Headaches - tension - InDepth
Tension-type headache - InDepth; Episodic tension-type headache - InDepth; Muscle contraction headache - InDepth; Headache - benign - InDepth; Headache - tension - InDepth; Chronic headaches - tension - InDepth; Rebound headaches - tension - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of common headaches.
Highlights
What Are Tension-Type Headaches?
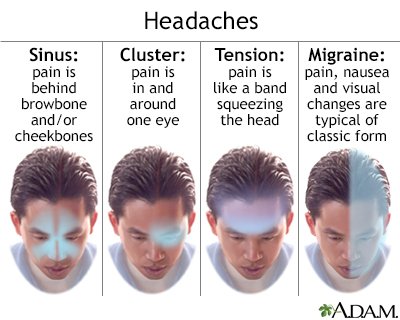
Tension-type headaches are the most common type of headache, accounting for about half of all headaches. The pain is usually mild-to-moderate in intensity, with a steady pressing or tightening quality (like a vise being squeezed around the head). The headache is not accompanied by nausea or vomiting, and the pain is not increased by routine physical activity such as walking or climbing stairs. A tension-type headache attack can last anywhere from 30 minutes to an entire week.
Who Gets Tension-Type Headaches?
Women are slightly more likely to get tension-type headaches than men. Nearly everyone will have at least one tension-type headache at some point in their lives and more than a third of people will experience a tension headache each year. Many people who have migraine headaches also have tension-type headaches.
What Is The Difference Between Tension-Type Headaches and Migraine Headaches?
Migraines and tension headaches have some similar characteristics, but also some important differences:
- Migraine pain is usually throbbing while tension-type headache pain is usually a steady ache.
- Migraine pain often affects only one side of the head while tension-type headache pain typically affects both sides of the head.
- Migraine headaches, but not tension-type headaches, may be accompanied by nausea or vomiting, sensitivity to both light and sound.
- Tension headaches don't typically have a warning or aura.
Treatment
Treatment of tension-type headache focuses on relieving pain when attacks occur, and preventing recurrence of attacks. Most tension-type headache attacks respond to simple nonprescription pain relievers such as aspirin, ibuprofen (Advil, Motrin, generic), or naproxen (Aleve, generic). However, these medications, especially those that contain caffeine, should not be used more than twice a week because they can cause medication overuse (rebound) headaches.
People who have two or more tension-type headache attacks each month should talk to their health care providers about preventive therapy. This may include a tricyclic antidepressant, such as amitriptyline (Elavil, generic), combined with behavioral therapies. Behavioral treatment approaches include relaxation therapy, biofeedback, stress management, and cognitive-behavioral therapy.
Introduction
Most people have had headaches. There are many different kinds of headaches, and they range from being an infrequent annoyance to a persistent, severe, and disabling medical condition. Tension-type headaches are among the most common of all headaches. The pain of a tension-type headache can range from mild to severe and last anywhere from a few minutes to several days.
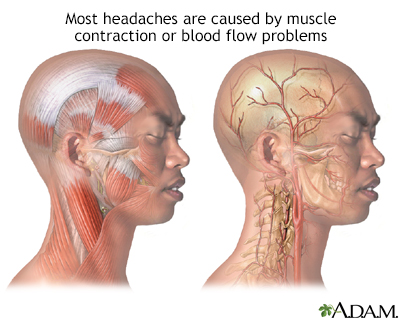
Brain tissue itself does not generate sensations of pain, so the brain is not what hurts when you have a headache. Rather, the pain occurs in some of the following locations:
- The tissues covering the brain
- The attaching structures at the base of the brain
- Muscles and blood vessels around the scalp, face, and neck
Primary and Secondary Headaches
Primary Headaches
A headache is considered primary when it is not caused by another medical condition or disease. Most primary headaches fall into three main types: tension-type, migraine, and cluster headaches. Tension-type headache is the most common type of primary headache.
Migraine
An in-depth report on the causes, diagnosis, treatment, and prevention of migraine.
| Read Article Now | Book Mark Article |
Cluster headaches
An in-depth report on the causes, diagnosis, treatment, and prevention of cluster headaches.
| Read Article Now | Book Mark Article |
Headaches can be caused by problems in the interaction of chemicals in the brain, nerve pathways, and blood vessels.
