Urinary incontinence
Loss of bladder control; Uncontrollable urination; Urination - uncontrollable; Incontinence - urinary; Overactive bladderUrinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries urine out of your body from your bladder. You may leak urine from time to time. Or, you may not be able to hold any urine. The three main types of urinary incontinence are:Stress incontinence --...
The Basics
Tests for bladder pelvic pain
A Closer Look
- Back pain and sciatica - InDepth (Detailed Report)
- Low back pain (Alternative Medicine)
- Urinary incontinence - InDepth (Detailed Report)
- Urinary tract infection - InDepth (Detailed Report)
- Urinary incontinence (Alternative Medicine)
- Prostatitis (Alternative Medicine)
- Benign prostatic hyperplasia - InDepth (Detailed Report)
Endometriosis - Animation
Endometriosis
Animation
Uterine fibroids - Animation
Uterine fibroids
Animation
Hysterectomy - Animation
Hysterectomy
Animation
Cervical cancer - Animation
Cervical cancer
Animation
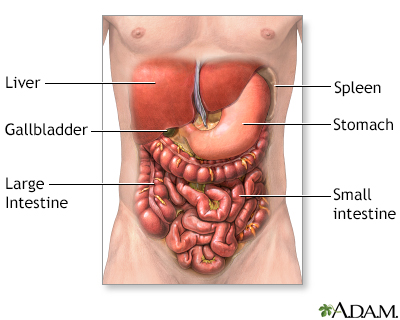
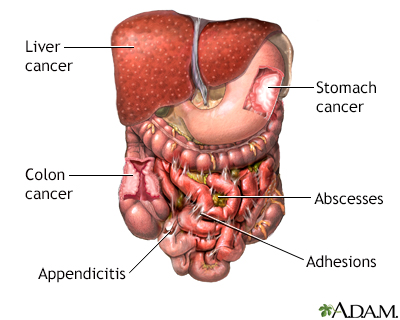
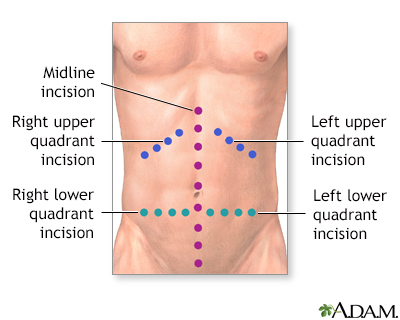
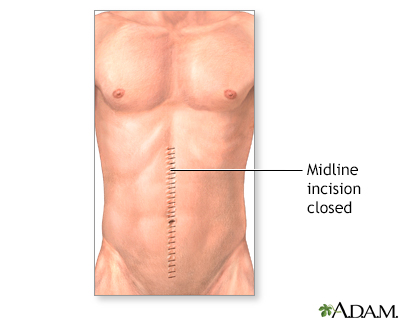
Abdominal exploration - series
Presentation
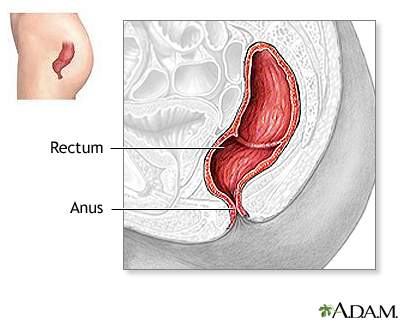
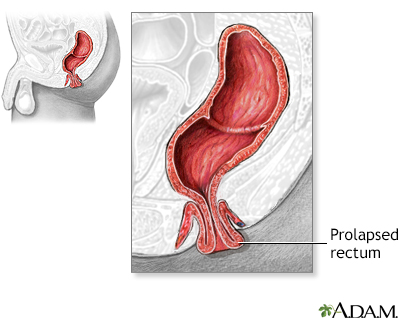
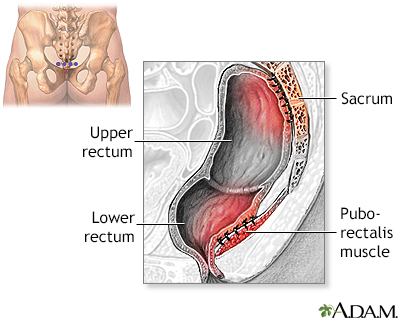
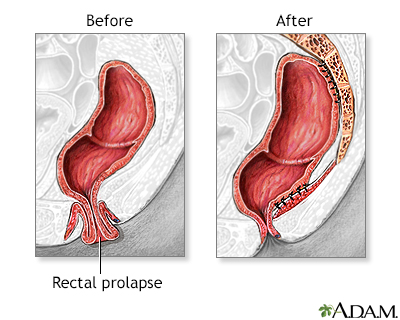
Rectal prolapse repair - series
Presentation
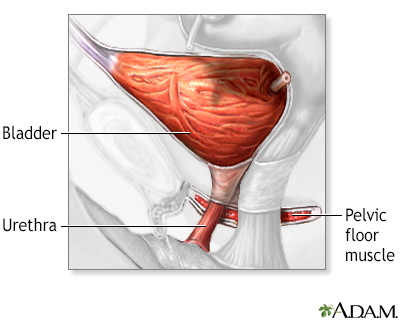
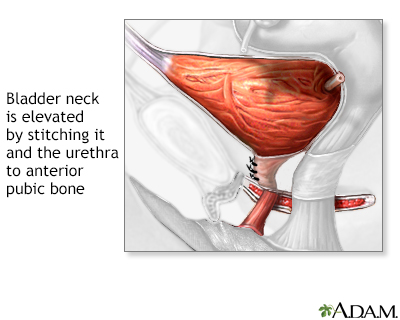
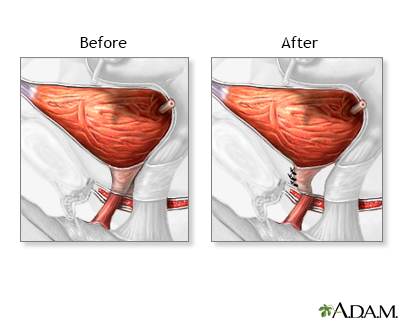
Bladder and urethral repair - series
Presentation
Endometriosis - Animation
Endometriosis
Animation
Uterine fibroids - Animation
Uterine fibroids
Animation
Hysterectomy - Animation
Hysterectomy
