Osteoarthritis - InDepth
Hypertrophic osteoarthritis - InDepth; Osteoarthrosis - InDepth; Degenerative joint disease - InDepth; DJD - InDepth; OA - InDepth; Arthritis - osteoarthritis - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of the most common form of arthritis.
Highlights
Osteoarthritis
Osteoarthritis is a degenerative joint disease that typically affects joints in the knees, hip, hand, feet, and spine. It is the most common form of arthritis. Patients with osteoarthritis experience pain, stiffness, and limited mobility of the affected joint.
Risk Factors
- Older age. Osteoarthritis usually occurs in older adults.
- Women. Osteoarthritis occurs more often in women than in men (although among those younger than age 45, men are affected more often than women).
- Obesity. Being overweight increases the risk of developing osteoarthritis.
- Joint injuries. Sports injuries, fractures involving joints, or occupational repetitive stress can lead to osteoarthritis.
Symptoms
Symptoms of osteoarthritis begin gradually and worsen slowly over time. Osteoarthritis pain is generally described as:
- A sensation of aching or stiffness
- Pain is worsening during activity and improving with rest
- Occurring intermittently
- Causing a grating sensation when the joint is moved
Diagnosis
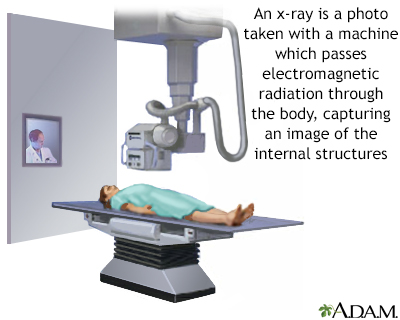
Osteoarthritis is usually diagnosed based on a physical exam and the results of x-rays. In some cases, the doctor may take a sample of synovial fluid from the joint.
Treatment
There is no cure for osteoarthritis, but treatment can reduce pain and improve joint movement and quality of life. Treatment options include:
- Lifestyle modifications and non-drug approaches such as exercise, weight loss, and physical therapy
- Braces to improve stability or realignment of the limb to offload the osteoarthritis
- Medications, including acetaminophen, NSAIDs. or corticosteroid injections
- Surgery, which may be considered for severe osteoarthritis that is not helped by other treatments
Newer Drugs Being Studied
Tanezumab is a monoclonal antibody agent being studied. It targets a protein called nerve growth factor, a substance that regulates pain. Studies are currently being done to evaluate the safety and efficacy of this drug in the treatment of osteoarthritic pain.
Introduction
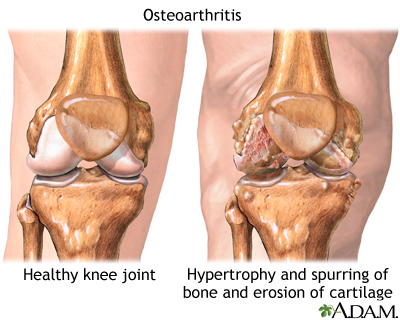
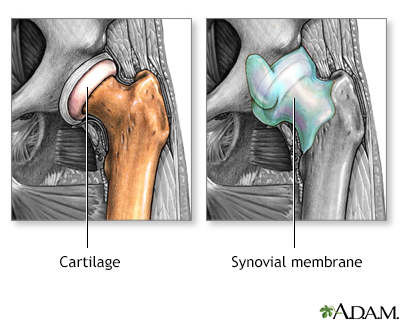
Osteoarthritis, also known as degenerative joint disease, is the most common form of arthritis. In osteoarthritis, joints progressively lose cartilage, the slippery material that cushions the ends of bones.
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from "wear and tear" on a joint. Joints appear swollen, are stiff and painful, and usually feel worse with increased use throughout the day.
As a result, the bone beneath the cartilage is seeing a higher load. The joint edge develops bony overgrowth. The tissue that lines the joint can become inflamed, the ligaments can loosen, and the muscles around the joint can weaken. The person feels pain and has limited movement when using the joint.
Joints
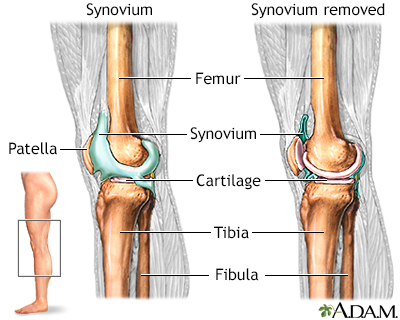
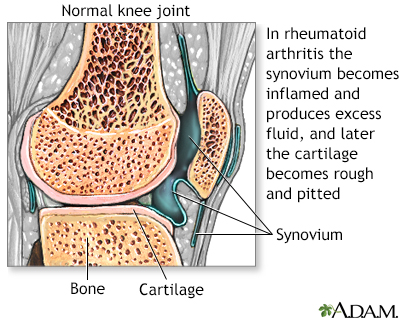
Joints provide flexibility, support, stability, and protection. Specific parts of the joint, the synovium and cartilage, provide these functions.
Synovium
The synovium is a thin membrane lining in the inside of the capsule around a joint. Synovial fluid is a lubricating fluid that supplies nutrients and oxygen to cartilage.
Cartilage
The cartilage is a soft, smooth, and slippery tissue that coats the ends of the bones. The function of the cartilage is to protect the bone and allow for a low friction gliding movement of the bones during joint movement. Cartilage is composed of 4 components:
- Water is the main component of cartilage. The water content of cartilage decreases with age. About 85% of cartilage is water in young people. Cartilage in older people is about 70% water.
- Chondrocytes are the basic cartilage cells that are critical for joint health.
- Proteoglycans are large molecules that bond to water and help keep large amounts of water in cartilage.
- Collagen, an essential protein in cartilage, forms a mesh to give the joint support and flexibility. Collagen is the main protein found in all connective tissues of the body, including the muscles, ligaments, and tendons.
