmacologic Approach
Non-pharmacologic therapies that have been shown to benefit fibromyalgia patients include:
- Patient education
- Graded exercise
- Physical therapy
- Cognitive behavioral therapy (CBT)
- Complementary therapies (acupuncture, balneotherapy, yoga, etc.)
Introduction
Description
Fibromyalgia is a condition that causes lasting, and sometimes debilitating muscle pain and fatigue. It is characterized by:
- Widespread musculoskeletal pain
- Fatigue
- Memory and cognitive problems
- Sleep disturbance
- Mood disturbances
- Anxiety
- Depression
- Headache
- Numbness or abnormal sensations
No one knows exactly what causes fibromyalgia. Some research suggests that the central nervous system is hypersensitive to pain. Fibromyalgia often emerges in people who have experienced chronic pain earlier in their life through some other means, such as trauma, injuries, infections, or autoimmune conditions like lupus or rheumatoid arthritis. The long lasting earlier chronic pain is thought to sensitize the central nervous system to pain stimuli, resulting in fibromyalgia.
Symptoms
Pain
The main symptom of fibromyalgia is pain. It can be localized or widespread.
- Localized pain (tender points). Pain starts in the muscles, usually in the neck and shoulders, and then spreads out from these areas. The joints are not affected, although many patients feel like the pain starts in their joints. There are no lumps on the tender points, and no signs of inflammation (swelling.) The skin also feels more sensitive to the touch.
- Widespread pain. Pain described as generalized stiffness, burning, and aching pain. It can also "radiate," or spread, to nearby areas. Most people report feeling some pain all the time, but the intensity of the pain may increase or decrease. Many describe it as "exhausting." The pain can vary with the time of day, changes in the weather, physical activity or inactivity, and stress. The pain is often more intense when sleep is disturbed.
Fatigue and Sleep Disturbances
Fatigue and sleep disturbances are almost universal in patients with fibromyalgia. Restless legs syndrome and periodic limb movement disorder are also common. It is not clear whether fibromyalgia leads to poor sleeping patterns or if the sleep disturbances come first.
Many people complain that they cannot get to sleep or stay asleep, and they feel tired when they wake up. Some report that their fatigue is more distressing than their pain, because it interferes with their ability to enjoy life. Some experts believe that if a person does not have sleep problems, the condition may not be fibromyalgia. Researchers continue to investigate the link between fibromyalgia and sleep.
Mood and Cognition
Many people with fibromyalgia suffer from depression and other mood disturbances. They also report cognitive difficulties, such as memory and concentration problems. These conditions often go undiagnosed.
Other Symptoms
The following symptoms may also occur with fibromyalgia:
- Digestive problems ( irritable bowel syndrome, gas, diarrhea, and constipation)
- Dizziness
- Dry mouth
- Menstrual cramps
- Muscle weakness
- Balance problems
- Nausea
- Heartburn
- Ringing in ears
- Depression
- Nervousness
- Tension or migraine headaches
- Tingling or numbness in the hands and feet
- Urinary problems or bladder spasms
Causes
The exact cause of fibromyalgia is unknown. The hallmark of fibromyalgia is hyperactivity of pain pathways in the central nervous system.
Physical injuries, trauma, viral infections, or other conditions that cause long lasting pain are associated with fibromyalgia, but no one trigger has been shown to be the primary cause of fibromyalgia.
Many experts believe that fibromyalgia is a chronic pain condition brought on by several abnormal body responses to stress.
People with fibromyalgia have decreased activity in opioid receptors in parts of the brain that affect mood and the emotional aspect of pain. This reduced response might explain why fibromyalgia patients are likely to have depression or other mood disorders, and are less responsive to opioid painkillers.
Stress Response Abnormalities
Many hormonal, metabolic, and brain chemical abnormalities have been described in studies of fibromyalgia patients. Changes appear to occur in several brain chemicals, although no regular pattern has emerged that fits most people. Fibromyalgia may be a result of the effects of pain and stress on the central nervous system that lead to changes in the brain, rather than a brain disorder itself.
Serotonin
Of particular interest to researchers is serotonin, an important nervous system chemical messenger found in the brain, gut, and other areas of the body. Serotonin helps create feelings of well-being, adjusts pain levels, and promotes deep sleep. Lower serotonin levels have been noted in some people with fibromyalgia.
Stress Hormones
There is evidence of abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, which controls important functions, including sleep, the stress response, and depression. Changes in the HPA axis appear to produce lower levels of the stress hormones norepinephrine and cortisol. Lower levels of stress hormones lead to impaired responses to psychological or physical stresses.
Factors that may trigger a person's stress response and contribute to the development of fibromyalgia, include:
- Infections (Epstein-Barr virus, Lyme disease)
- Physical trauma (such as a car accident)
- Emotional stress
- Hormonal changes (such as an underactive thyroid gland)
- Medications
Insulin-like growth factor-1 (IGF-1)
IGF-1 is secreted in the liver in response to growth hormone, a pituitary hormone. Some studies have reported low levels of IGF-1 or of growth hormone in some people with fibromyalgia. Growth hormone and IGF-1 promotes bone and muscle growth. Low levels of these hormones may lead to impaired thinking, lack of energy, muscle weakness, and intolerance to cold. Although researchers have not found a causative link between IGF-1 levels and fibromyalgia; IGF-1 levels in the blood may be a marker of the disorder. Additionally, growth hormone is being investigated as therapy for fibromyalgia.