Secondary Headaches
Secondary headaches are caused by other medical conditions, such as sinus infections, neck injuries, and strokes. Headaches due to abnormalities or infections in the nasal or sinus passages are commonly referred to as sinus headaches.
Episodic and Chronic Headaches
Tension-type headaches are classified as either episodic or chronic based on how frequently they occur:
- Episodic headaches occur on less than 15 days per month. (People who have frequent episodic tension-type headaches, more than 10 days a month, often also have migraine headaches.)
- Chronic headaches occur on more than 15 days per month and have been present for at least 6 months. About 25% of the time, episodic-type headaches evolve into chronic tension-type headaches.
Chronic daily headaches can begin as tension headaches, migraines, or a combination of these or other headache types. Chronic daily headaches are subdivided into 2 categories:
- Short-duration headaches, or those lasting fewer than 4 hours. The most common short-acting chronic headaches are cluster headaches.
- Long-duration headaches, which last more than 4 hours. Tension-type headaches are the most common type of long-duration chronic headaches and are, in fact, the most common type of chronic headaches in general.
Causes
Researchers are not sure what causes tension-type headaches. At one time, these headaches were blamed on abnormal muscle contractions but this theory has largely been discounted. This is why this headache's name has changed from "tension" to "tension-type."
Researchers now think that tension-type headaches most likely occur due to an interaction of several factors that involve pain sensitivity and perception, as well as the role of brain chemicals (neurotransmitters). Several studies have shown abnormalities of serotonin levels in people with tension-type headaches.
Some research has shown abnormal muscle activity in people with tension-type headache. Although muscle tightness does not necessarily cause tension-type headaches, certain triggers associated with muscle contractions or strain may contribute to this condition.
Pain Sensitivity and Perception
Research indicates that people with tension-type headache may have abnormalities in the central nervous system that increase their sensitivity to pain. Tension-type headaches are associated with, and may represent an overlap of other pain syndromes such as fibromyalgia. The central nervous system includes the nerves in the brain and spine.
Tension-type headaches may also be linked to myofascial trigger points in the neck and shoulder muscles. Myofascial pain involves the fascia (connective tissue) and muscles. Trigger points are knots in the muscle tissue that can cause tightness, weakness, and intense pain in various areas of the body. For example, a trigger point in the shoulder may result in headache.
Brain Chemicals (Neurotransmitters)
Neurotransmitters are chemical messengers in the brain. Several types of neurotransmitters affect how the brain reacts to pain stimulation. In particular, serotonin (also called 5-HT) and nitric oxide are thought to be involved in these chemical changes. Release of these chemicals may activate nerve pathways in the brain, muscles, or elsewhere and increase pain.
People with tension-type headache are at increased risk of having depression. It isn't known if depression is a result of having headaches, or an underlying neurotransmitter problem results in both depression and tension-type headache.
Triggers for Tension-Type Headache
Many different factors can trigger or aggravate tension-type headaches.
Stress
Stress certainly plays a role in tension-type headaches. Emotional and psychological factors that contribute to stress include anxiety, depression, and anger. Lifestyle factors include fatigue, lack of sleep, dehydration, and hunger.
Sleep Problems
Sleep disorders, such as insomnia or obstructive sleep apnea, can trigger or worsen tension-type headaches.
Poor Posture
Working or sleeping in an awkward position can contribute to posture problems that affect muscles in the neck and shoulders.
Medication and Substance Overuse
About a third of persistent headaches, including chronic migraine and tension-type, are medication-overuse headaches. They result from a rebound effect caused by the overuse of headache medications. Nearly any type of headache medication can produce this effect. This is true for medications that contain caffeine. Headaches can also occur after withdrawing from caffeine, nicotine, or alcohol.
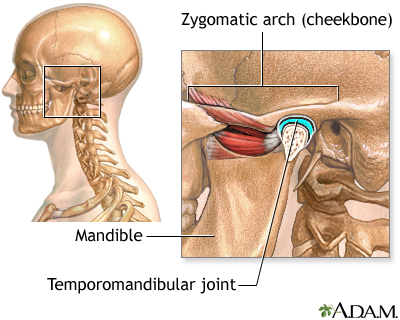
Dental Problems
Jaw clenching or teeth grinding, during sleep, are signs of temporomandibular joint (TMJ) dysfunction. TMJ pain can occur in the ear, cheek, temples, neck, or shoulders. This condition often coexists with chronic tension headache. Some people with TMJ dysfunction may see improvement in tension-type headaches from procedures or exercise therapies that specifically address the dental condition.