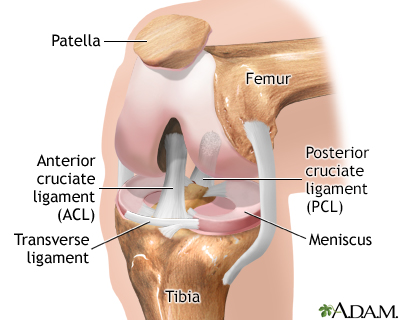
The combination of collagen and water forms a strong and slippery pad in the joint. This pad (meniscus) cushions the ends of the bones in the joint during muscle movement.
Osteoarthritis: The Disease Process
Osteoarthritis develops when cartilage in a joint deteriorates or gets worn away. The process is usually slow:
- In the early stages of the disease, the surface of the cartilage becomes inflamed and swollen. The joint loses proteoglycan molecules and other tissues, which reduces the water content. Cracks (fissures) and pits appear in the cartilage.
- As the disease progresses and more tissue is lost, the cartilage hardens. As a result, it becomes increasingly vulnerable to damage from repetitive use and injury. The initial cartilage swelling slowly progresses to roughening and surface shredding.
- Eventually, large amounts of cartilage are destroyed, leaving the ends of the bone within the joint unprotected.
As the body tries to repair damage to the cartilage, other problems can develop:
- Clusters of damaged cells or fluid-filled cysts may form around the bony areas or near the fissures in the cartilage.
- Fluid pockets may also form within the bone marrow itself, and lead to swelling. The marrow, which runs up through the center of the bone, is rich in nerve fibers. As a result, these injuries can cause pain.
- Breakdown products of the bone and cartilage induce inflammation of the synovium.
- Bone cells may respond to damage by multiplying, growing, and forming dense, misshapen growths around exposed areas where cartilage is completely eroded.
- At the margins of the joint, the bone may produce outcroppings, "bone spurs" or osteophytes, on which new cartilage cells (chondrocytes) multiply and grow abnormally.
Location of Osteoarthritis
Unlike some other types of arthritis, such as rheumatoid arthritis, osteoarthritis does not migrate from one joint to another. Rather, it affects one or a few joints, usually joints that have received extra wear.
Osteoarthritis affects joints differently depending on their location in the body:
- It is common in joints of the fingers, feet, knees, hips, and spine.
- It sometimes occurs in the wrist, elbows, shoulders, and jaw, but it is not as common in these locations.
Causes
The exact causes of osteoarthritis are not known. Scientists think that osteoarthritis most likely develops from a combination of factors, including aging, genetic susceptibility, metabolic factors, and joint injury.
Aging Cells
The body's ability to repair cartilage declines with increasing age. Osteoarthritic cartilage is chemically different from normal cartilage. As chondrocytes (the cells that make cartilage) age, they lose their ability to repair damage and produce more cartilage. This process likely plays an important role in the development and progression of osteoarthritis.
Genetic Factors
Osteoarthritis tends to run in families. Genetic factors may be involved in about half of osteoarthritis cases in the hands and hips, and in a lower percentage of cases in the knee. Several genes that might contribute to an inherited risk are under investigation.
Inflammatory Response
The inflammatory response is a reaction of the immune system to an injury or other assault in the body, such as an infection. This response causes specific immune factors, called cytokines, to gather in injured areas and cause inflammation. Sometimes this can lead to chronic or persistent inflammation that does not resolve itself and can damage body tissues and cells. The inflammatory response plays an important role in rheumatoid arthritis, and other muscle and joint problems associated with autoimmune diseases.
Inflammation is probably less important during the early stages of osteoarthritis and is more likely to be a result, not a cause, of the disease. However, inflammation may contribute to the progression of osteoarthritis and in its chronic nature. The effects of the inflammatory response in osteoarthritis are likely to be different, and less severe, than those in rheumatoid arthritis.
Joint Injury
Joint damage from injuries or recurrent stress to the joint is often the starting point in the osteoarthritis disease process. Osteoarthritis sometimes develops years after a single traumatic injury to or near a joint. People with knee injuries may be up to 5 times more likely to develop osteoarthritis in the injured knee than those without injuries, and people with hip injuries may be more than 3 times more likely to develop arthritis in the injured hip. Proper treatment of injuries may help prevent the development of osteoarthritis. Ligament injuries have been shown to lead to osteoarthritis in the joint.
Medical Conditions That Can Cause Osteoarthritis
Other causes of osteoarthritis include:
- Bleeding disorders that cause bleeding in the joint, such as hemophilia
- Disorders (such as sickle cell anemia) that block the blood supply near a joint, such as avascular necrosis
- Complications of persistent, inflammatory arthritic conditions, particularly chronic gout, pseudogout, or rheumatoid arthritis
- Conditions that cause iron build-up in the joints, such as hemochromatosis
- Anatomical abnormalities, such as mismatched surfaces on the joints, which can become damaged over time. Legs of unequal length, misaligned knees, or skewed feet can cause jerky movement that may lead to osteoarthritis.
Risk Factors
Age
Osteoarthritis can affect people of any age, but it is more common in older people. It rarely occurs in people younger than age 40.
Gender
In people younger than age 45, osteoarthritis occurs more frequently in men. After age 45, it develops more often in women. Some research suggests that women may experience greater muscle and joint pain than men.
Obesity
Obesity increases the risk for osteoarthritis. It also worsens osteoarthritis once deterioration begins. This higher risk is due to increased weight on the joints.
Work and Leisure Factors
Because injuries can trigger the disease process, people involved in jobs or leisure activities that place them at risk for muscle and joint injuries may face a higher risk for osteoarthritis later on in life.
Occupational Risks
Certain occupations with repeated stressful motions (squatting or kneeling with heavy lifting) can contribute to the deterioration of cartilage. People with jobs that require kneeling or squatting for more than an hour a day are at high risk for knee osteoarthritis. Jobs that involve lifting, climbing stairs, or walking also pose some risk.
Exercise
There have been questions about the role of strenuous exercise in osteoarthritis. Sports that definitely pose a higher risk for osteoarthritis have repetitive or direct joint impact (such as football), joint twisting, or both (baseball pitching or soccer).
Regular and moderate exercise is, however, important for everyone and does not increase the risk for osteoarthritis. In middle-aged and older people, recreational weight-bearing exercise (walking and jogging), neither prevents osteoarthritis nor increases risk. Furthermore, many factors associated with a sedentary life (muscle weakness and obesity) are associated with a higher risk for osteoarthritis.