Abnormal Pain Perception and Substance P
Some studies have suggested that people with fibromyalgia may perceive pain differently than healthy people. Fibromyalgia involves hyper-activity in the parts of the central nervous system that process pain (the nociceptive system). Brain scans of people with fibromyalgia have found abnormalities in blood flow and pain processing centers. For example, researchers have detected up to 3 times the normal level of substance P (a chemical messenger associated with increased pain perception) in people with fibromyalgia.
Some people with fibromyalgia may be oversensitive to external stimulation, and overly anxious about the sensation of pain. This increase in awareness is called generalized hypervigilance. People with fibromyalgia have been found to have greater awareness of, or less tolerance for, movement problems (such as tremor) that do not match their expected sensory feedback. This mismatch in sensory signals might enhance the perception of pain. People with fibromyalgia also seem to be more sensitive to sounds.
Immune Abnormalities
Fibromyalgia has symptoms that resemble those of some rheumatic illnesses, including rheumatoid arthritis and lupus (systemic lupus erythematosus). These are autoimmune diseases in which a defective immune system mistakenly attacks the body's own healthy tissue, producing inflammation and damage. The pain in fibromyalgia, however, does not appear to be due to autoimmune factors, and there is little evidence to support a role for an inflammatory response in fibromyalgia.
Psychiatric Disorders
People with fibromyalgia are more likely to also have a psychiatric disorder, such as:
- Depression
- Anxiety
- Obsessive-compulsive disorder
- Post-traumatic stress disorder (PTSD)
While psychological stressors are not the primary causes of fibromyalgia, they may contribute to the condition in 3 ways:
- They could make people more susceptible to fibromyalgia.
- They may play some role in triggering the onset of the condition.
- They may perpetuate the condition.
Studies have reported higher rates of severe emotional and physical abuse in people with fibromyalgia compared with the general population.
PTSD or chronic stress may play a strong role in the development of fibromyalgia in some patients. PTSD is an anxiety disorder triggered by a specific traumatic event. Some evidence indicates that PTSD actually causes changes in the brain, possibly from long-term overexposure to stress hormones.
Risk Factors
General Risk Factors
It is estimated that 3% to 6% of the world's population have fibromyalgia. Some evidence suggests that several factors may make people more susceptible to fibromyalgia. These risk factors include:
- Being female - women are twice as likely to have fibromyalgia as men
- Age - the prevalence of fibromyalgia increases with age
- Family history of chronic pain
- Painful, traumatic, or stressful condition earlier in life
- Psychological stress
- Poor sleep habits
- Obesity
- Inactivity
Fibromyalgia can arise at any age, any ethnic group, and in developing and industrialized countries alike. However, nearly all people with fibromyalgia have experienced multiple periods of other types of chronic pain, often localized, earlier in their life through any one of a number of sources, such as:
- Headaches and migraines
- Menstrual cramps (dysmenorrhea)
- Jaw pain (temporomandibular joint dysfunction)
- Chronic fatigue
- Arthritis
- Irritable bowels
- Painful bladder syndrome
- Endometriosis
- Back or neck pain
Family members of people with fibromyalgia often suffer themselves from some form of chronic pain. First-degree relatives of people with fibromyalgia are more likely to have fibromyalgia themselves. The way a person processes pain may be in part due to genetic factors.
Diagnosis
Diagnostic Criteria
Typically, a person with fibromyalgia presents a degree of pain that cannot be fully explained by inflammation or signs of tissue damage.
It is important to diagnose fibromyalgia as soon as possible, so treatment can be started.
Fibromyalgia criteria can be helpful, particularly if the person does not have another disorder, such as depression or arthritis, which could complicate the diagnosis. Failure to meet the criteria, however, does not rule out fibromyalgia. Fibromyalgia should be suspected in any person who has muscle and joint pain with no identifiable cause.
The American College of Rheumatology (ACR) put forth diagnostic criteria in 1990 and then later updated the criteria in 2010. The main difference is that the old criteria focused on the presence of pain at 18 specific tender points mapped on the body, whereas the new criteria is concerned with the extent of pain anywhere on the body. Another difference is that the new criteria balanced the presence of pain with other symptoms like fatigue, sleep disturbance, cognitive problems, and mood problems.
New Criteria
The ACR's proposed new scoring system that replaced the tender point examination with the summation of the following assessments:
- A widespread pain index (WPI), which counts the number of areas where the patient has felt pain in the last week. WPI accounts for 0 to 19 points.
- A symptom severity scale (SSS), which rates on a scale of 0 to 3 the severity in the last week of 3 common fibromyalgia symptoms: fatigue, unrefreshing sleep, and cognitive symptoms. The three symptoms domains component of the SSS accounts for 0 to 9 points.
- An additional component of the SSS score is the severity of somatic symptoms, including: headaches, irritable bowels, abdominal pain, Raynaud's phenomenon, nausea, chest pain, heartburn, painful urination, insomnia, depression, and others. The somatic symptoms component of the SSS accounts for (0 to 3 points.)