Risk Factors
Tension-type headaches are the most common type of headache. Nearly everyone has at least one tension-type headache during their lifetime. Episodic tension-type headaches are far more common than chronic tension-type headaches.
Headaches in Adults
Gender
Tension-type headaches are slightly more common in women than men.
Age
Tension-type headaches are most likely to occur among people in their 30s. They tend to occur less as people become older.
Education
Tension-type headaches occur more commonly in people with higher educational levels.
Headaches in Children
Tension-type headaches are rare before age 4 but become more common throughout childhood, reaching a peak at around age 13, and occurring in as many as 48% of children according to some studies. Children with tension-type headaches often suffer from an accompanying emotional or psychological disorder.
Factors associated with childhood tension-type headaches include:
- Sleep problems. Many children who experience chronic daily headaches suffer from sleep disturbances, especially difficulty falling asleep.
- Mental health conditions. Many children with chronic tension-type headaches also have depression or an anxiety disorder.
- Family stress. Stressful family events can contribute to emotional problems that lead to tension-type headaches.
- Problems at school. According to a National Headache Foundation survey, nearly 30% of children miss school because of headaches. For many children, the start of the school season can be a particularly stressful time.
The National Headache Foundation recommends these tips for parents:
- Keep a diary of your child's headaches noting time of onset, length and intensity of attack, location of pain, and dietary triggers.
- Make sure your child gets plenty of sleep at regular times.
- Avoid changes in your child's eating routine (hunger and eating at irregular times can trigger headaches).
- Discuss any headache concerns with your child's provider.
Prognosis
Both episodic and chronic tension-type headache can affect quality of life. However, tension-type headache episodes are rarely disabling, and rarely require emergency treatment. If they do, there is usually a migraine component occurring with the tension-type headache.
Although they are not medically dangerous, chronic tension headaches can have a negative impact on quality of life, social relations, and work productivity. Several studies have reported lower quality of life for people with any chronic daily headache compared to those with no headaches or only episodic ones. Many people with chronic tension-type headaches also suffer from anxiety and depression.
Tension-type headaches can, in most cases, be treated and prevented. Episodes of these headaches can also resolve over time. In one study, nearly half of people with frequent or chronic tension-type headache were not experiencing headaches when examined 3 years later. People who have both tension-type and migraine headaches may face steeper challenges in recovery.
Symptoms
Tension-type headaches (episodic and chronic) tend to have the following symptoms:
- Pressing or tightening (but non-pulsating) pain
- Mild-to-moderate pain on both sides of the head
- Not aggravated by routine physical activity (such as walking or climbing stairs)
The absence of other features helps differentiate tension-type headaches from other kinds of headaches.
Episodic tension-type headaches are also characterized by:
- No nausea or vomiting
- Extreme sensitivity to bright light (photophobia) and extreme sensitivity to sound (phonophobia) are either both absent or only one of these symptoms may be present
Chronic tension-type headaches are also characterized by:
- No vomiting
- No moderate or severe nausea
- No more than one of the following symptoms: mild nausea, sensitivity to light, or sensitivity to sounds
- Discomfort triggered by manual palpitation of the head (pericranial tenderness)
Differentiating Tension-Type Headaches from Migraine Headaches
Migraines and tension-type headaches have some similar symptoms and some people may have both of these types of headaches. However, there are important differences between migraines and tension-type headaches:
- Migraine pain is usually throbbing, while tension-type headache pain is usually a steady ache.
- Migraine pain usually affects only one side of the head, while tension-type headache pain typically affects both sides of the head.
- Migraine pain, but not tension-type pain, worsens with head movement.
- Migraine headaches, but not tension-type headaches, may be accompanied by moderate-to-severe nausea and vomiting.
- Migraine headaches, but not tension-type headaches, may be accompanied by sensitivity to both light and sound.
- Migraine headaches may be accompanied by visual disturbances called auras. Tension-type headaches do not have auras.