Symptoms
The pain of osteoarthritis begins gradually and progresses slowly over many years. Some people may have no symptoms at all, despite radiographic evidence of osteoarthritis.
Osteoarthritis is commonly identified by the following symptoms:
- Stiffening after first awakening in the morning or after periods of inactivity later in the day. Stiffness (called gelling) resolves with activity, usually in less than 30 minutes.
- Pain that worsens during activity and gets better during rest. This is the most common symptom of osteoarthritis. As the disease advances, the pain may occur even when the joint is at rest.
- Pain that is generally described as aching, stiffness, and loss of mobility. The symptoms are often worse when resuming activities after periods of inactivity.
- Pain that may be intermittent, with bad spells followed by periods of relative relief.
- Pain that seems to increase in humid weather.
- Muscle spasms and contractions in the tendons.
- A grating sensation when the joint is used. Osteoarthritis in the knee may cause a crackling noise (called crepitus) when the affected knee is moved.
Symptoms by Location
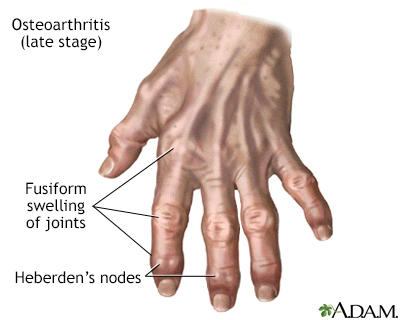
Hand
Osteoarthritis of the hand occurs most often in older women and may be inherited within families. The following joints are most frequently affected:
- Distal interphalangeal (DIP) joint. The first joint below the fingertips is the most common location of osteoarthritis of the hand. These joints can develop bony growths known as Heberden's nodes.
- Carpometacarpal (CMC) joint. The joint at the base of the thumb, where the thumb joint connects with the wrist, is the second most common location.
- Proximal interphalangeal (PIP) joint. The middle joints of the fingers can also develop osteoarthritis. These joints may develop small, solid lumps (nodules) known as Bouchard's nodes.
Osteoarthritis of the hand may predict later development of osteoarthritis in the hip or knee.
Knee
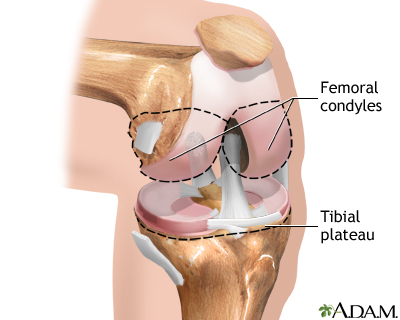
Osteoarthritis is particularly debilitating in the weight-bearing joints of the knees. The meniscus, the cartilage pad between the joint formed by the thighbone and the shinbone, plays an important role in protecting this joint. It acts as a shock absorber. Tears of the meniscus occurring from injury are associated with earlier development of osteoarthritis. The joint is usually stable until the disease reaches an advanced stage when the knee becomes enlarged and swollen. With osteoarthritis progression, the alignment of bones may be disrupted, and knee deformity may occur, such as varus (bow-legged), or valgus (knock-kneed) deformity. Although painful, the arthritic knee usually retains reasonable flexibility.
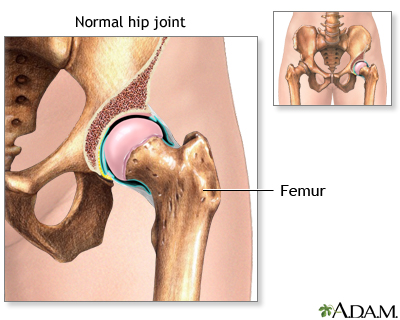
Hips
One in four people develop hip arthritis over the course of their lifetime. Being obese increases the risk. Osteoarthritis frequently strikes the weight-bearing joints in 1 or both hips. Pain develops slowly, usually in the groin and on the outside of the hips, or sometimes in the buttocks. Pain may also radiate to the knee, confusing the diagnosis. Those with osteoarthritis of the hip often have a restricted range of motion (particularly when trying to rotate the hip) and walk with a limp, because they slightly turn the affected leg to avoid pain.
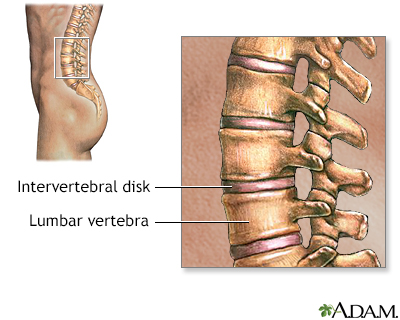
Spine
Osteoarthritis may affect the cartilage in the disks that form cushions between the bones of the spine, the moving joints of the spine itself, or both. Spinal osteoarthritis can affect the neck (cervical), mid-back (thoracic), or lower back (lumbar) regions. Osteoarthritis in any of these locations can cause pain, muscle spasms, and diminished mobility. In some cases, the nerves may become pinched, which produces radiating pain. Advanced disease may result in numbness and muscle weakness.
Shoulder
Osteoarthritis is less common in the shoulder area than in other joints, but it may develop in the shoulder joint (the glenohumeral joint). In such cases, it is most often associated with a previous injury, and patients gradually develop pain and stiffness in the back of the shoulder. Osteoarthritis also can develop in the acromioclavicular (AC) joint, which is between the shoulder blade and the collarbone. However, it rarely causes symptoms in this location.
Diagnosis
Diagnosis of osteoarthritis is based on physical symptoms, medical history, and x-ray images. Other tests may also be performed.
Medical History
Your doctor will ask you about the type of pain you experience, when it occurs, how long it lasts, and whether you have ever injured the joint.
Physical Exam
In osteoarthritis, the affected joint is generally tender to pressure along the joint line. Joint movement may cause a crackling sound. The bones around the joints may feel larger than normal. The joint's range of motion is often reduced, and normal movement is often painful.