A total score greater than 12 (WPI score greater than 7 and SSS score greater than 5 or WPI score of 3 to 6 and SSS score greater than 9) has been proposed as a cutoff for diagnosis. These symptoms should be present for longer than 3 months and not be explainable by another disorder. However, some view fibromyalgia as a spectrum disorder, where the score simply reflects the severity of the condition.
Medical and Personal History
A doctor should always take a careful personal and family medical history, which includes a psychological profile and history of any factors that might indicate other conditions, such as:
- Infectious diseases
- Muscle weakness
- Physical injuries
- Rashes
- Recent weight change
- Sexual, physical, or substance or alcohol abuse
During this medical history, people should tell their doctor about any drugs they take, including vitamins and over-the-counter or herbal medications.
Physical Examination
The physical exam may not reveal much, other than the tender spots that are included in the diagnostic criteria. These spots must be painful when pressed, not simply tender. For fibromyalgia to be diagnosed, these tender sites should not show signs of inflammation (redness, swelling, or heat in the joints and soft tissue.)
The tender points may change in location and sensitivity over time. A doctor may recheck tender points that do not respond the first time in people who have other fibromyalgia symptoms.
The doctor will also examine the nails, skin, mucus membranes, joints, spine, muscles, and bones to help rule out arthritis, thyroid disease, and other disorders.
Other Tests
No blood, urine, or other laboratory tests can definitively diagnose fibromyalgia. If these tests show abnormal results, the doctor should look for other disorders.
Tests that are done to diagnose or rule out diseases with similar symptoms may include:
- Antibody tests
- Complete blood count
- C-reactive protein
- Erythrocyte sedimentation rate (ESR)
- Thyroid and liver function tests
- Sleep testing
The doctor may suggest follow-up psychological profile testing if laboratory results do not indicate a specific disease.
Conditions with Similar Symptoms
Between 20% and 30% of all rheumatology office visits in the US are due to symptoms that resemble those of fibromyalgia. Because no laboratory test can confirm fibromyalgia, doctors will usually first test for similar conditions.
Getting diagnosed with one of the disorders below may not always rule out fibromyalgia, because several conditions may overlap or coexist with fibromyalgia, and have similar symptoms. Like fibromyalgia, a number of these conditions also cannot easily be diagnosed. It is not clear whether these conditions cause fibromyalgia, are risk factors for the disorder, have causes in common with fibromyalgia, or have no relationship at all with it.
Chronic Fatigue Syndrome
There is a significant overlap between fibromyalgia and chronic fatigue syndrome (CFS.) As with fibromyalgia, the cause of CFS is unknown. A doctor can diagnose either disorder based only on symptoms reported by the patient. The 2 disorders share most of the same symptoms. They are also treated almost identically. The main differences are:
- Pain is the primary symptom in fibromyalgia. While some people with CFS may experience muscle pain, it is typically less prominent.
- Fatigue is the main symptom in CFS. It is severe, is not caused by excessive work or exercise, and is not relieved by rest or sleep.
Myofascial Pain Syndrome
Myofascial pain syndrome can be confused with fibromyalgia. It may also occur with it. Unlike fibromyalgia, myofascial pain occurs in trigger points, as opposed to tender points, and typically there is no widespread, generalized pain. Trigger-point pain occurs in tight muscles, and when the doctor presses on these points, the person may experience a muscle twitch. Unlike tender points, trigger points are often small lumps, about the size of a pencil eraser.
Major Depression
The link between psychological disorders and fibromyalgia is very strong with best estimated concurrence of 40%. Studies report that fibromyalgia patients have a 90% lifetime prevalence of depression, and 62% to 86% prevalence of major depression.
People who have both a psychological disorders and fibromyalgia may be more likely to seek medical help, compared with people who simply have symptoms of fibromyalgia.
Depressed feelings in people with fibromyalgia can be normal responses to the pain and fatigue caused by this syndrome. Such emotions are temporary and related to the condition. They are not considered to be a depression disorder. Unlike ordinary periods of sadness, an episode of major depression can last for many months.
Symptoms of major depression include the following:
- Depressed mood every day
- Feeling worthless or inappropriately guilty
- Inability to concentrate or make decisions
- Insomnia or excessive sleeping
- Low energy every day
- Restlessness or a sense of being slowed down
- Significant weight gain or loss (5% or more of a person's typical body weight in a month)
- Suicidal thoughts
If several of the above symptoms are present, and none of the physical symptoms (particularly the tender points) of fibromyalgia exist, the condition is most likely major depression.
Suicidal thoughts and behaviors are more often encountered in fibromyalgia patients than in the general population.
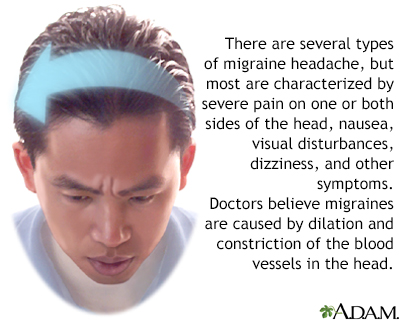
Chronic Headache
Chronic primary headaches, such as migraines, are common in people with fibromyalgia. Some experts believe that migraine headaches and fibromyalgia both involve abnormalities in brain chemistry regulation, including that of serotonin and epinephrine (adrenaline.) Low levels of magnesium have also been noted in patients with both fibromyalgia and migraines. Chronic migraine sufferers who do not benefit from usual therapies may also have fibromyalgia.