Diagnosis
The diagnosis of tension-type headache is based on symptoms, medical history, and a physical exam. The provider may recommend you keep a headache diary to track the occurrence and intensity of headache attacks. For chronic, severe, or unusual headaches, the provider may conduct a neurological exam or order imaging tests.
Medical and Personal History
You should inform your provider about:
- Duration and frequency of headaches.
- Location of the pain.
- Type of pain (throbbing or steady pressure).
- Intensity of the pain.
- Associated symptoms, such as visual disturbances or nausea and vomiting. (These are seen most often with migraines.)
- Behavior during a headache. Different behaviors may help distinguish between migraine and tension headaches. People with tension headaches tend to relieve pain by massaging the scalp, temples, or the nape of the neck. People with migraines are more likely to press the forehead and temples or to apply a cold pack to the area.
You should also report any other conditions that might be associated with headache, such as any:
- Chronic or recent illness and their treatments
- Injuries, particularly head or back injuries
- Dietary changes
- Current medications or recent withdrawal from any drugs, including over-the-counter or natural remedies
- History of caffeine, alcohol, or drug abuse
- Stress, depression, or anxiety
The provider will also ask about your general medical and family history, particularly concerning headaches or other neurological diseases.
Headache Diary to Identify Triggers
Keeping a headache diary is a useful way to identify triggers that bring on headaches, and to help differentiate between migraine and tension-type headache. Keeping a headache diary will help your healthcare provider better classify your headache. Be sure to include all events preceding an attack. Often two or more triggers interact to produce a headache.
Tracking medications is an important way of identifying medication-overuse headache. Many persistent headaches result from the rebound effect caused by the overuse of headache medications.
Try to define the intensity of the headache. There are different scoring symptoms available that help measure severity of pain. For instance, the following is a number system that can be helpful:
- = Mild, barely noticeable
- = Noticeable, but does not interfere with work/activities
- = Distracts from work/activities
- = Makes work/activities very difficult
- = Incapacitating
Physical Examination
The provider will examine the head and neck to check for muscle tenderness. The provider may also perform a neurologic examination, which includes a series of simple evaluations to test strength, reflexes, coordination, sensation, and mental function. The provider may also recommend an eye examination.
Imaging Tests
Imaging tests look for any serious medical condition as the cause of headache. For people who have stable headaches, they are generally not recommended except for sudden new or worsening symptoms. For imaging tests, magnetic resonance imaging (MRI) is preferred over computed tomography (CT) scans because MRIs do not expose people to radiation.
Imaging tests of the brain may be recommended under the following circumstances:
- If the results of the medical history and physical examination suggest neurologic problems
- Changes in vision
- Muscle weakness
- Fever and stiff neck
- Changes in mental status including signs of disorientation
- Recent fall or head injury
- A sudden or extremely severe headache
- Worsening headaches or headaches that do not respond to routine treatment
- History of cancer
Headache Symptoms that Could Indicate a Serious Underlying Disorder
Most headaches, such as tension-type headaches, are not serious or life-threatening. Headaches indicating a serious underlying problem, such as cerebrovascular disorder or malignant hypertension, are uncommon. (A headache without other neurological symptoms is not a common first symptom of a brain tumor.)
People with chronic headaches may, however, overlook a more serious condition believing it to be one of their usual headaches. You should immediately call your provider if your headache or other accompanying symptoms changes.
Be sure to call your provider, go to the emergency room, or call your local emergency number for any of the following symptoms:
- Sudden, severe headache that persists or increases in intensity over the following hours, sometimes accompanied by nausea, vomiting, or altered mental states (possible hemorrhagic stroke)
- Sudden, very severe headache, worse than any headache ever experienced (possible indication of hemorrhage or a ruptured aneurysm)
- Chronic or severe headaches that begin after age 50
- Headaches accompanied by other symptoms, such as memory loss, confusion, loss of balance, changes in speech or vision, or loss of strength in or numbness or tingling in arms or legs (possibility of stroke)
- Headaches after head injury, if drowsiness or nausea is present (possibility of hemorrhage)
- Headaches accompanied by fever, stiff neck, nausea, and vomiting (possibility of meningitis)
- Headaches that increase with coughing or straining (possibility of brain swelling)
- A throbbing pain around or behind the eyes or in the forehead accompanied by redness in the eye and perceptions of halos or rings around lights (possibility of acute glaucoma)
- A one-sided headache in the temple in elderly people; the artery in the temple may be firm and knotty and without a pulse; the scalp may be tender (possibility of temporal arteritis, which can cause blindness or stroke if not treated)
- Sudden onset and then persistent, throbbing pain around the eye that may spread to the ear or neck and is unrelieved by pain medication (possibility of blood clot in one of the sinus veins of the brain)
- New or changing headaches with a compromised immune system (such as from cancer or HIV)
Treatment
Management of tension-type headaches focuses in the short term on treating attacks, and in the long term on preventing recurrence. In general, short-term treatment of tension-type headache involves drugs (mainly pain relievers) while long-term preventive measures include both drug and non-drug approaches. With medications, relaxation training, lifestyle changes, and other therapies, most headache pain can be relieved or reduced.