Imaging Tests
Osteoarthritis is often visible in x-rays. Cartilage loss is suggested by certain characteristics of the images, such as:
- Narrowed space between the bones in a joint
- An abnormal increase in bone density in areas immediately underneath cartilage
- Bony projections or spurs (called osteophytes), cysts, or erosions
Some people may have osteoarthritis even though it does not show up on an x-ray. Likewise, other people may have minimal symptoms even though an x-ray clearly shows they have osteoarthritis.
An MRI exam of an arthritic joint is generally not needed, unless the doctor suspects other causes of pain.
X-rays are a form of ionizing radiation that can penetrate the body to form an image on film. Structures that are dense (such as bone) will appear white, air will be black, and other structures will be shades of gray depending on density. X-rays can provide information about obstructions, tumors, and other diseases, especially when coupled with the use of various contrast materials.
Synovial Fluid Tests
If the diagnosis is uncertain or infection is suspected, your doctor may recommend taking a sample of synovial fluid from the joint. The doctor inserts a sterile needle into the joint and withdraws the synovial fluid into a syringe attached to the needle.
The fluid is sent to a laboratory for analysis, which may reveal:
- Cartilage cells in the fluid are signs of osteoarthritis.
- A high white blood cell count is a sign of infection, gout, pseudogout, or rheumatoid arthritis.
- Uric acid crystals in the fluid are an indication of gout.
Other abnormalities may suggest different arthritic conditions, including Lyme disease and rheumatoid arthritis.
Blood Tests
Blood test results may help identify other types of arthritis besides osteoarthritis. Some examples include:
- Elevated levels of rheumatoid factor (specific antibodies in the blood) are usually found in patients with rheumatoid arthritis
- Abnormal results for tests such as the erythrocyte sedimentation rate (ESR, or "sed rate") and C-reactive protein (CRP) indicate inflammation, which may be caused by conditions such as rheumatoid arthritis or systemic lupus erythematosus
- Elevated uric acid levels in the blood may indicate gout
Ruling Out Conditions with Similar Symptoms
Numerous conditions cause symptoms of joint aches and pains. Something as simple as sleeping on a bad mattress or as serious as cancer can mirror symptoms of osteoarthritis. Other problems that can cause aches and pains in the joints include physical injuries, infections, tendinitis, and poor circulation.
Osteoarthritis can generally be distinguished from other joint diseases by considering several factors together:
- Osteoarthritis usually occurs in older people and is located in only one or a few joints.
- The joints are less inflamed than in other arthritic conditions.
- Progression of pain is usually gradual.
Below are a few of the most common disorders that can be confused with, or may even accompany, osteoarthritis.
Rheumatoid Arthritis
Osteoarthritis can be confused at times with milder forms of rheumatoid arthritis, particularly when osteoarthritis affects multiple joints in the body. Rheumatoid arthritis normally occurs earlier in life than osteoarthritis, often affecting people in their 30s and 40s. This condition can also be passed on genetically. Rheumatoid arthritis affects many joints, and often occurs symmetrically on both sides of the body. People with rheumatoid arthritis generally have morning stiffness that lasts for at least an hour. (Stiffness from osteoarthritis usually clears up within half an hour.) Although osteoarthritis can occasionally cause swollen, red joints, this appearance is much more typical of rheumatoid arthritis and other types of inflammatory arthritis. In addition to blood tests, x-rays can help show differences between rheumatoid arthritis and osteoarthritis.
Rheumatoid arthritis is a body-wide (systemic) autoimmune disease that initially attacks the synovium, a connective tissue membrane that lines the cavity between joints and secretes a lubricating fluid known as the synovial fluid.
Chondrocalcinosis (Pseudogout)
Chondrocalcinosis (pseudogout syndrome) is a disease in which a certain type of calcium crystal known as CPPD (calcium pyrophosphate dihydrate) accumulates in the joints. This condition can accompany and even worsen osteoarthritis. Chondrocalcinosis is also called pseudogout or pseudo-osteoarthritis, particularly the latter when it affects the knees. A doctor can usually differentiate between the 2 disorders because chondrocalcinosis usually damages other joints (wrists, elbows, and shoulders) that are not normally affected by osteoarthritis.
Charcot's Joint
Charcot's joint occurs when an underlying disease, usually diabetes, causes nerve damage in the joint, which leads to swelling, bleeding, increased temperature, and changes in bone. There may be a loss of sensation that leads to an increased risk of injury from overuse. The nerve pain associated with Charcot's joint may be mistaken for osteoarthritis.
Treatment
There is no cure for osteoarthritis, but there are many treatments that can relieve symptoms and significantly improve the quality of life.
The goals of osteoarthritis treatment are to reduce pain and improve joint function. Treatment approaches include:
- Lifestyle Changes. Lifestyle modifications and non-drug therapies are an important first step for treatment and are used in combination with other treatment modalities. Lifestyle measures include exercise, weight loss, hot and cold therapies, pain management techniques, and the use of mechanical aids, such as braces, and assistive devices, such as crutches and walkers.
- Medications. For mild pain relief, doctors recommend acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and topical ointments. People with more severe pain may require stronger narcotic pain medication or occasional corticosteroid injections.
- Surgery. Some surgical procedures are used for earlier-stage osteoarthritis when only one section (compartment) of the knee has been damaged. For severe osteoarthritis that is not helped by other treatments, joint replacement may be recommended.
Lifestyle Changes
Lifestyle changes can help reduce stress on affected joints.
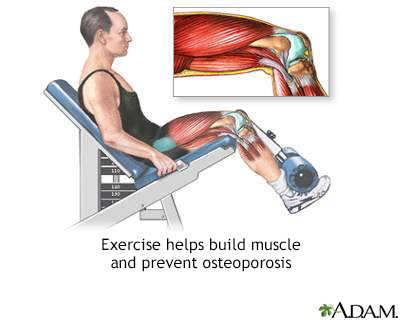
Exercise
Joints need motion to stay healthy. Long periods of inactivity cause the arthritic joint to stiffen and the adjoining tissue to waste away (atrophy). A moderate exercise program that includes low-impact aerobics and power and strength training has benefits for people with osteoarthritis. Even light-intensity exercise can help prevent osteoarthritis progression and disability.