Animation
Cervical cancer - Animation
Cervical cancer
Animation
Urinary incontinence
Loss of bladder control; Uncontrollable urination; Urination - uncontrollable; Incontinence - urinary; Overactive bladderUrinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries urine out of your body from your bladder. You may leak urine from time to time. Or, you may not be able to hold any urine. The three main types of urinary incontinence are:Stress incontinence --...
The Basics
Tests for bladder pelvic pain
A Closer Look
- Back pain and sciatica - InDepth (Detailed Report)
- Low back pain (Alternative Medicine)
- Urinary incontinence - InDepth (Detailed Report)
- Urinary tract infection - InDepth (Detailed Report)
- Urinary incontinence (Alternative Medicine)
- Prostatitis (Alternative Medicine)
- Benign prostatic hyperplasia - InDepth (Detailed Report)
Urinary incontinence
Loss of bladder control; Uncontrollable urination; Urination - uncontrollable; Incontinence - urinary; Overactive bladderUrinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries urine out of your body from your bladder. You may leak urine from time to time. Or, you may not be able to hold any urine. The three main types of urinary incontinence are:Stress incontinence --...
The Basics
Tests for bladder pelvic pain
A Closer Look
- Back pain and sciatica - InDepth (Detailed Report)
- Low back pain (Alternative Medicine)
- Urinary incontinence - InDepth (Detailed Report)
- Urinary tract infection - InDepth (Detailed Report)
- Urinary incontinence (Alternative Medicine)
- Prostatitis (Alternative Medicine)
- Benign prostatic hyperplasia - InDepth (Detailed Report)
Review Date: 10/1/2024
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.