Symptoms of a migraine attack may include heightened sensitivity to light and sound, nausea, vision problems (auras), speech difficulty, and intense pain that is mainly on one side of the head.
Multiple Chemical Sensitivity
Multiple chemical sensitivity (MCS) is a term for conditions in which symptoms are attributed to certain chemicals as the cause. Symptoms can be similar to CFS or fibromyalgia. Because everyone is exposed to many chemicals on a daily basis, it is very difficult to determine whether chemicals are responsible for specific symptoms.
Restless Legs Syndrome
People with fibromyalgia are more prone to have restless legs syndrome (RLS.) RLS is an unsettling and poorly understood movement disorder that is sometimes described as a sense of unease and weariness in the lower leg that is aggravated by rest and relieved by movement.
Lyme Disease
Lyme disease is a bacterial disease transmitted by ticks. Health care providers can usually diagnose Lyme disease correctly using blood tests that identify antibodies directed at the bacteria that cause it. But if this infection is not diagnosed correctly, it may be mistaken for fibromyalgia. If people with fibromyalgia are incorrectly diagnosed and treated for Lyme disease with long courses of antibiotics, the drugs may have serious side effects.
Drugs and Alcohol
Fatigue is a side effect of many prescription and over-the-counter medications, such as antihistamines. Constant fatigue is also a symptom of drug and alcohol dependency or abuse. Providers should consider medications as a possible cause of fatigue if a person has recently started, stopped, or changed medications. Withdrawal from caffeine can also produce depression, fatigue, and headaches.
Polymyalgia Rheumatica
Polymyalgia rheumatica is a condition that causes pain and stiffness. It generally occurs in older people. Tender points are also present with this disorder, although they almost always occur in the hip and shoulder area. Morning stiffness is common, and people may also experience fever, weight loss, and fatigue. It is important to diagnose polymyalgia rheumatica early with an ESR blood test, because some people with polymyalgia rheumatica have a related condition (giant cell arteritis) that may lead to blindness if not treated. Polymyalgia rheumatica usually responds to low doses of a steroid medication such as prednisone.
Other Conditions
Certain pain-related conditions are also common in people with fibromyalgia, and have overlapping symptoms. Some experts believe these disorders interact so often that they may all be part of one general condition. Examples are:
- Rheumatoid Arthritis. People with this condition experience chronic pain and stiffness. The man difference with fibromyalgia is that the pain in rheumatoid arthritis is localized primarily to the joints, which become inflamed and swollen.
- Irritable bowel syndrome (IBS). More than half of people with fibromyalgia also have IBS, a gastrointestinal disorder that causes cramping, abdominal pain, bloating, constipation, and diarrhea.
- Temporomandibular joint dysfunction. This condition affects the muscles of the face and jaw, leading to pain in those areas. Most people with fibromyalgia experience face and jaw pain.
- Chemicals and environmental toxins. Exposure to various chemicals and environmental toxins such as solvents, pesticides, or heavy metals (cadmium, mercury, or lead) can cause fatigue, chronic pain, and other symptoms of fibromyalgia.
Prognosis
From Mild to Disabling
Fibromyalgia can be mild or disabling, and the emotional toll can be substantial. People with fibromyalgia experience greater psychological distress and a greater impact on quality of life than those with other conditions, such as chronic low back pain.
About half of all people have difficulty with routine daily activities, or are unable to perform them. People with either CFS or fibromyalgia are more likely to lose their jobs, possessions, and support from friends and family than are people suffering from other conditions that cause fatigue.
The pain, emotional consequences, and sleep disturbances that come with fibromyalgia may lead to self-medication and overuse of sleeping pills, alcohol, drugs, or caffeine.
Long-term Outlook
Outlook in Adults
Although fibromyalgia is lifelong, it is not fatal. Some studies show that fibromyalgia symptoms remain stable over the long term, while others report that more than a quarter of patients see improvements in their pain symptoms over time. Regular exercise improves the outlook. People with a significant life crisis or who are on disability have a poorer outcome based on their:
- Ability to work
- Depression
- Disturbed sleep
- Fatigue
- Feelings about their condition
- Pain
Outlook in Children
Children with fibromyalgia tend to have a better outlook than adults with the disorder. Several studies have reported that more than half of children with fibromyalgia recover in 2 to 3 years.
Treatment
An Integrated Approach
Treatment usually involves not only relieving symptoms, but also changing people's attitudes about their disease, and teaching them behaviors that help them cope.
Because fibromyalgia involves hyperactivity of the central nervous system, treatments that target the peripheral nervous systems (such as opioids, corticosteroids, non-steroidal anti-inflammatory drugs, and surgery) are not as effective. Drugs that are centrally acting are more likely to provide relief, and include:
- Tricyclics
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Gabapentinoids and pregabalin
- Selective serotonin reuptake inhibitors (SSRIs)
Many people with fibromyalgia are treated first with medication; however, a combination of non-pharmacologic therapies sometimes appears to work just as well as drug therapy for improving pain, depression, and disability. These therapies include: patient education, graded exercise, cognitive behavioral therapy (CBT), and complementary therapies (acupuncture, balneotherapy, yoga, etc.)