Exercise helps:
- Promote weight loss.
- Reduce stiffness and increase flexibility. It may also help improve the strength and elasticity of knee cartilage.
- Improve muscle strength, which in turn improves balance and endurance.
- Reduce stress and improve feelings of wellbeing, which helps people cope with the emotional burden of pain.
Exercise is generally recommended for all OA patients. Exercise especially helps people with mild-to-moderate osteoarthritis in the hip or in the knee. Many people who begin an aerobic or resistance exercise program report less disability and pain. They are better able to perform daily chores and remain more independent than their inactive peers. Older people and those with medical problems should always check with their doctors before starting an exercise program.
Three types of exercise are best for people with osteoarthritis:
- Strengthening and resistance exercise
- Range-of-motion exercise
- Aerobic, or endurance, exercise
Strengthening and Resistance Exercise
Strengthening exercises include isometric exercises (pushing or pulling against static resistance). Isometric training builds muscle strength while burning fat, helps maintain bone density, and improves digestion. For people with arthritis in the hip or knees, exercises that strengthen the muscles of the upper leg are important.
Exercise, such as weightlifting, helps build muscle that is usually lost with age and puts stress on bones, keeping them strong and healthy.
Range-of-Motion Exercise
These exercises increase the amount of movement in joints. In general, they are stretching exercises. The best examples are yoga and tai chi, which focus on flexibility, balance, and proper breathing. The latest clinical guidelines from the American College of Rheumatology strongly recommend tai chi for osteoarthritis of the hip and knee.
Aerobic Exercise
Aerobic exercises help control weight and may reduce inflammation in some joints. Low-impact workouts also help stabilize and support the joint. Cycling, walking, elliptical training, and cross-country skiing can be beneficial for people with osteoarthritis. However, weight-bearing exercise and even bicycling can place added stress on hips, knees, or ankles when arthritis is already present. Swimming or exercising in water is highly recommended. People with osteoarthritis should avoid high-impact sports such as jogging, tennis, and racquetball if they cause pain.
Weight Reduction
Overweight people with osteoarthritis can lessen the shock on their joints by losing weight. Knees, for example, sustain an impact 3 to 5 times the bodyweight when descending stairs. Losing 5 pounds of weight can eliminate 20 pounds of stress on the knee. The greater the weight loss achieved, the greater the benefit will be. The American Academy of Orthopedic Surgeons recommends that people with a body mass index (BMI) greater than 25 should try to lose at least 5% of their body weight.
Weight reduction is best achieved through both diet and exercise. Studies indicate that for overweight people with osteoarthritis, a combination of diet and exercise is the most effective way to help reduce pain and improve functioning.
Physical Therapy
Physical therapy can be helpful for osteoarthritis by teaching you how to strengthen muscles that support a joint and to add flexibility to a joint.
A physical therapist will use a variety of techniques to help increase strength, flexibility, and range of motion in the joints. The therapist will use hands-on treatment and may also apply other modalities.
For example, ultrasound therapy uses high-energy sound waves to produce heat within the tissue. The therapist applies gel to the affected area (usually the knee) and moves a handheld ultrasound transducer over the joint. There is, however, no clear evidence that this therapy provides much carryover benefit.
A physical therapist can show you ways to more easily perform daily tasks of living without putting stress on your joints. Your therapist can recommend how to make changes in your workplace or work tasks to avoid repetitive or damaging motions. Your therapist may also advise you on hot or cold treatments to use for pain.
Heat and Ice
Ice
When a joint is inflamed (particularly in the knee) applying ice for 20 to 30 minutes can be helpful. If an ice pack is not available, a package of frozen vegetables works just as well.
Heat Treatments
Soaking in a warm bath or applying a heating pad may help relieve stiffness and pain.
Mechanical Aids
A wide variety of devices are available to help support and protect joints, although it is unclear how effective they are. Some of these devices include splints or braces, and shoe inserts or orthopedic shoes. However, evidence suggests that lateral wedge insoles are not helpful for knee osteoarthritis. An offloading (also called unloading) brace is commonly used for knee osteoarthritis to help transfer the weight off the affected joint.
Assistive Devices
There are many different types of assistive devices that can help make your life easier in the home. Kitchen gadgets, such as jar openers, assist with gripping and grabbing. Door-knob extenders and key turners are helpful for people who have trouble turning their wrists. Bathrooms can be fitted with shower benches, grip bars, and raised toilet seats. An occupational therapist can advise you on choosing the right kinds of assistive devices.
Pain Management
Relaxation
Relaxation techniques such as guided imagery and breathing exercises may help some people better cope with chronic pain.
Acupuncture
Some people use acupuncture to reduce osteoarthritis pain. The technique is painless and involves the insertion of small fine needles at select points in the body. Acupuncture is considered a safe alternative medicine approach. Some, but not all, studies have found that acupuncture is effective for treating chronic pain and can help provide pain relief for osteoarthritis.
TENS
Transcutaneous electric nerve stimulation (TENS) uses low-level electrical pulses to suppress pain. A variant (sometimes called percutaneous electrical nerve stimulation, or PENS) applies these pulses through a small needle to acupuncture points. Recent studies have not found improvements with TENS treatment, and the American College of Rheumatology guidelines recommend against its use for osteoarthritis.
Massage
Massage therapy may help provide short-term pain relief for some people. It is important to work with an experienced massage therapist who understands how not to injure sensitive joint areas.
Herbs and Dietary Supplements
Glucosamine and Chondroitin
Glucosamine hydrochloride and chondroitin sulfate are natural substances that are part of the building blocks found in and around cartilage. For many years, researchers have been studying whether these dietary supplements really work for relieving osteoarthritis pain. Earlier studies suggested a potential benefit from these supplements.
However, more recent high-quality studies involving large numbers of patients have indicated that glucosamine and chondroitin, either alone or in combination, do not seem to work any better than a placebo for relieving symptoms of osteoarthritis.
Based on these studies, the American College of Rheumatology recommend against the use of these supplements.
Generally, manufacturers of herbal remedies and dietary supplements do not need FDA approval to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been several reported cases of serious and even lethal side effects from herbal products. Always check with your doctor before using any herbal remedies or dietary supplements.