Treatment for Episodic Tension-Type Headaches
Most episodic attacks of tension-type headaches get better without any treatment. Simple over-the-counter pain relievers such as acetaminophen (Tylenol, generic) or non-steroidal anti-inflammatory drugs (NSAIDs) can treat mild symptoms. Aspirin or ibuprofen (Advil, generic) are usually the first NSAID choices, followed by naproxen (Aleve, generic).
Some people may also try medications that combine a pain reliever with caffeine. However, using combination medications that contain caffeine more than twice per week may cause rebound headache.
Some people find massage therapy helpful for treating acute episodes of tension-type headache.
Preventive Treatment for Chronic Tension-Type Headaches
Daily preventive treatment is recommended for people who experience at least 2 headache attacks a month. Preventive treatments do not work as well when people overuse pain-relief medication. Your provider may recommend stopping and withdrawing from painkillers before beginning preventive approaches.
The goals of preventive treatment are to reduce the frequency and severity of headache attacks, and to improve the response to pain medication.
Prevention of tension-type headache includes:
- Drug treatment with an antidepressant, usually the tricyclic antidepressant amitriptyline
- Relaxation training and biofeedback
- Stress management through cognitive-behavioral therapy
- Lifestyle modifications
Studies indicate that best results are achieved when drug treatment is combined with relaxation or stress-management training.
Withdrawing from Medications after Medication-Overuse Headaches
If your headaches develop because of medication overuse, you will need to stop taking the drug. (If caffeine is the trigger, you may only need to reduce your coffee, tea, or soft-drink intake.)
A person usually has the option of stopping abruptly or gradually, and should expect the following course:
- Most headache drugs can be stopped abruptly, but be sure to check first with your provider. Certain non-headache medications, such as anti-seizure drugs, as well as some anti-anxiety drugs or beta-blockers, require gradual withdrawal under medical supervision.
- If you choose to taper off standard headache medications, withdrawal should be completed within 3 days or less.
- No matter which approach is used for stopping medication, there may be a period of worsening headache for a few days afterward. Alternative pain relievers may be administered during the first days to help withdrawal.
- Most people feel better within 2 weeks, although in some cases headache symptoms can persist up to 16 weeks (and in rare cases even longer).
Medications
The standard treatments for episodic attacks of tension-type headaches are NSAIDs, such as aspirin and ibuprofen. The tricyclic antidepressant amitriptyline (Elavil, generic) is considered the most effective preventive medication for treating chronic tension-type headaches.
Due to the risks of overuse and dependence, opioids, opioid-like drugs, and sedative hypnotics are not recommended for treatment of tension-type headaches.
Pain Relievers
Pain relief medication is helpful for treating mild-to-moderate headaches. However, it cannot prevent headaches. There are many different types of pain relief medicine.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs block prostaglandins, substances that dilate blood vessels and cause inflammation and pain. NSAIDs are usually the first drugs tried for almost any kind of headache. There are dozens of NSAIDs. Common NSAIDs include:
- Over-the-counter NSAIDs: Aspirin, ibuprofen (Advil, generic), naproxen (Aleve, generic), ketoprofen (Nexcede, generic)
- Prescription NSAIDs: Diclofenac (Cataflam, generic), tolmetin (Tolectin, generic), indomethacin (Indocin, generic)
Long-term use of high-dose NSAIDs may increase the risk for stomach bleeding and heart problems, including heart attack and stroke. Using NSAIDs more than twice a week may increase the risk for medication overuse (rebound) headache.