Treatments usually involve trial and error:
- People may start with physical therapy, exercise, stress reduction techniques, and cognitive-behavioral therapy.
- If these methods fail to improve symptoms, an antidepressant or muscle relaxant may be added to the treatment. Doctors usually prescribe these drugs to improve pain tolerance.
- Patient education and programs that encourage coping skills are an important part of any treatment plan.
Preparation for Treatment
People must have realistic expectations about the long-term outlook of their condition, and their own abilities. It is important to understand that fibromyalgia can be managed, and people can live a full life with the disorder.
The definition of improvement is personal. For example, some people are pleased with only a 10% reduction in pain and other symptoms.
The following tips may be helpful when starting a fibromyalgia treatment program:
- The goal of therapy is to relieve symptoms, not cure them.
- Treatment must be tailored to each patient, and a combination approach is often needed.
- People must begin all treatments with the attitude that they are trial-and-error. No single treatment will necessarily relieve all symptoms.
- Treatments are long-lasting, in some cases lifelong, and patients should not be discouraged by the return of symptoms (relapses.)
- Enlisting family members, partners, and close friends, particularly to help with exercise and stretching programs, can be helpful.
- Joining a fibromyalgia support group also helps many people. Support groups may also help their family members, particularly the parents of children with fibromyalgia.
Treatment for Children
Experts say the treatment of fibromyalgia in children should begin with non-drug therapies, including exercise and CBT. While some medications are recommended for adults, most have not been well tested in children yet. No treatments are approved by the FDA for fibromyalgia in pediatric patients. Analgesics and NSAIDs are not very effective in children. Psychological therapies may help control pain in children, although there is no evidence that they improve disability or mood.
Pharmacologic Therapies
On-label and Off-label Options
There is no consensus over which treatment is most useful, or whether a combination of treatments works best. People may receive drug treatments in combination with exercise, patient education, and behavioral therapies.
Pregabalin (Lyrica), duloxetine (Cymbalta), and milnacipran (Savella) are FDA approved for treating fibromyalgia. However, many other drugs, including antidepressants, sleeping aids, pain relievers, and muscle relaxants, are also used off-label to treat the condition. The goal with medication is to improve sleep and pain tolerance.
The main classes of antidepressants used for treating fibromyalgia are tricyclics, SSRIs, and SNRIs. Although these drugs are antidepressants, doctors sometimes prescribe them to improve sleep and relieve pain in non-depressed patients with fibromyalgia. The dosages used for managing fibromyalgia are generally lower than dosages prescribed for treating depression. If a person has depression in addition to fibromyalgia, higher doses may be required.
Tricyclics
Tricyclic antidepressants were the first drugs to be well-studied for fibromyalgia. Tricyclics cause drowsiness and can be helpful for improving sleep. They are also effective for reducing pain, and improving depressed mood and quality of life. The tricyclic drug most commonly used for fibromyalgia is amitriptyline (Elavil, Endep). Other tricyclics include nortriptyline (Pamelor, Aventyl), desipramine (Norpramin), doxepin (Sinequan), imipramine (Tofranil), and amoxapine (Asendin.)
Generally, only small doses of tricyclic antidepressants are needed to relieve fibromyalgia. Therefore, although tricyclics have several side effects, these side effects may be less frequent in people with fibromyalgia than in people who are taking tricyclics for depression. The side effects most often reported include:
- Blurred vision
- Difficulty urinating
- Dizziness
- Drowsiness
- Dry mouth
- Heart rhythm disturbances
- Sexual dysfunction
- Weight gain
As a general rule with medications, tricyclic antidepressants must be taken as directed. An overdose can be life threatening.
Unfortunately, not all people respond to tricyclics, and the effects wear off in some people, sometimes after only a month.
Muscle Relaxants
Cyclobenzaprine (Flexeril) relaxes muscle spasms in specific locations without affecting overall muscle function. It helps relieve fibromyalgia symptoms. Cyclobenzaprine is related to the tricyclic antidepressants and has similar side effects, including drowsiness, dry mouth, and dizziness.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs act directly on 2 chemical messengers in the brain; norepinephrine and serotonin. These drugs appear to have more consistent benefits for fibromyalgia pain than SSRIs. They also tend to have fewer side effects than the tricyclics and are well tolerated.
SNRIs include:
- Duloxetine (Cymbalta) has been approved by the FDA for treating fibromyalgia and can reduce pain by around one-third. The most common side effects are nausea, dry mouth, constipation, decreased appetite, sleepiness, increased sweating, and agitation. Drug interactions are possible. Talk to your provider before taking NSAIDs, aspirin, or blood thinners.
- Milnacipran (Savella) can also improve pain and physical function in people with fibromyalgia. Milnacipran is also FDA-approved for fibromyalgia, however it is not approved for use in children. The label includes a boxed warning that it may increase the risk of suicidal thoughts and behaviors in children and adolescents.