Medications
Acetaminophen
Acetaminophen (Tylenol, generic) is one of the top choices for treating mild-to-moderate osteoarthritis pain. Acetaminophen is an analgesic that helps relieve pain but unlike NSAIDs it does not help reduce inflammation.
Acetaminophen is inexpensive and generally safe. It poses far less of a risk for gastrointestinal problems than NSAIDs. However, it does pose a risk for liver damage if more than the prescribed amount is taken. Drinking alcohol while taking acetaminophen significantly increases the risk for liver damage. Long-term, high-dose acetaminophen therapy may increase the risk for high blood pressure.
The FDA-recommended daily dose limit of acetaminophen is 4,000 mg but many doctors advise not taking more than 3,000 mg per day. Carefully read the label of your acetaminophen bottle because dosage amounts vary depending on the product. For example, regular strength acetaminophen contains 325 mg per pill, while "arthritis pain" branded products contains 650 mg of acetaminophen per pill. Many combination cold products also contain acetaminophen, and additional care should be exercised when taking these drugs to not pass the maximum daily dosage.
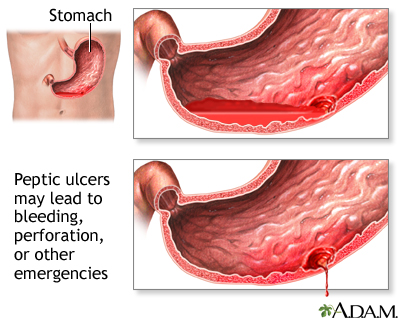
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) block prostaglandins, the substances that dilate blood vessels and cause inflammation and pain. Oral NSAIDs are the first choice short-term drug treatment for osteoarthritis. There are dozens of NSAIDs:
- Over-the-counter NSAIDs include aspirin, ibuprofen (Advil, Motrin, generic), naproxen (Aleve, Naprosyn, generic), and ketoprofen (Actron, Orudis KT, generic).
- Prescription NSAIDs include flurbiprofen (Ansaid, generic), diclofenac (Voltaren, Cataflam, Arthrotec, generic), tolmetin (Tolectin, generic), ketoprofen (Orudis, generic), nabumetone (Relafen, generic), indomethacin (Indocin, generic), celecoxib (Celebrex, generic), and meloxicam (Mobic, generic).
- Topical NSAIDs are gels, creams, or patches that are available either by prescription or over-the-counter. The American College of Rheumatology recommends the use of topical NSAIDs such as trolamine salicylate (Aspercreme, Myoflex, generic) for hand or knee osteoarthritis. (See Capsaicin section below for safety information about these products.)
Oral NSAIDs should be used only for short periods of time. Long-term use of NSAIDs does not delay the progression of osteoarthritis and can increase the risk of side effects.
Use only the lowest effective dose of NSAIDs. High dosages can cause heart problems (such as increased blood pressure and risk of heart attack), kidney problems, and stomach bleeding. Because of these risks, the American College of Rheumatology recommends using topical NSAIDs in place of oral NSAIDs, for people age 75 years and older.
People who take daily low-dose aspirin for heart protection should consider using an oral NSAID other than ibuprofen. Ibuprofen may make the aspirin less effective.
People who are at increased risk of stomach bleeding and ulcers should switch to another type of pain reliever or take the NSAID along with a proton-pump inhibitor drug, such as omeprazole (Prilosec, generic) or esomeprazole (Nexium), an H2 blocker such as famotidine (Pepcid, generic), or with the synthetic prostaglandin misoprostol (Cytotec, generic). (Misoprostol can cause miscarriage and should not be used by women who may be pregnant.) Some NSAIDs are available as combination pills; they include diclofenac/misoprostol (Arthrotec, generic) and ibuprofen/famotidine (Duexis).
Capsaicin and Other Topical Products
Capsaicin is a component of hot red peppers and may bring pain relief when used as a skin cream (Zostrix, generic). This is the only skin preparation that does more than just mask pain or reduce it temporarily. With repeated applications, capsaicin seems to reduce a substance in the body, known as substance P, which contributes both to inflammation and the delivery of pain impulses to the central nervous system.
A small amount of capsaicin must be applied to the area of inflammation about four times a day. During the first few days of use, capsaicin causes a warm, stinging sensation when the cream is applied. This sensation goes away, and pain relief usually begins within 1 to 2 weeks. The American College of Rheumatology recommends topical capsaicin for hand osteoarthritis but not for knee or hip osteoarthritis.
Topical over-the-counter joint pain relievers that contain menthol, methyl salicylate, and (less commonly) capsaicin may in rare cases cause chemical burns. Menthol and methyl salicylate products are sold under brand names such as Bengay, Flexall, Icy Hot, and Mentholatum. Products that contain capsaicin include Capzasin as well as Zostrix. The risks appear more severe for combination products that contain higher doses of both menthol (greater than 3%) and methyl salicylate (greater than 10%).
The FDA warns:
- Do not apply these products to damaged or irritated skin
- Do not apply bandages, heating pads, or hot water bottles to areas treated with these products
- If you see any signs of blisters or burns, stop using the product and seek medical attention.
These warnings also apply to the topical NSAID products that contain trolamine salicylate (see NSAIDs section above).
Duloxetine (Cymbalta)
Duloxetine (Cymbalta, generic) is a selective serotonin-norepinephrine reuptake inhibitor (SSNRI) antidepressant that is used to treat depression, anxiety disorders, diabetic nerve pain, and fibromyalgia. In 2010, the FDA approved duloxetine for the treatment of chronic musculoskeletal pain associated with osteoarthritis.
Depression
An in-depth report on the causes, diagnosis, treatment, and prevention of depression.

| Read Article Now | Book Mark Article |
Tramadol
Tramadol (Ultram, generic) is a pain reliever that has been used as an alternative to opioids. However, Tramadol has opioid-like properties and the same addictive properties as opioids, with the potential for dependence and abuse. Tramadol can cause nausea but does not cause severe gastrointestinal problems, as NSAIDs can. Some people experience severe itching. A combination of tramadol and acetaminophen (Ultracet, generic) is available, but has the same associated addiction risks.