Acetaminophen
Acetaminophen (Tylenol, generic) is a good alternative to NSAIDs when stomach distress, ulcers, or allergic reactions prohibit their use. A high dose (1,000 mg) is recommended for treating headaches.
Acetaminophen does have some adverse effects, and the daily dose should not exceed 3 grams (3,000 mg). People who take high doses of this drug for long periods are at risk for liver damage, particularly if they drink alcohol and do not eat regularly. Acetaminophen may cause serious kidney problems in people who already have kidney disease. It also may interact with certain medications, including the blood thinner warfarin (Coumadin, generic).
Tricyclics and Other Antidepressants
Tricyclics are the type of antidepressant most often used for prevention of severe chronic tension-type headaches.
Tricyclic Antidepressants
Tricyclics are used to treat depression but they can also help relieve muscle pain and improve sleep. Amitriptyline (Elavil, generic) is the tricyclic most commonly prescribed for prevention of tension-type headache. Nortriptyline (Pamelor, generic) and Imipramine (Tofranil, generic) are other tricyclics sometimes prescribed.
A tricyclic antidepressant is usually started at a lower dose and then slowly increased. A headache diary can help you and your provider evaluate the effectiveness of the treatment. In general, people should remain on preventive drug treatment for at least 6 months. After that time, your provider will slowly reduce the dose while continuing to monitor the frequency of headache attacks.
Side effects are fairly common with these medications. Drowsiness is the most common side effect and may be better tolerated when tricyclics are taken before sleep. Other side effects may include dry mouth, constipation, blurred vision, sexual dysfunction, weight gain, trouble urinating, heart rhythm problems, and dizziness. Blood pressure may drop suddenly when sitting up or standing.
Tricyclics can have serious, although rare, side effects, including heart rhythm problems, which can be dangerous for people with certain heart diseases. These drugs can be fatal with overdose.
Other Antidepressants
Selective serotonin-reuptake inhibitors (SSRIs) work by increasing levels of serotonin in the brain. SSRIs used for prevention of tension-type headache include fluoxetine (Prozac, generic). Other antidepressants used for tension-type headache are mirtazapine (Remeron, generic), duloxetine (Cymbalta), and venlafaxine (Effexor, generic), which target both serotonin and norepinephrine.
Although these antidepressants have fewer side effects than tricyclics, they do not appear to work as well for prevention of tension-type headaches.
Other Drugs
Muscle relaxants
Tizanidine (Zanaflex, generic) is a muscle relaxant that is sometimes used for prevention of chronic tension-type headaches. In general, there is little evidence that other muscle relaxers are effective in treating tension-type headaches.
Anticonvulsants
Anti-seizure drugs, which are used for treating epilepsy, are sometimes used for prevention of tension-type headaches. They include topiramate (Topamax, generic), valproic acid (Depakote), and gabapentin (Neurontin, generic). When taken during pregnancy, anti-seizure medications increase the risk of birth defects, and may not be suitable in young women of child-bearing potential.
Investigational Drugs
Botulinum Toxin
Botulinum toxin (such as onabotulinumtoxin A, Botox) injections are used to relax muscles and reduce skin wrinkles. Botulinum toxin injections are FDA-approved for prevention of chronic migraines in adults. However, the FDA has not approved these drugs for treatment of tension-type headaches. While studies show conflicting evidence regarding the effectiveness of botulinum toxin for treating tension-type headache, a systematic review suggests botulinum injections may be effective.
Nitric Oxide Synthase Inhibitors
Nitric oxide synthase inhibitors block nitric oxide, which may play a role in increasing nerve activity and in vasodilation that leads to headache. Researchers are studying these drugs for treatment of tension-type headaches.
Lifestyle Changes
Psychological and behavioral techniques, and lifestyle changes, help reduce the intensity and frequency of tension-type headaches. These therapies can also enhance the effects of drug treatments. To date, relaxation training and biofeedback have the strongest evidence for improving tension-type headaches.