- Venlafaxine (Effexor) is similar to fluoxetine (Prozac) in effectiveness and tolerability. Venlafaxine may impair sexual function and has been shown to be safe and effective in most people. Reported problems with blood pressure and heart rhythm may cause serious problems in elderly patients. Some people also report severe withdrawal symptoms, including dizziness and nausea.
Anti-seizure Drugs
Pregabalin is an anti-seizure drug that works through the chemical messenger gamma aminobutyric acid (GABA), which helps prevent nerve cells from over-firing. Pregabalin was approved by the FDA for treatment of fibromyalgia.
There is evidence that pregabalin may improve sleep quality, fatigue symptoms, and fibromyalgia pain. The most common side effects include mild-to-moderate dizziness, sleepiness, and impaired motor function and concentration. People should talk to their provider about whether pregabalin may affect their ability to drive.
Another anti-epileptic, gabapentin (Neurontin) relieves pain in some people with fibromyalgia. People have reported sleeping better and feeling less tired after taking this drug. However, gabapentin can cause side effects such as dizziness, sleepiness, and swelling.
Selective Serotonin-Reuptake Inhibitors (SSRIs)
SSRIs increase serotonin levels in the brain, which may have specific benefits for fibromyalgia patients. Commonly prescribed SSRIs include fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), and fluvoxamine (Luvox.) They may improve sleep, fatigue, and well-being in many people, but their role in improving pain is not certain. SSRIs should be taken in the morning, since they may cause insomnia. Common side effects are agitation, nausea, and sexual problems, including a delay or loss of orgasm and low sex drive.
Gamma-hydroxybutyrate (GHB)
GHB is the active ingredient of sodium oxybate (Xyrem), a drug usually prescribe for serious sleep disorders. It has been show in some studies to be helpful for patients with fibromyalgia; however, due to the risk of potentially fatal respiratory depression, the FDA did not approve it as a treatment for fibromyalgia.
Non-pharmacologic Therapies
Physical Activity
Many studies have shown that exercise is the most effective part of managing fibromyalgia, and people should expect to take part in a long-term exercise program. Physical activity prevents muscle wasting, increases emotional well-being, and, over time, reduces fatigue and pain.
Exercise programs for fibromyalgia often combine aerobic, strength training, and flexibility exercises with self-education. Benefits can last for up to 9 months after the exercise program ends.
Graded Exercise
The basic approach used for fibromyalgia is called graded exercise. Graded exercise means slowly increasing the amount of physical activity.
In general, graded exercise involves:
- A very gradual program of activity, beginning with mild exercise and building in intensity over time.
- Stretching exercises before working out. A daily stretching routine can help relax tense muscles and prevent soreness.
- Walking, swimming, and using equipment such as treadmills or stationary bikes. Swimming and water therapy are good because they do not require putting weight on the joints.
Adding CBT to a program of graded exercise may also help people with fibromyalgia feel better.
It is important to start an exercise program slowly. People who try difficult exercises too early actually experience an increase in pain, and are likely to become discouraged and quit. Every person must be prepared for relapses and setbacks, and should not get discouraged. People who do not respond to one type of exercise might consider experimenting with another form.
Bursts of Exercise
Exercise can help relieve fibromyalgia, but many people with the condition find it hard to exercise for long periods of time. Adding small amounts of everyday physical activity like taking the stairs, gardening, and walking helps people with fibromyalgia increase their daily exercise amount, and improves their pain and fatigue. As people improve, they can increase their activity level gradually.
Physical Therapy
Physical therapy can also be very helpful. Studies suggest that physical therapy may reduce muscle overload and fatigue, and strengthen weak muscles.
Tai Chi
The ancient Chinese exercise program that combines slow movement, breathing, and meditation may also help people with fibromyalgia. Tai chi improves pain, fatigue, physical functioning, sleeplessness, and depression, and it does not have any side effects.
Improving Sleep Habits
Sleep is essential, particularly because sleep disruptions worsen pain. Many people with fibromyalgia have trouble getting a restful and healing night's sleep. Those who are consistently unable to sleep have little improvement in symptoms. Swing shift work, for example, is extremely hard on people with fibromyalgia. Poor sleep habits can add to sleep problems. Tips for good sleep habits include:
- Avoid caffeine or alcohol 4 to 6 hours before bedtime.
- Avoid drinking fluids right before bedtime so that you do not have to wake up to urinate.
- Avoid exercising 6 hours before bedtime.
- Avoid large meals before bedtime. A light snack, however, may help you sleep.
- Avoid naps, especially in the evening or late afternoon.
- Establish a regular time for going to bed and getting up in the morning. Maintain this schedule even on weekends and during vacations.
- If you are unable to fall asleep after 15 or 20 minutes, go into another room and start a quiet activity. Return to bed when you feel sleepy.
- Minimize light and maintain a comfortable, moderate temperature in the bedroom. Keep the bedroom well ventilated.
- Use the bed only for sleep and sexual relations.
[For more information see In-Depth Report #27 -- Insomnia.]