Narcotics
Narcotics are pain-relieving and sleep-inducing drugs that act on the central nervous system. They are the most powerful medications available for the management of moderate-to-severe pain. There are 2 types of narcotics:
- Opiates, which are derived from natural opium (morphine and codeine)
- Opioids, which are synthetic drugs. They include oxycodone (such as Percodan, Percocet, Roxicodone, Oxycontin, generic), hydrocodone (Vicodin, generic), oxymorphone (Opana, generic), and fentanyl (Duragesic, generic)
The use of narcotics for arthritic pain is controversial. These drugs are highly addictive and should be prescribed at the lowest possible effective dose. Their use should be limited to rare cases when safer drugs are not effective or appropriate.
Common side effects include anxiety, constipation, nausea and vomiting, dizziness, drowsiness, paranoia, urinary retention, restlessness, and labored or slow breathing.
Corticosteroid Injections
When pain becomes a major problem and less potent pain relievers are ineffective, doctors may try corticosteroid (steroid) injections into the joint. Corticosteroid shots are useful only if inflammation is present in the joint. Relief from pain and inflammation is of short duration, and this treatment is rarely used for chronic osteoarthritis. The American College of Rheumatology does not recommend these injections for hand osteoarthritis.
Corticosteroid injections are usually given every 3 months. People should not have more than 2 or 3 injections a year, since there is some concern that repeated injections over the long term may be harmful. Because long-term use of corticosteroids has many potentially serious side effects, steroid medications are never given by mouth (systemically) for the treatment of osteoarthritis.
Hyaluronic Acid Injections (Viscosupplementation)
Injections of hyaluronic acid (Hyalgan, Synvisc, and Euflexxa) into the joint, a procedure called viscosupplementation, is a controversial treatment for knee osteoarthritis. Evidence indicates that these injections provide modest, short-term pain relief at best. Some studies suggest these injections may increase the risk for swelling and inflammation. The American Academy of Orthopedic Surgeons and the American College of Rheumatology no longer recommend viscosupplementation as a treatment for people with symptomatic osteoarthritis of the knee or hip.
Surgery
If lifestyle measures and medications fail to relieve pain and increase function, surgery may be an option. Certain surgical procedures can help relieve pain if medications fail. Even with these procedures, joint replacement may still be needed later on.
Joint Replacement (Arthroplasty)
When osteoarthritis becomes so severe that pain and immobility make normal functioning impossible, people may be eligible for artificial (prosthetic) joint implants using a procedure called arthroplasty. Arthroplasty involves removing the surfaces of the joint and replacing them with an artificial material made of metal, plastic, or other material.
Hip replacement (total hip arthroplasty) is the most established and successful replacement procedure, followed by knee replacement. Other joint surgeries (shoulders, elbows, wrists, and fingers) are less common, and some arthritic joints (in the spine, for instance) cannot yet be treated in this manner.
Candidates
In evaluating the need for surgery, a person's pain and disability are more important considerations than age or other factors (such as weight).
Joint replacement is effective for people of all ages. While older people may take longer than younger people to achieve full recovery, the long-term outcome of the surgery is usually excellent, and can lead to significant improvements in pain and quality of life. In the past, surgeons generally recommended delaying joint replacement for younger people, because of concerns of implants wearing out and the need for additional revision procedures in the future. Newer, longer-lasting materials are helping to reduce the need for revision operations.
Complications
Complications from joint replacement can occur and, in rare cases, be life-threatening. In addition to blood loss and infection, deep blood clots in the legs (deep venous thrombosis) are a serious potential complication. These clots can potentially travel to the lungs (pulmonary embolism) and pose a risk for death. People who are overweight are at higher than average risk for blood clots.
Metal ball and socket components are sometimes used in both total hip replacement and hip resurfacing procedures. The FDA is currently reviewing the safety of these "metal-on-metal" components to see if they increase swelling and pain. There is also concern that metal ions (particles) may be released into the bloodstream, where they might trigger allergic reactions and other problems. Talk with your surgeon about the type of materials that will be used in your procedure and their possible risks and benefits. If you experience any swelling or pain after surgery, be sure to notify your doctor.
Recovery and Rehabilitation
Aside from the surgeon's skill and the person's underlying condition, the success rate depends on the kind and degree of activity the joint receives following replacement surgery. Physical therapy takes about 6 weeks to rebuild adjoining muscle and strengthen surrounding ligaments. People typically experience considerable pain during this time.
While many people find that joint replacement eventually provides pain relief and restores some mobility, they need time to adjust to the artificial joint.
Limitations after hip surgery include:
- Usually people with new hips are able to walk several miles a day and climb stairs, but they cannot run.
- Prosthetic hips should not be flexed beyond 90 degrees, so people must learn new ways to perform activities requiring bending down (like tying a shoe).
Limitations after knee surgery include:
- Walking distance improves after knee replacement surgery, but people still cannot run.
- Artificial knee joints generally have a limited range of motion of just 110 degrees and stair climbing may remain difficult.
Minimally Invasive Arthroplasty
Surgeons are exploring a variety of new techniques for a minimally invasive approach to knee and hip arthroplasty. They include using a shorter incision, and new types of smaller specialized instruments. The goal is to give the person a shorter recovery time and less postoperative pain. However, minimally invasive arthroplasty is still in its early stages. At this time, there is no consensus on which minimally invasive technique works best, or if it actually achieves any additional benefits beyond the recovery period.
Computer-assisted Surgery
Numerous factors can disrupt the ideal positioning of artificial joint parts during arthroplasty procedures, resulting in incorrect joint functioning after the operation. Computer-assisted surgery is currently investigated as a method to increase the accuracy in the placement of prosthetic components for hip and knee arthroplasty. Computer-assisted navigation systems can be image-free, fluoroscopic, and CT-based. Preliminary studies indicate improved arthroplasty outcomes with the use of computer-assisted navigation.