Relaxation Training and Biofeedback
Relaxation training uses breathing exercises, guided imagery, and other techniques to help relax muscles and relieve stress. Biofeedback uses a device to record a person's bodily responses (heart rate, surface skin temperature, and muscle tension). This information is then "fed back" to the person through a sound or visual image. Through this feedback, people learn to control their physical responses. In clinical studies, relaxation training and biofeedback, both alone and in combination, have led to improvements in tension-type headaches.
Cognitive Behavioral Therapy and Stress Management
Cognitive-behavioral therapy (CBT) teaches techniques to recognize and cope with life stressors. It can help people understand how thoughts and behavior patterns may affect their symptoms, and how to change the way the body responds to anticipated pain. CBT is often included in stress management techniques. Research indicates that CBT and stress management are most effective when combined with relaxation training or biofeedback.
Massage, Spinal Manipulation, and Physical Therapy
Massage can help relax tense muscles and may be helpful during acute headache episodes, however there is little evidence for long-term benefits. Although some small studies have suggested that spinal manipulation by chiropractors or osteopaths may be helpful for preventing tension-type headaches, there is insufficient evidence to confirm its effectiveness for reducing pain in tension-type headaches.
Evidence is somewhat stronger on the benefits of spinal manipulation for people with headaches originating from nerve or muscular problems in the neck. Some researchers believe that tension-type headaches relieved by spinal manipulation are probably caused by neck problems.
There has been little research on evaluating the benefits of physical therapy for tension-type headache. Sessions with a physical therapist might help in teaching specific exercises for strengthening and stretching muscles or improving posture. A physical therapist may also be able to advise on ergonomic changes for the workplace environment.
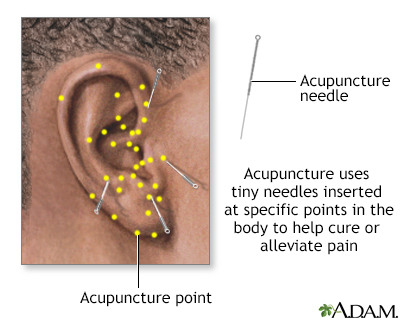
Acupuncture
Several reviews of clinical trials of acupuncture suggest that it may have some benefit for tension headaches.
Acupuncture, hypnosis and biofeedback are all alternative ways to control pain. Acupuncture involves the insertion of tiny sterile needles, slightly thicker than a human hair, at specific points on the body.
Diet and Exercise
Good health habits, including adequate sleep, adequate hydration, healthy diet, and regular exercise are helpful for reducing stress. Quitting smoking is important in reducing the risks for all types of headaches.
Home Remedies
Heat or cold packs may be helpful. Some people report more relief with cold, others with heat. Packs can either be frozen or heated.
Herbal and Other Natural Remedies
Numerous herbal remedies are promoted for tension-type headaches. It is important that anyone taking herbal or so-called natural remedies be aware of the lack of regulations on quality and effectiveness governing their marketing. Generally, manufacturers of herbal remedies and dietary supplements do not need approval from the FDA to sell their products.
Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. Always check with your provider before using any herbal remedies or dietary supplements. Never give herbal remedies or dietary supplements to children without first consulting the pediatrician.
Essential Oils
Some people find relief using 2 drops of peppermint, eucalyptus, or lavender oil added to 1 cup of water. Soak a cloth in the solution and apply it as a compress to the head.
Magnesium
Some studies suggest that magnesium supplements can help prevent migraine headache attacks, but there is little evidence that magnesium is helpful for tension-type headaches.
Herbs
Butterbur and feverfew are two popular herbal remedies for headache relief. The American Academy of Neurology deems butterbur as "effective" for migraine relief, and feverfew as "probably effective." It is not clear if these herbs are effective for tension-type headaches.
The following are special concerns for people taking these herbs:
- Butterbur can cause an allergic reaction in people who are sensitive to ragweed and related plants. It is not certain if butterbur is safe for use during pregnancy.
- Feverfew may be dangerous for people who have a bleeding or blood clot disorder, or who take blood-thinning medications such as warfarin (Coumadin, generic). Feverfew can interfere with these medications and can affect the time it takes blood to clot. Pregnant women or women hoping to become pregnant should not take this herb, as it may potentially harm the fetus.