Insomnia
An in-depth report on the causes, diagnosis, treatment, and prevention of insomnia.
| Read Article Now | Book Mark Article |
Stress Reduction Techniques
Relaxation and stress-reduction techniques are proving helpful for managing chronic pain. Evidence shows that people with fibromyalgia have a more stressful response to daily conflicts and encounters than those without the disorder. Several relaxation and stress-reduction techniques may be helpful for managing chronic pain, including:
- Biofeedback
- Deep breathing exercises
- Hypnosis
- Massage therapy
- Meditation
- Muscle relaxation techniques
Biofeedback
During a biofeedback session, electric leads are taped to a person's head. The person is encouraged to relax using any method that works. Brain waves are measured and an audio signal sounds when alpha waves are detected. Alpha waves are brain waves that occur with a state of deep relaxation. By repeating the process, people using biofeedback connect the sound with the relaxed state and learn to relax on their own. Evidence from studies does not suggest that biofeedback techniques are very helpful for fibromyalgia patients.
Meditation
Meditation, which has been used for many years in Eastern cultures, is an effective relaxation technique. A number of studies are reporting its benefits for fibromyalgia patients who practice on a regular basis.
Meditation can provide the following physical benefits:
- Reduced heart rate, blood pressure, adrenaline levels, and skin temperature
- Improved well-being
- Better sleep. Melatonin helps regulate the sleep-wake cycle.
- Less pain, possibly from reductions in levels of cortisol, a stress hormone
Massage Therapy
Massage therapy is thought to slow the heart rate and relax the body. In one study, people who were given 30-minute massage sessions twice a week had lower stress and anxiety and less pain after 5 weeks compared to a group receiving an alternative therapy called transcutaneous electrical stimulation.
Complementary Medicine and Fibromyalgia
Because of the difficulties in treating fibromyalgia, many people seek alternative therapies. Although some studies have reported a benefit from these treatments, there is not enough evidence to recommend them.
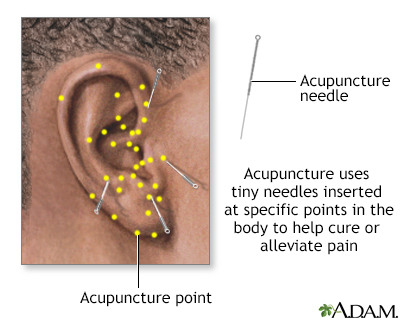
Acupuncture
Studies continue to report conflicting results on acupuncture's ability to relieve pain. Several small studies suggest that it offers some benefit, especially to people who cannot take medicines because of side effects. Other studies have not found enough evidence to support the use of acupuncture for fibromyalgia.
Chiropractic or Osteopathic Manipulation
Chiropractic or osteopathic manipulation are also used by some patients. Osteopathic techniques may include manipulation of the spine or muscle tissue release. While some small studies have reported pain relief and improved sleep with osteopathic manipulation, larger and better designed studies are needed to clearly identify whether this is an effective treatment. There is always a risk for side effects from any of these techniques.
Some alternative remedies are being investigated for fibromyalgia, but none have proved effective so far. Examples include: melatonin, a natural hormone associated with the sleep-wake cycle; and S-adenosylmethionine (SAMe), a natural substance that has antidepressant, anti-inflammatory, and pain relieving properties. Studies have suggested benefits for some people with fibromyalgia, but trials done so far have not been well designed.
Generally, manufacturers of herbal remedies and dietary supplements do not need approval from the FDA to sell their products. It is extremely important for people to realize that any herbal remedy or natural medicine that has positive effects most likely has negative side effects and toxic reactions, just like any conventional drug. There have been a number of reported cases of serious and even deadly side effects from herbal products.
Consult a doctor before using any herbal products or dietary supplements. Also discuss with your doctor the potential interactions between the supplements and any medications you take.
Cognitive Behavioral Therapy
Cognitive-behavioral therapy (CBT) is an effective way to help patients deal with chronic pain and stressful situations. Although the effects of CBT and other non-medication treatments for fibromyalgia do not always last over the long-term, evidence suggests that CBT can help some patients with fibromyalgia, particularly those with a high level of psychological stress.
CBT may be particularly useful for addressing insomnia, one of the hallmark symptoms of fibromyalgia. In studies, people who received CBT for insomnia woke up less often at night, had fewer symptoms of insomnia, and had an improved mood.
The Goals of CBT
The primary goals of CBT are to change mistaken ideas and self-defeating behaviors. People learn to think of pain as something other than a negative factor that controls their life. Over time, the idea that they are helpless goes away and they learn that they can manage the pain.
CBT is particularly helpful for defining and setting limits, which is extremely important for people with fibromyalgia, who often push themselves too far. People learn to prioritize their responsibilities and drop some of the less important tasks or delegate them to others. Learning these coping skills can eventually lead to a more manageable life. People also learn to view themselves and others with a more flexible attitude.
How CBT Works
CBT usually consists of 6 to 20 one-hour sessions. People also receive homework, which usually includes keeping a diary and trying tasks they have avoided in the past because of negative attitudes.
A typical CBT program may involve the following measures:
- Keeping a Diary. People are usually asked to keep a diary. The diary serves as a guide for setting limits and planning activities. People use the diary to track any stress, such as a job or relationship that may be worsening their pain.