Alternatives to Total Joint Replacement
Surgical alternatives to total knee or hip joint replacement include:
- Unicompartmental knee arthroplasty (also called partial joint replacement) involves replacing damaged cartilage in only one part of the knee. The surgery may be performed in the inside part of the knee (medial), the outside part (lateral), or the part of the knee between the kneecap and thighbone (patellofemoral). This surgery is only recommended for a small percentage of patients whose osteoarthritis damage is confined to a specific part of the knee. People who have this type of surgery may still need total joint replacement at some point in the future.
- Hip resurfacing is a surgical alternative to total hip replacement, which involves removing the hip joint and replacing it with an artificial joint. Hip resurfacing involves scraping the surfaces of the hip joint and femur and placing a metal cap over the bone. Hip resurfacing may provide more stability, a faster recovery, and greater range of motion, making it a potentially good option for young, physically active patients. However, this is a more complicated surgical procedure than total hip replacement.
Realigning Bones (Osteotomy)
Osteotomy is a surgical procedure used to realign bone and cartilage and reposition the joint to help transfer weight from a damaged to healthy part of the knee. The procedure involves making a cut in one of the bones in the lower leg and removing a slice of bone to straighten the leg.
There are 2 types of osteotomy surgery:
- Tibial osteotomy, if the cut is made on the shin bone
- Femoral osteotomy, if the cut is made on the thigh bone
Osteotomy is generally performed for early-stage knee osteoarthritis that has affected only a certain section (compartment) of the knee. According to the American Academy of Orthopedic Surgeons, this procedure works best for people who are thin, active, or younger (40 to 60 years old).
Fusing Bones (Arthrodesis)
If the affected joint cannot be replaced, surgeons can perform a procedure called arthrodesis that eliminates pain by fusing the bones together. The person must understand, however, that fusing the bones makes movement of the joint impossible. Bone fusion is most often done in the spine and in the small joints of the hands and feet.
Arthroscopy and Debridement
Arthroscopy with lavage and debridement is sometimes performed to clean out bone and cartilage fragments that, in theory at least, may cause pain and inflammation. Arthroscopy is also sometimes used to diagnose osteoarthritis. In this procedure, the surgeon makes a small incision and inserts the arthroscope, a pencil-width fiber-optic instrument that contains a light and magnifying lens. The arthroscope is attached to a miniature television camera that allows the surgeon to see the inside of the joint. Saline solution is injected to wash out the debris (lavage) and the fragments are then removed (debridement).
Research and debate continues on whether arthroscopy is truly helpful for osteoarthritis and, if so, which people may benefit the most from it. Most guidelines, including those from the American Academy of Orthopedic Surgeons, do not recommend this treatment for people who have symptoms of osteoarthritis but no other problems such as symptomatic loose fragments or meniscus tears. Arthroscopy may possibly benefit people with mild-to-moderate osteoarthritis who have bone and cartilage fragments in the joint, or people whose joints lock or catch with movement.
Resources
- American College of Rheumatology -- rheumatology.org/
- Arthritis Foundation -- www.arthritis.org
- National Institute of Arthritis and Musculoskeletal and Skin Diseases -- www.niams.nih.gov
- American Academy of Orthopaedic Surgeons -- www.aaos.org
References
Bennell KL, Buchbinder R, Hinman RS. Physical therapies in the management of osteoarthritis: current state of the evidence. Curr Opin Rheumatol. 2015;27(3):304-311. PMID: 25775185 pubmed.ncbi.nlm.nih.gov/25775185/.
Ebell MH. Osteoarthritis: Rapid Evidence Review. Am Fam Physician. 2018;97(8):523-526. PMID: 29671497 pubmed.ncbi.nlm.nih.gov/29671497.
Ferguson RJ, Palmer AJ, Taylor A, et al. Hip replacement. Lancet. 2018;392(10158):1662-1671. PMID: 30496081 pubmed.ncbi.nlm.nih.gov/30496081.
Harkess JW, Crockarell JR. Arthroplasty of the hip. In: Azar FM, Beaty JH, Canale ST, eds. Campbell's Operative Orthopaedics. 13th ed. Philadelphia, PA: Elsevier; 2017:chap 3.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745-1759. PMID: 31034380 pubmed.ncbi.nlm.nih.gov/31034380.
Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21(9):571-576. PMID: 23996988 pubmed.ncbi.nlm.nih.gov/23996988.
Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020 Jan 6. [Epub ahead of print] PMID: 31908163 pubmed.ncbi.nlm.nih.gov/31908163.
Kraus VB, Vincent TL. Osteoarthritis. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier Saunders; 2020:chap 246.
Lavelle DG. Hip Resurfacing. In: Canale ST, Beaty JH, Azar FM, eds. Campbell's Core Orthopaedic Procedures. 1st ed. Philadelphia, PA: Elsevier; 2016:chap 5.
Marshall M, Watt FE, Vincent TL, Dziedzic K. Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nat Rev Rheumatol. 2018;14(11):641-656. PMID: 30305701 pubmed.ncbi.nlm.nih.gov/30305701.
Mihalko WM. Arthroplasty of the knee. In: Azar FM, Beaty JH, Canale ST, eds. Campbell's Operative Orthopaedics. 13th ed. Philadelphia, PA: Elsevier; 2017:chap 7.
Murray PM. Treatment of the osteoarthritic hand and thumb. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS, eds. Green's Operative Hand Surgery. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 11.
Neogi T, Felson D. Osteoarthritis and rheumatoid arthritis. In: McMahon SB, Koltzenburg M, Tracey I, Turk DC, eds. Wall & Melzack's Textbook of Pain. 6th ed. Philadelphia, PA: Elsevier Saunders; 2013:chap 47.
Percope de Andrade MA, Campos TV, Abreu-E-Silva GM. Supplementary methods in the nonsurgical treatment of osteoarthritis. Arthroscopy. 2015;31(4):785-792. PMID: 25633815 pubmed.ncbi.nlm.nih.gov/25633815.
Sharma L. Local and systemic risk factors for incidence and progression of osteoarthritis. In: Hochberg MC, Gravallese EM, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, eds. Rheumatology. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 180.
Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(4):507-515. PMID: 25447976 pubmed.ncbi.nlm.nih.gov/25447976.
Review Date: 2/27/2020
Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.