Resources
- National Headache Foundation -- headaches.org
- American Migraine Foundation -- americanmigrainefoundation.org
- American Academy of Neurology -- www.aan.com
- National Institute of Neurological Disorders and Stroke -- www.ninds.nih.gov
References
Banzi R, Cusi C, Randazzo C, Sterzi R, Tedesco D, Moja L. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) for the prevention of tension-type headache in adults. Cochrane Database Syst Rev. 2015;(5):CD011681. PMID: 25931277 pubmed.ncbi.nlm.nih.gov/25931277.
Cerritelli F, Lacorte E, Ruffini N, Vanacore N. Osteopathy for primary headache patients: a systematic review. J Pain Res. 2017;10:601-611. PMID: 28352200 pubmed.ncbi.nlm.nih.gov/28352200.
Crawford P, Kim M. Acupuncture for frequent tension-type headaches. Am Fam Physician. 2016;94(3). PMID: 27479630 pubmed.ncbi.nlm.nih.gov/27479630.
Derry S, Wiffen PJ, Moore RA. Aspirin for acute treatment of episodic tension-type headache in adults. Cochrane Database Syst Rev. 2017;1:CD011888. PMID: 28084009 pubmed.ncbi.nlm.nih.gov/28084009.
Digre KB. Headaches and other head pain. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier Saunders; 2020:chap 370.
Freund B, Rao A. Efficacy of Botulinum Toxin in Tension-Type Headaches: A Systematic Review of the Literature. Pain Pract. 2019;19(5):541-551. PMID: 30742360 pubmed.ncbi.nlm.nih.gov/30742360.
Hershey AD, Kabbouche MA, O'Brien HL, Kacperski J. Headaches. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 613.
Garza I, Schwedt TJ, Robertson CE, Smith JH. Headache and other craniofacial pain. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice. 7th ed. Philadelphia, PA: Elsevier; 2016:chap 103.
Jackson JL, Mancuso JM, Nickoloff S, Bernstein R, Kay C. Tricyclic and tetracyclic antidepressants for the prevention of frequent episodic or chronic tension-type headache in adults: a systematic review and meta-analysis. J Gen Intern Med. 2017;32(12):1351-1358. PMID: 28721535 pubmed.ncbi.nlm.nih.gov/28721535.
Jay GW, Barkin RL. Primary Headache Disorders- Part 2: Tension-type headache and medication overuse headache. Dis Mon. 2017;63(12):342-367. PMID: 28886861 pubmed.ncbi.nlm.nih.gov/28886861.
Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016;4:CD007587. PMID: 27092807 pubmed.ncbi.nlm.nih.gov/27092807.
Probyn K, Bowers H, Caldwell F, et al. Prognostic factors for chronic headache: a systematic review. Neurology. 2017;89(3):291-301. PMID: 28615422 pubmed.ncbi.nlm.nih.gov/28615422.
Rizzoli P, Mullally WJ. Headache. Am J Med. 2018;131(1):17-24. PMID: 28939471 pubmed.ncbi.nlm.nih.gov/28939471.
Schuster NM, Rapoport AM. New strategies for the treatment and prevention of primary headache disorders. Nat Rev Neurol. 2016;12(11):635-650. PMID: 27786243 pubmed.ncbi.nlm.nih.gov/27786243.
Simpson DM, Hallett M, Ashman EJ, et al. Practice guideline update summary: botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016;86(19):1818-1826. PMID: 27164716 pubmed.ncbi.nlm.nih.gov/27164716.
Stephens G, Derry S, Moore RA. Paracetamol (acetaminophen) for acute treatment of episodic tension-type headache in adults. Cochrane Database Syst Rev. 2016;(6):CD011889. PMID: 27306653 pubmed.ncbi.nlm.nih.gov/27306653.
Voigt AW, Gould HJ 3rd. Chronic daily headache: mechanisms and principles of management. Curr Pain Headache Rep. 2016;20(2):10. PMID: 26780038 pubmed.ncbi.nlm.nih.gov/26780038.
Wieckiewicz M, Grychowska N, Zietek M, Wieckiewicz G, Smardz J. Evidence to Use Botulinum Toxin Injections in Tension-Type Headache Management: A Systematic Review. Toxins (Basel). 2017;9(11). pii: E370. PMID: 29140286 pubmed.ncbi.nlm.nih.gov/29140286.
Review Date: 3/31/2020
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.