- Confronting Negative or Discouraging Thoughts. People are taught to challenge and reverse negative beliefs. For example, "I am not good enough to control this disease, so I am a total failure" becomes the coping statement, "I can learn to control this disease."
- Setting Limits. Limits are designed to keep both mental and physical stress within manageable levels, so that people do not get in over their heads and become discouraged. For example, tasks are broken down into incremental steps, and people focus on doing one step at a time.
- Seeking out Pleasurable Activities. People list a number of enjoyable low-energy activities that they can conveniently schedule.
- Prioritizing. People learn to drop some of the less critical tasks or delegate them to others.
People should learn to accept that relapses occur, and that pushing to accomplish too much too soon can often cause a relapse. People should respect these relapses and back off, and not consider them a sign of failure.
Research also shows that patient education can be effective in treating fibromyalgia, especially when combined with CBT, exercise, and other therapies. Educational programs can take the form of group discussions, lectures, or printed materials.
Support Groups
Cognitive therapy may be expensive and often is not covered by insurance. Other effective approaches that are free or less costly include support groups or group psychotherapy. The success of these programs varies based on the skill of the therapist.
Resources
- American College of Rheumatology -- rheumatology.org/
- National Institute of Arthritis and Musculoskeletal and Skin Diseases -- www.niams.nih.gov
- Arthritis Foundation -- arthritis.org
- National Fibromyalgia Association -- www.fmaware.org/
- Fibromyalgia Network -- fmnetnews.iraherman.com
- American Association of Medical Acupuncture -- www.medicalacupuncture.org
References
American College of Rheumatology. Fibromyalgia. rheumatology.org/patients/fibromyalgia. Updated February 2023. Accessed October 9, 2023.
Arnold LM, Bennett RM, Crofford LJ, et al. AAPT diagnostic criteria for fibromyalgia. J Pain. 2019;20(6):611-628. PMID: 30453109 www.ncbi.nlm.nih.gov/pubmed/30453109.
Berman B, Lewith G, Witt CM, D’Adamo C. Complementary and alternative medicine. In: Hochberg MC, Gravallese EM, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, eds. Rheumatology. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 58.
Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311(15):1547-1555. PMID: 24737367 www.ncbi.nlm.nih.gov/pubmed/24737367.
Clauw DJ. Fibromyalgia and chronic fatigue syndrome. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 258.
Comeau D, Corey D. Rheumatology and musculoskeletal problems. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Elsevier Saunders; 2016:chap 32.
Cooper TE, Derry S, Wiffen PJ, Moore RA. Gabapentin for fibromyalgia pain in adults. Cochrane Database Syst Rev. 2017;1:CD012188. PMID: 28045473 www.ncbi.nlm.nih.gov/pubmed/28045473.
Cording M, Derry S, Phillips T, Moore RA, Wiffen PJ. Milnacipran for pain in fibromyalgia in adults. Cochrane Database Syst Rev. 2015;(10):CD008244. PMID: 26482422 www.ncbi.nlm.nih.gov/pubmed/26482422.
Goldenberg DL, Clauw DJ, Palmer RE, Clair AG. Opioid use in fibromyalgia: a cautionary tale. Mayo Clin Proc. 2016;91(5):640-648. PMID: 26975749 www.ncbi.nlm.nih.gov/pubmed/26975749.
Gmuca S, Sherry DD. Fibromyalgia: treating pain in the juvenile patient. Paediatr Drugs. 2017;19(4):325-338. PMID: 28536810 www.ncbi.nlm.nih.gov/pubmed/28536810.
Kia S, Choy E. Update on treatment guideline in fibromyalgia syndrome with focus on pharmacology. Biomedicines. 2017;5(2). pii: E20. PMID: 28536363 www.ncbi.nlm.nih.gov/pubmed/28536363.
McBeth J, Prescott G, Scotland G, et al. Cognitive behavior therapy, exercise, or both for treating chronic widespread pain. Arch Intern Med. 2012;172(1):48-57. PMID: 22082706 www.ncbi.nlm.nih.gov/pubmed/22082706.
Russell IJ. Fibromyalgia syndrome and myofascial pain syndrome. In: McMahon SB, Koltzenburg M, Tracey I, Turk DC, eds. Wall and Melzack’s Textbook of Pain. 6th ed. Philadelphia, PA: Elsevier Saunders; 2013:chap 48.
Walitt B, Klose P, Fitzcharles MA, Phillips T, Häuser W. Cannabinoids for fibromyalgia. Cochrane Database Syst Rev. 2016;7:CD011694. PMID: 27428009 www.ncbi.nlm.nih.gov/pubmed/27428009.
Walitt B, Urrútia G, Nishishinya MB, Cantrell SE, Häuser W. Selective serotonin reuptake inhibitors for fibromyalgia syndrome. Cochrane Database Syst Rev. 2015;(6):CD011735. PMID: 26046493 www.ncbi.nlm.nih.gov/pubmed/26046493.
Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319-329. PMID: 27916278 www.ncbi.nlm.nih.gov/pubmed/27916278.
Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62(5):600-610. PMID: 20461783 www.ncbi.nlm.nih.gov/pubmed/20461783.
Review Date: 12/16/2019
Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 10/09/2023.